DSM V categorise these as seperate disorders
- Depressive disorders
- Bipolar disorders
- Anxiety disorders
Depressive Disorders
- Major depressive disorder
- Other depressive disorder
- Persistent Depressive Disorder
- Substance/medication induced depression disorder
- Depressive disorder due to another medical condition
Overview
Overview Depressive disorders are typically characterised by persistent low mood, loss of interest and enjoyment, neurovegetative disturbance, and reduced energy, causing varying levels of social and occupational dysfunction. Depression is the leading cause of disability and premature death in 18-44 yo and is predicated to be the 2nd leading cause of disability in 2020. 20% of adults will have it at some point in their life, women are twice as likely. Depression will make up ~5-10% of people seen in primary care setting.
| Definition Anhedonia: Loss of interest or pleasure in activities that were previously pleasurable Depression: Clinical Depression is an illness, a medical condition. It significantly affects the way someone feels, causing a persistent lowering of mood. Grief: Multifaceted response to loss, particularly to the loss of someone or something that has died, to which a bond or affection was formed. |
| Grief | Depression |
| There is an identifiable loss | A specific loss may or may not be identified |
| The person’s focus is on the loss | The person’s focus is on self |
| Fluctuating ability to feel pleasure | Inability to feel pleasure |
| Fluctuating physical symptoms | Prolonged and marked functional impairment |
| Closeness of others is usually comforting | Persistent isolation from other and self |
| Able to feel a wide range of emotions | Fixed emotions and feeling “stuck” |
| May express guilt over some aspects over loss | Generalised feelings of guilt |
| Thoughts of death are typically related to wanting to be reunited with the deceased loved one | Thoughts of death related to feeling worthless, undeserving of life or unable to cope with the pain |
Psychiatric Interview
Interview
History
- History of presenting Illness
- Medical history
- Medication history
- Drug and Alcohol
- Forensic History
- Social History
- Developmental history
- MSE
| Mini State Examination (MSE) | Findings in Depression |
| Appearence and Behaviour | Desheveled, furrowing of brows, ↓rate of blinking, shoulder bent, head down, ↓gesture, ↓eye contant |
| Speech | Slow, long pauses, little spontaneous speech, low volume |
| Mood and affect | Low mood/misery (worse in morning), pessimistic about the present, hopelessness about future, guilt about the past, suicidal, dysphoric, blunt affect |
| Thought form and though content | Delusions common (especially persecutory) |
| Cognition | ↓attention, concentration and memory |
| Insight | variable |
| Perception | reduced intensity of normal perceptions. Occasionally auditory hallucinations |
Mental State Examination (ABCDEFGHIJ)
- Appearence and Behaviours
- Cognition
- Delusion (Thought content)
- Emotion (mood and affect)
- Thought Form
- Gab (speech)
- Hallucinations and illusions (perception)
- Insight and Judgement
Risk Factors
| Risk Factors |
| Age (onset peaks in late 20s) |
| Family history (3x risk with affected 1° relatives) |
| Personal history |
| Lower SES |
| Substance abuse |
| Adverse life events |
| Lack of confiding relationship |
| Physical illness |
Signs and Symptoms
| Remember Mneumonic SIG-E-CAPS for the signs and symptoms of Depression. |
- Sleep changes
- Interest (decreased)
- Guilt (excessive)
- Energy (decreased)
- Concentration (decreased)
- Appetite changes
- Psychomotor agitation or retardation
- Suicidal ideation
Non-specific symptoms of Depression
- Abdominal pain
- Back pain
- Change in weight or appetite
- Constipation
- Fatigue
- Headache
- Insomnia or hypersomnia
- Joint pain
- Neck pain
- Weakness
Differential Diagnosis
- Bipolar Disorder
- Grief reaction
- Anxiety
- Hypothyroidism
- Multiple Sclerosis
- Dementia
- Other depressive disorder
- Persistent Depressive Disorder
- Substance/medication induced depression disorder (illicit drug withdrawal, antihypertensives, steroids)
- Depressive disorder due to another medical condition
| Remember Rule out an underlying substance (eg, alcohol and cocaine withdrawal), medication (eg, antihypertensives, steroids), or medical condition causing depression (eg, hypothyroidism, multiple sclerosis), especially if the patient does not have a prior history of depression. |
Investigations
- FBC (anaemia, infectious diseases)
- ESR
- EUC
- LFT
- Urinalysis – uraemia
- Thyroid function tests – hypothyroidism
- ECG – dysrhythmia -> cerebral infarct
Diagnosis
- 1 core symptom
- At least 4 associated symptoms (SIG-E-CAPS)
- Sleep changes
- Interest (decreased)
- Guilt (excessive)
- Energy (decreased)
- Concentration (decreased)
- Appetite changes
- Psychomotor agitation or retardation
- Suicidal ideation
Criteria for symptoms
- Pervasive (all day, most days)
- Persistent (2 weeks)
- Not better explained
- No manic or hypomanic episodes
- New signs and symptoms then normal that impact with daily function
Aetiology
Multifactorial
Changes in brain
- No structural abnormalities
- Function abnormalities present:
- Decreased activity in frontal lobe
- Increased firing in the limbic system
- Increase cortisol in blood
- Altered neurotransmitter pathways
- Serotonin
- Dopamine
- Noradrenaline
Management
| Remember The treatment that was successful for prior episodes of major depression has a higher likelihood of achieving remission in future episodes. |
Psychological therapy
- Cognitive behavioural therapy
- Interpersonal therapy
Psychosocial treatments are first line treatments for mild depression. Usually psychotherapy is used in conjunction with pharmacotherapy.
