Quotes
“I'm so good at beginnings, but in the end I always seem to destroy everything, including myself.”
― Kiera Van Gelder
“I need them to be aware and present with me in the midst of the storm, not just tell me what to do.”
― Kiera Van Gelder
Overview
Overview The term ‘personality disorder’ is frequently used in clinical practice to describe individuals with pervasive difficulties in interpersonal functioning, self-concept, emotional regulation and behaviour. Difficulties in personality functioning are potentially disabling conditions and are associated with significant distress and interpersonal difficulties.
Effects of personality
- Forms working opinions about ourselves
- A necessary element for relationship
- Allows us to adapt to the changes inherent in the life cycle
Characteristics of a “successful” personality
- Flexibility and Adaptability
- Emotional stability
- Reliability
- Likeability or attractiveness
| Definition Personality: pattern of perceiving, relating and beliefs about oneself and the environment as it is exhibited in actions in social, interpersonal and intrapersonal contexts Personality Disorder: Pattern of inner experience and behaviours not consistent with culture in two of the following: Cognition ( unusual ways of analysis of self, other, or events) Affect (range, intensity, lability and appropriateness) Interpersonal functioning Impulse control |
Psychiatric Interview
Interview
History
- History of presenting Illness
- Medical history
- Medication history
- Drug and Alcohol
- Forensic History
- Social History
- Developmental history
- MSE
Risk Factors
- History of abuse
- Family History of schizophrenia
- Negative parenting interactions
- Emotional/disruptive disorder in childhood
Types
Types of Personality Disorders
- Cluster A "MAD" - group of disorders characterised by odd and eccentric behavious
- Cluster B "BAD" - group of disorders characterised by dramatic, emotional and erratic behaviours
- Cluster C "SAD" - group of disorders characterised by anxious or fearful behaviours
| PERSONALITY DISORDER CLUSTERS | ||
| Cluster | Subtype | Key features |
| A. Odd/eccentric (MAD) | Paranoid | Suspcious |
| Schizoid | Sociall indifferent | |
| Schizotypal | Eccentric | |
| B. Dramatic/emotional (BAD) | Antisocial | Unempathic, callous |
| Borderline | Unstable identity | |
| Hisrionic | Attention-seeking | |
| Narcissisic | Self-centred, grandiose | |
| C. Anxious/fearful (SAD) | Avoidant | Inhibited |
| Dependent | Submissive, anxious | |
| Obsessive | Perfectionistic, rigid | |
| Classification of personality disorder | ||||
| Cluster A - Mad, Odd and eccentric | Schizoid: loner, detached, flat affect, restricted emotions | Schizotypal: odd, eccentric, magical thinking, paranoid | Paranoid: distrustful and suspicious | |
| Cluster B - Bad, dramatic and erratic | Histrionic: excessively emotional, attention-seeking | Narcissistic: self-important, needs admiration, lacks empathy | Antisocial: lacks empathy towards others. | Borderline: impulsive, unstable relationship, splitting (love then hate), attentionseeking |
| Cluster C Sad, anxious and timid | Obsessive-compulsive | Avoidant, Hypersensitive to criticism, socially uncomfortable, seeks out interpersonal relationships but with great discomfort | Dependent: submissive,clinging, needs to be taken care of | |
Signs and Symptoms
| Remember Persistence and pervasiveness is required in all the above criteria. |
- Paranoia
- Odd thinking
- Restricted range of emotions
- Anger and irritability
- Excessive emotionally and unstable mood stages
- Anxiety and tension
- Impulsive behaviours
- Grandiosity
- Evidence of self-harm
| Risk assessment in personality disorder |
| History of suicidal and self-harming behaviours and feelings |
| Triggers for self-harming behaviour |
| Degree of planning and intent |
| Chronic versus acute suicidal ideation |
| Available interpersonal support and responses elicited from carers/supports |
| Past intervention strategies and capacity to engage |
| Definition Self-harm/ self-injury: Refers to people deliberately hurting their bodies and is often done in secret without anyone else knowing. |
General criteria for personality disorder
The essential features of a personality disorder are
- An enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture. This pattern is manifested in 2 (or more) of the following areas
- Cognition (ways of perceiving and interpreting self, other people and events
- Affectivity (range, intensity, lability and appropriateness of emotional response)
- Interpersonal function
- Impulse control
- Enduring pattern is relatively inflexible and pervasive across a broad range of personal and social situations
- Enduring pattern leads to significant distress or impairment in social, occupational or other important areas of functioning
- Pattern is stable and of long duration, and its onset can be traced back at least to adolescence or early adulthood
- Enduring pattern is not better explained by another mental disorder
- Enduring pattern is not attributable to the physiological effects of a substance or another medical condition (eg. Severe head trauma)
- The impairments are not better understood as normal for an individual’s developmental stage or sociocultural environment.
Borderline Personality Disorder
Most common and most common to present is borderline personality Disorder. Borderline personality disorder is a severe mental disorder that has its onset during adolescence and emerging adulthood. It affects up to 3% of the population and occurs almost equally among males and females. Borderline personality disorder is Cluster B.
