Overview
Osteomalacia (adults) and rickets (children) are disorders of impaired bone mineralisation leading to soft, poorly mineralised bone. It arises when there is insufficient calcium–phosphate supply to the mineralising matrix due to vitamin D deficiency, calcium deficiency, phosphate deficiency (often FGF23-mediated). Nutritional rickets still occurs worldwide, while hypophosphataemic forms (e.g., XLH, tumour-induced osteomalacia) are rarer but important. Major complications include growth failure and limb deformity in children, pseudofractures and fragility fractures in adults, bone pain, proximal myopathy, and impaired quality of life [1,3,8,11].
Definition
Osteoid: unmineralised organic bone matrix; excess osteoid with delayed mineralisation is the hallmark of osteomalacia (histomorphometry).
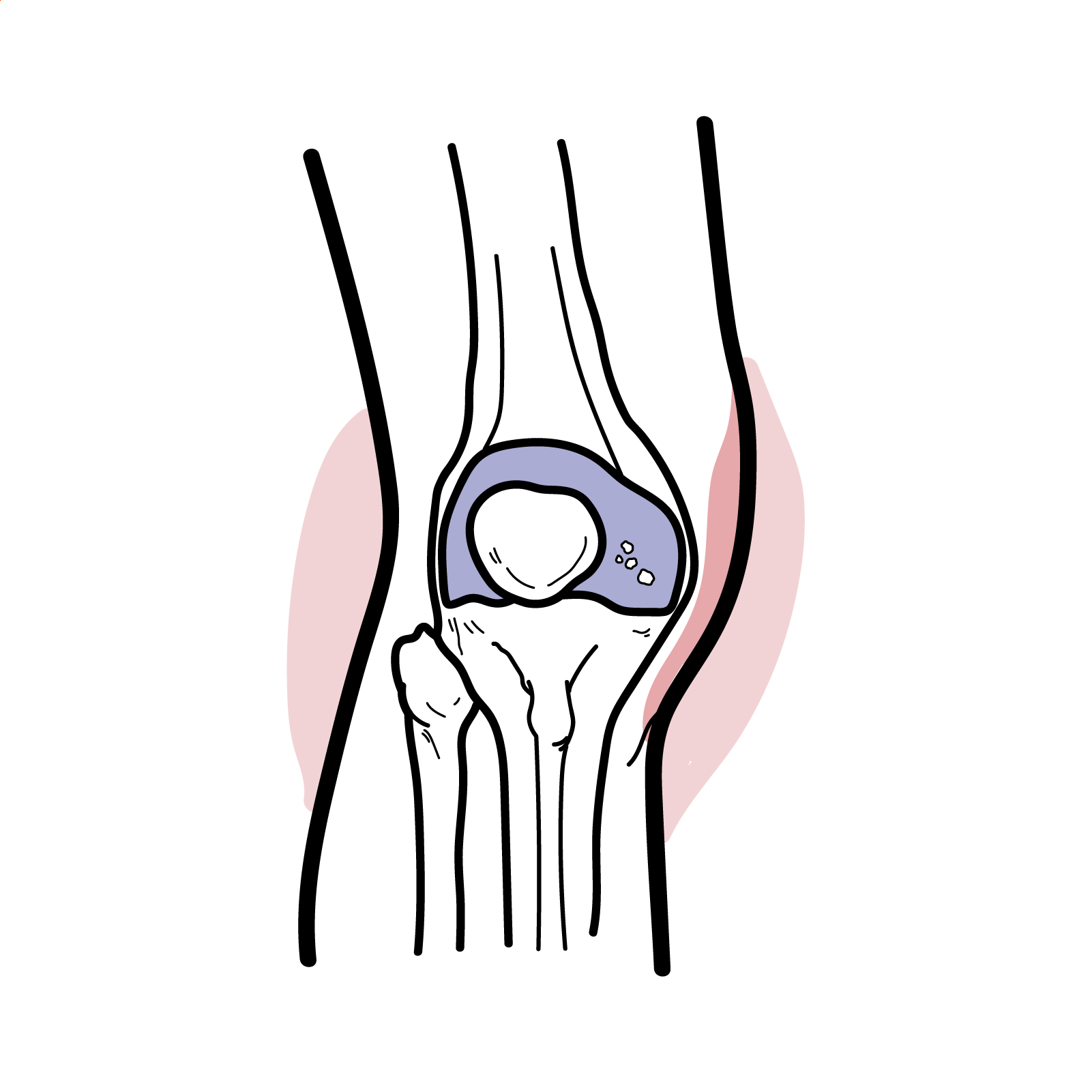
Looser zones (pseudofractures): transverse lucencies with sclerotic margins at sites of tensile stress (ribs, pubic rami, femoral neck) pathognomonic of osteomalacia.