Pharmacological therapy
- SSRI (first line)
- Certraline
- SNRI
- Desvanlafaxine
- TCA
- Amytriptaline
- Other
- Mertazapine (safe in pregnancy)
None has been shown to be more effective then the other, so the choice depends on the adverse effects the patient can tolerate. SNRI are used first line because they generally have less side effects. When response to treatment is poor the diagnosis and compliance with treatment should be reassessed
| Think important to identify if patient also has manic episodes in the past, as antidepressent can induce a manic episode. |
| Remember Adults with major depressive disorder being treated with antidepressants should be observed for worsening depressed mood and suicidality, especially during the initial few months of a course of drug therapy, or at times of dose changes (either increases or decreases). |
| Pharmacology Selective serotonin reuptake inhibitors (SSRI) work by inhibiting the reuptake of serotonin from the synativ cleft thus increase serotonin effects on post synaptic neurons (causing good feels). Lower starting doses are often recommended and slowly increase and titrate accordingly. Side effects: Diarrhea, dizziness, dry mouth, fatigue, headache, sexual dysfunction, sweating, tremor, and weight gain are commonly reported. Nausea and vomiting are the most common reasons for discontinuation. Overdose of SSRI leads to serotonin syndrome (more info below). |
Moderate/severe depression:
- Electro Convulsive Therapy
- Transcranial Magnetic Stimulation
Complications and Prognosis
Complications
- Sexual dysfunction and Gastrointestinal disturbance of SSRIs and SNRIs
- Risk of self-injurious behaviour
- Undesired weight gain from antidepressant
| Remember Risk of suicide with SSRI (increase risk in young, risk decreases in old >25years). |
Prognosis
- Complete remission of symptoms and return to normal functioning are the therapy goals.
- For patients in their first episode of depression, treatment to remission may take up to several months and should be continued for a minimum of 9 to 12 months after remission.
- For patients who have had recurrent episodes, or in whom relapse or recurrence would likely convey a high risk, evidence supports prolonged antidepressant treatment.
| Remember More than 50% of patients who have had one episode of major depression will have recurrent episodes. |
Postpartum Depression
Overview Many experience what is known as postpartum blues, in which there is sadness, strong feelings of dependency, frequent crying spells, and dysphoria. This occurs in up to one in seven women.
Postpartum blues usually last for several days to a week. In rare cases, postpartum depression exceeds in both severity and length that is observed in postpartum blues and is characterized by suicidality and severely depressed feelings.
| Remember All women should be screened for depression during pregnancy and the postpartum period. |
Risk factors
- History of depression
- Family history
- Mental illness
- Recent stressful life events
- Poor social support
- Discontinuing pharmaceutical treatments
- Exposure to violence
Diagnosis –
Management
For first-time mothers, adolescent mothers, and mothers who have experienced a traumatic delivery, home health visits, telephone-based peer support, and psychotherapy may help prevent peripartum depression.
- Mild to moderate depression – psychotherapy or selective serotonin reuptake inhibitors (SSRI’s)
- Moderate to severe depression – combination of psychotherapy and medication (SSRI’s are the safest)
Serotonin Syndrome
| Think Selective serotonin reuptake inhibitors are the most commonly used medications for depression but should not be used in conjunction with MAOIs. One medication should be discontinued for at least 5 weeks before the other is initiated to avoid serotonin syndrome. |
Serotonin syndrome is characterized by (in order of appearance) diarrhea, restlessness, extreme agitation, hyperreflexia, autonomic instability, myoclonus, seizures, hyperthermia, rigidity, delirium, coma, and death.