- Interpersonal (fear of abdomenet, spiltting)
- Image (attention-seeking)
- Impulssive
- Intense emotions
- Ideation (suicide, self harm)
Borderline personality disorder is a severe mental disorder that has its onset during adolescence and emerging adulthood. It affects up to 3% of the population. Borderline personality disorder are thought to result from the impact of trauma and neglect in early development on vulnerable individuals.
| Remember Borderline personality disorder is characterised by a pervasive pattern of instability in emotional regulation, interpersonal relationships and self-image, along with marked impulsivity. |
Course of Borderline Personality Disorder
- Onset occurs in adolescence or early adulthood.
- The most common pattern is one of chronic instability in early adulthoo
- The impairment from the disorder is greatest in young-adult years and gradually wane with advancing age.
- During the 30s and 40s, the majority of individuals attain greater stability in relationship and vocational functioning.
- After about 10 years many as half no longer have pattern of behavior meeting the full diagnostic criteria.
Treatment
| Remember Drugs should not be used as primary therapy for borderline personality disorder, because they have only modest and inconsistent effects, and do not change the nature and course of the disorder. |
- Dialectical behaviour therapy
- Mentalisation-based treatment
- Schema-focused therapy
- Cognitive behavioural therapy
- Cognitive analytic therapy
- Transference-focused therapy
- Systems training for emotional predictability and problem solving
- Dynamic deconstructive psychotherapy
| Dialectical Behavioral Therapy Integration of CBT with mindfulness, acceptance and techniques to tolerate stress and control emotions. It teaches skills to control intense emotions, reduce self-destructive behaviours and improve relationships. Four skill that are taught in DBT: 1. Mindfulness, Distress tolerance, interpersonal effectiveness and emotional regulation. |
Differential Diagnosis
- Mood Disorders
- Psychotic disorders
- Anxiety
- Substance related Disorders
Remember there are many types of personality disorder all with distinct features.
| PERSONALITY DISORDER CLUSTERS | ||
| Cluster | Subtype | Key features |
| A. Odd/eccentric (MAD) | Paranoid | Suspcious |
| Schizoid | Sociall indifferent | |
| Schizotypal | Eccentric | |
| B. Dramatic/emotional (BAD) | Antisocial | Unempathic, callous |
| Borderline | Unstable identity | |
| Hisrionic | Attention-seeking | |
| Narcissisic | Self-centred, grandiose | |
| C. Anxious/fearful (SAD) | Avoidant | Inhibited |
| Dependent | Submissive, anxious | |
| Obsessive | Perfectionistic, rigid | |
Management
General principles of management include consistency, reliability, encouraging autonomy, and the sensitive management of change
Non-pharmacological Management
- Hospitalisation or inpatient hospitalization referral - if self of harm or harm to others
- Cognitive behavioural therapy
- Substance abuse treatment program
Pharmacological Management (short-term)
- SSRI - for affective dysregulation, impulsive behaviour, depression and irrtability
- Mood stabilisers - for mood control and behavioural dysregulation
- lithium carbonate
- anticonvulsants - carbazepine
- Antipscyhotic - agitation, hostility and psychotic-like symptoms such as paranoid ideation and anxiety
| PERSONALITY DISORDER CLUSTERS | |||
| Cluster | Subtype | Therapy | Medication (usually short-term) |
| A. Odd/eccentric (MAD) | Paranoid | Reluctant to seek help. Referral for substance abuse if necessary | Low-dose antipsychotics |
| Schizoid | Low-dose antipsychotics | ||
| Schizotypal | Low-dose antipsychotics | ||
| B. Dramatic/emotional (BAD) | Antisocial | Contingency management treatment (a behavioural therapy where adaptive behaviours are rewarded | |
| Borderline | Alot discussed more at the borderline personality disorder section | ||
| Hisrionic | |||
| Narcissisic | |||
| C. Anxious/fearful (SAD) | Avoidant | CBT | |
| Dependent | Cognitive behavioural, psychodynamic, and social skills training, substance abuse therapy | ||
| Obsessive | Cognitive behavioural, psychodynamic, and social skills training, substance abuse therapy | ||
Prognosis
Consequences of personality disorders
| Remember All clusters worse under stress, especially interpersonal. |
- Failure to thrive in a psychological sense
- Difficulties in interpersonal relationships
- Failure to adapt to life’s many trials and tribulations
- Substance use
- Poor self-esteem → depression
- Reduced psychological coping skill → anxiety
| Side note Depression, anxiety, substance use, suicidal behaviour, and suicide are all more common in these patients; comorbid mental health problems are more difficult to treat and have poorer outcomes. |
Suicide
Overview Suicide is widespread across many age groups, and is associated with mental illness such as depression and other factors. Suicide is likely to be under-reported as deaths from suicide may be difficult to distinguish from accidental or intentional injury. It is important to note that suicide attempts are up to 20 times more frequent than completed suicide.