FGF23: phosphaturic hormone that reduces renal phosphate reabsorption and 1α-hydroxylation of vitamin D; excess causes hypophosphataemic rickets/osteomalacia [3,8].
Rickets vs osteomalacia: rickets = defective mineralisation of growth plate cartilage in children; osteomalacia = defective mineralisation of bone matrix in all ages; in children rickets and osteomalacia usually coexist.
Anatomy & Physiology
- Bone remodelling units:
- osteoclasts resorb
- osteoblasts lay osteoid
- mineralisation requires adequate Ca2+×PO4 product and alkaline phosphatase activity.
- Vitamin D pathway: skin 7-dehydrocholesterol → cholecalciferol (UVB) → 25-OH-D (liver) → 1,25-(OH)2D (kidney via CYP27B1); 1,25-(OH)2D increases intestinal calcium and phosphate absorption and, with PTH, regulates bone turnover.
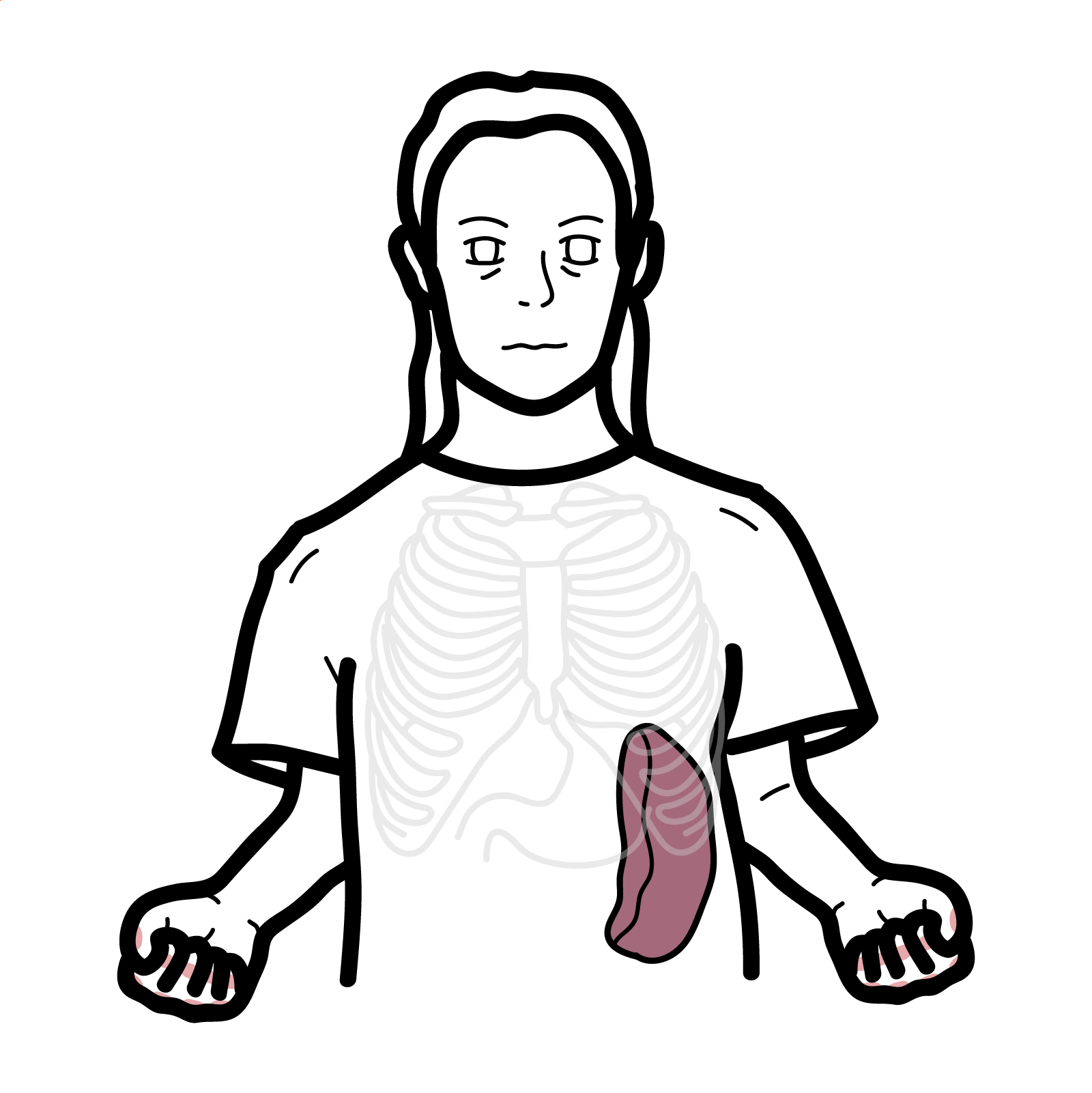
- Phosphate handling: ~80% reabsorbed in proximal tubule via NaPi2a/2c co-transporters; FGF23 (via Klotho) down-regulates these transporters and suppresses renal 1α-hydroxylase, lowering calcitriol [3,8].
- Calcium–phosphate homeostasis: PTH raises Ca2+ (bone resorption, renal Ca reabsorption) and lowers phosphate (phosphaturia); calcitriol raises both; FGF23 lowers phosphate and calcitriol.
Remember
A sustained fall in either intestinal supply (vitamin D/calcium) or renal phosphate reabsorption (FGF23 excess) prevents attainment of the Ca×PO4 ion product necessary for crystal deposition.
Aetiology and Risk Factors
Aetiology
- Nutritional deficiency: inadequate vitamin D intake/sunlight; dietary calcium deficiency
- Malabsorption: coeliac disease, IBD, pancreatic insufficiency, bariatric surgery
- Renal/hepatic disease: CKD (↓1α-hydroxylation, metabolic acidosis), Fanconi syndrome/renal tubular acidosis; cholestatic liver disease
- FGF23-mediated hypophosphataemia:
- X-linked hypophosphataemia (PHEX variants)