Alternative Medicine
| Definition Alternative medicine – refers to therapies used in place of conventional care Complementary medicine – therapies used in conjunction with mainstream medical therapies. These therapies do not replace medical regimens for serious medical problems but are offered to support the patient and family. Examples: massage, support groups, guided imagery, biofeedback, and hypnosis Folk medicine – refers to therapies provided by family or group members as part of a family or cultural tradition. Examples: using “cold” foods for “hot” illnesses, religious or ritual healing practices Integrative medicine – refers to the integration of CAM therapies into mainstream medical practice based upon evidence of safety and effectiveness within the context of relationship-based care promoting optimal health and wellbeing. Holistic medicine – refers to the care of the whole patient (eg, body, mind, emotions, spirit, and relationships) in the context of his or her values, beliefs, culture, and community. Examples of holistic medicine include promotion of literacy, screening for depression or alcohol use in family members, assessment of spirituality, and promotion of housecleaning to reduce allergic symptoms. |
Classification of CAM
- Mind-body therapies
- meditation
- guided imagery
- relaxation
- hypnosis
- biofeedback
- prayer
- expressive therapies (dance, art, music)
- Biologically-based therapies
- botanicals
- animal-derived extracts
- vitamins
- minerals
- fatty acids
- amino acids
- proteins
- prebiotics and probiotics
- whole diets and functional foods
- Manipulative and body-based methods
- osteopathic manipulation
- chiropractic
- massage
- reflexology
- Energy therapies
- Examples of biofield therapies: qi gong, Reiki, Healing Touch and Therapeutic Touch
- Examples of bioelectromagnetic-based therapies: use of pulsed, magnetic and alternating-current or direct-current fields
- Whole medical systems
- Traditional Chinese Medicine (TCM; including acupuncture, Chinese herbs, tui na massage, tai chi, qi gong)
| Remember Patients and families may or may not discuss their use of CAM with their mainstream healthcare professionals, so it’s important to ask! |
CAM treatments used for depression
- St. John’s Wort (Hypericum Perforatum)
- Mechanism of action is unknown but may involve increasing synaptic availability of neurotransmitters such as serotonin
- Induction of CYP450 3A4 system, leading to clinically significant drug reactions with many conventional drugs via enhanced drug metabolism
- St. John’s wort has many drug interactions
- Serotonin syndrome may occur with concurrent use of antidepressants with serotonergic action, so avoid this combination
- Additional side effects: GI symptoms, dizziness/confusion, tiredness/sedation, photosensitivity, dry mouth, urinary frequency, anorgasmia, swelling
- Omega-3 fatty acids (EFAs)
- Polyunsaturated fatty acids integrated in multiple biological systems and considered essential nutrients for physical health
- S-Adenosyl-L-Methionine (SAMe)
- Mechanism of action unknown, but low SAMe levels have been reported in the CSF of depressed individuals, while higher plasma levels have been associated with a reduction in depressive symptoms
- Contraindication: Bipolar disorder, Pregnancy, Parkinson’s disease and if patient is immunocompromised
- Other CAMs
- Exercise
- Yoga
- Acupuncture
- Light therapy
- Sleep deprivation
| Cytochrome p450 system The liver is responsible for the selective uptake, concentration, metabolism and excretion of the majority of drugs and toxins that are introduced to the body. Exogenous products are hepatically metabolized predominantly through two mechanisms: phase I and phase II reactions. Phase I reaction transform lipophilic molecules into more polar, hydrophilic molecules via oxidation, reduction, or hydrolysis. Phase II reactions often but not always involves a monooxygenase system in which CYP450 plays a key role. Cytochrome P450 enzymes can be inhibited or induced by drugs, resulting in clinically significant drug-drug interactions that can cause unanticipated adverse reactions or therapeutic failures. Interactions with warfarin, antidepressants, antiepileptic drugs, and statins often involve the cytochrome P450 enzymes. |
Suicide
Overview Suicide is widespread across many age groups, and is associated with mental illness such as depression and other factors. Suicide is likely to be under-reported as deaths from suicide may be difficult to distinguish from accidental or intentional injury. It is important to note that suicide attempts are up to 20 times more frequent than completed suicide.