- In 2000, one million people worldwide died from suicide (1 death every 40 seconds)
- Suicide rates have increased by 60% worldwide in the last 45 years
- Suicide is one of the three leading causes of death among those aged 15-44 in both genders
| Side note Suicide among medical practitioners is higher than other professional groups in many industrialised countries, especially among female doctors. Risk factors for suicide are the same as the general population, however there is greater knowledge about how succeed and the availability of methods which may contribute to relatively high suicide rates. |
| Definition Mental illness: A term referring to a group of conditions that significant affect how a person feels, thinks, behaves, and interacts. Mentally disordered person: A person (whether or not suffering from mental illness) whose behavior for the time being is so irrational as to justify a conclusion on reasonable grounds that temporary care, treatment, or control of the person is necessary. |
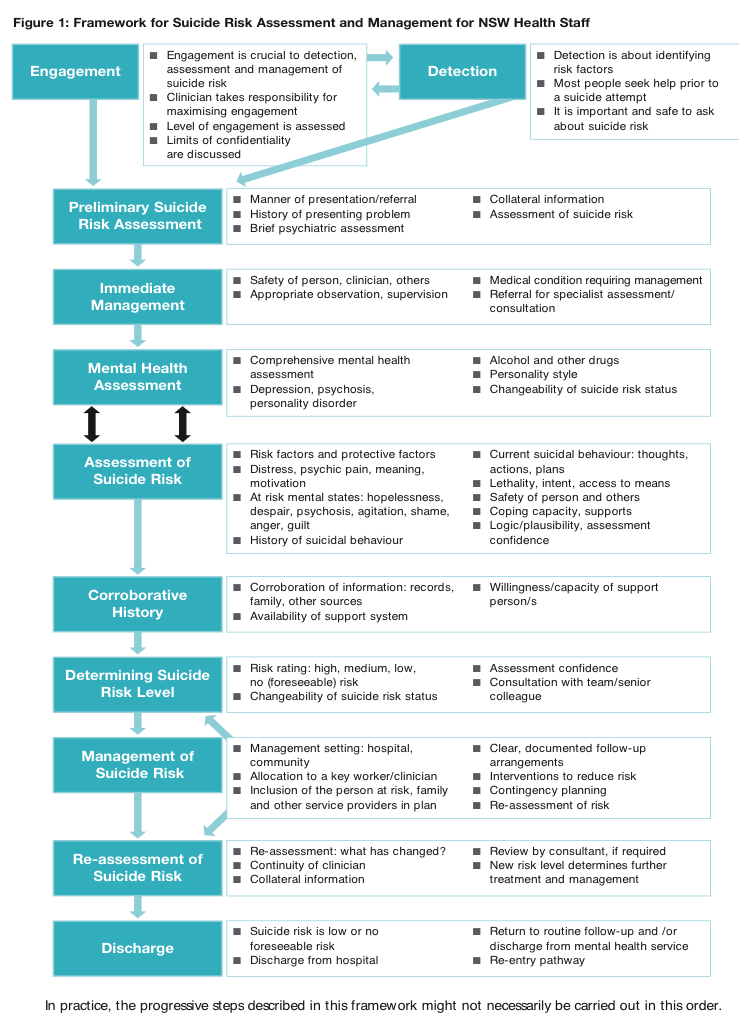
Suicide risk assessment – Important to complete when dealing with all patients who have mental health problems. The aim is to evaluate the likelihood of suicide attempt in the period of assessment.
Self-harm assessment (brief)
- Motivations
- At-risk mental states – Hopelessness, despair, psychosis, agitation, shame, anger, guilt
- Current suicidal behaviour – Thoughts, actions, plan
- Lethality, intent and access to means – Degree of determination, established plans, anticipated rescue, belief that they would die, finalization of personal business
- History of suicidal behavior or self harmSafety of person and others (homicidal intent)
-
- Coping capacity and supports
- Corroborative or collateral history – Records, family, other sources
- Potential triggers of presenting complaint
- Recent stressors
- Change in medications
- Change in social situations including relationships
- Major life events
| RISK FACTORS AND PROTECTIVE FACTORS OF SUICIDE | ||
| Groups at Risk of suicide | Risk Factors | Protective Factors |
| History of attempt or self-harm | Male | Strong perceived social supports |
| History of mental illness | Between 25-44yo | Family cohesion |
| History of sexual or physical abuse/neglect | Older people | Peer group affiliation |
| Domestic violence | Living in rural areas | Good coping and problem solving skills |
| Substance abuse | Recent break-up | Positive values and beliefs |
| Physical illness | Sexual identity conflicts | Ability to seek and access help |
| Refugees, immigrants | Financial difficulties | |
| Homeless | Impending legal prosecutions | |
| Lack of support |
Involuntary treatment
- Involuntary treatment must be reasonable, necessary, justified and proportionate
- The Doctor must have:
- Personally examinE or observed the person immediately or shortly before completing the certificate
- Formed the opinion that the person is either mentally ill or mentally disordered
- Is satisfied that involuntary admission and detention is necessary (and there are no less restrictive care reasonably available that is safe and effective)
- Is not the primary carer or a near relative of the person
Discharge following admission
- Patients who have been at risk of suicide need close follow-up when discharged
