- In 2000, one million people worldwide died from suicide (1 death every 40 seconds)
- Suicide rates have increased by 60% worldwide in the last 45 years
- Suicide is one of the three leading causes of death among those aged 15-44 in both genders
| Side note Suicide among medical practitioners is higher than other professional groups in many industrialised countries, especially among female doctors. Risk factors for suicide are the same as the general population, however there is greater knowledge about how succeed and the availability of methods which may contribute to relatively high suicide rates. |
| Definition Mental illness: A term referring to a group of conditions that significant affect how a person feels, thinks, behaves, and interacts. Mentally disordered person: A person (whether or not suffering from mental illness) whose behavior for the time being is so irrational as to justify a conclusion on reasonable grounds that temporary care, treatment, or control of the person is necessary. |
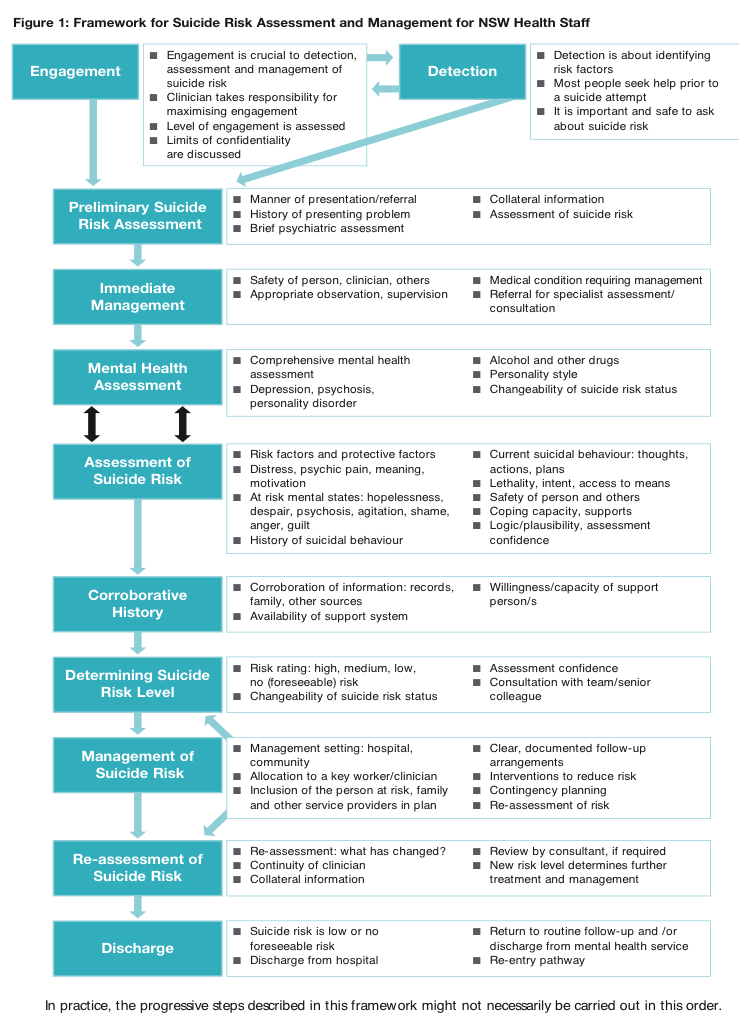
Suicide risk assessment – Important to complete when dealing with all patients who have mental health problems. The aim is to evaluate the likelihood of suicide attempt in the period of assessment.
Self-harm assessment (brief)
- Motivations
- At-risk mental states – Hopelessness, despair, psychosis, agitation, shame, anger, guilt
- Current suicidal behaviour – Thoughts, actions, plan
- Lethality, intent and access to means – Degree of determination, established plans, anticipated rescue, belief that they would die, finalization of personal business
- History of suicidal behavior or self harmSafety of person and others (homicidal intent)
-
- Coping capacity and supports
- Corroborative or collateral history – Records, family, other sources
- Potential triggers of presenting complaint
- Recent stressors
- Change in medications
- Change in social situations including relationships
- Major life events
| RISK FACTORS AND PROTECTIVE FACTORS OF SUICIDE | ||
| Groups at Risk of suicide | Risk Factors | Protective Factors |
| History of attempt or self-harm | Male | Strong perceived social supports |
| History of mental illness | Between 25-44yo | Family cohesion |
| History of sexual or physical abuse/neglect | Older people | Peer group affiliation |
| Domestic violence | Living in rural areas | Good coping and problem solving skills |
| Substance abuse | Recent break-up | Positive values and beliefs |
| Physical illness | Sexual identity conflicts | Ability to seek and access help |
| Refugees, immigrants | Financial difficulties | |
| Homeless | Impending legal prosecutions | |
| Lack of support |
Involuntary treatment
- Involuntary treatment must be reasonable, necessary, justified and proportionate
- The Doctor must have:
- Personally examinE or observed the person immediately or shortly before completing the certificate
- Formed the opinion that the person is either mentally ill or mentally disordered
- Is satisfied that involuntary admission and detention is necessary (and there are no less restrictive care reasonably available that is safe and effective)
- Is not the primary carer or a near relative of the person
Discharge following admission
- Patients who have been at risk of suicide need close follow-up when discharged






Discussion