- Autosomal dominant hypophosphataemic rickets (FGF23 gain-of-function)
- Tumour-induced osteomalacia (phosphaturic mesenchymal tumours)
- FGF23-independent phosphate loss:
- HHRH (SLC34A3)
- Poorly controlled RTA
- Phosphate binders.
- Drugs: anticonvulsants (enzyme inducers), tenofovir, ifosfamide (Fanconi), anti-resorptives very rarely with severe vitamin D deficiency (hungry bone)
Risk factors
- Dark skin, veiling/covering, high latitude, winter season, indoor living; pregnancy/lactation; exclusive breastfeeding without maternal/infant supplementation
- Obesity, older age, malnutrition, vegetarian/vegan diets low in Ca/Vit D; chronic liver/renal disease; malabsorption/bariatric surgery; medications above
Think
In adults with diffuse bone pain + proximal weakness + low phosphate, ask about dental abscesses (In X-linked phosphataemia) and search for tumour induced osteomalacia (TIO).
Pathophysiology
- Insufficient calcitriol (↓25-OH-D substrate, ↓renal 1α-hydroxylase, or FGF23-mediated suppression) and/or renal phosphate wasting.
- ↓Intestinal calcium/phosphate absorption → fall in serum Ca2+/PO4.
- Secondary hyperparathyroidism (↑PTH) to maintain serum Ca2+ → ↑bone resorption, phosphaturia, ↑alkaline phosphatase; calcitriol remains low/normal (esp. in FGF23 excess)
- Failure to reach critical Ca×PO4 product in osteoid → delayed mineralisation → increased osteoid thickness and surface on histology
- In children, metaphyseal growth plate disorganisation (rickets).
- Mechanical stress on undermineralised bone → pseudofractures (Looser zones) and deformities
- Chronic hypophosphataemia → dental enamel/dentin defects and enthesopathy (XLH)
Remember
FGF23-mediated disease typically shows low/normal calcitriol despite hypophosphataemia—this separates it from simple vitamin D/calcium deficiency.
Clinical Manifestations
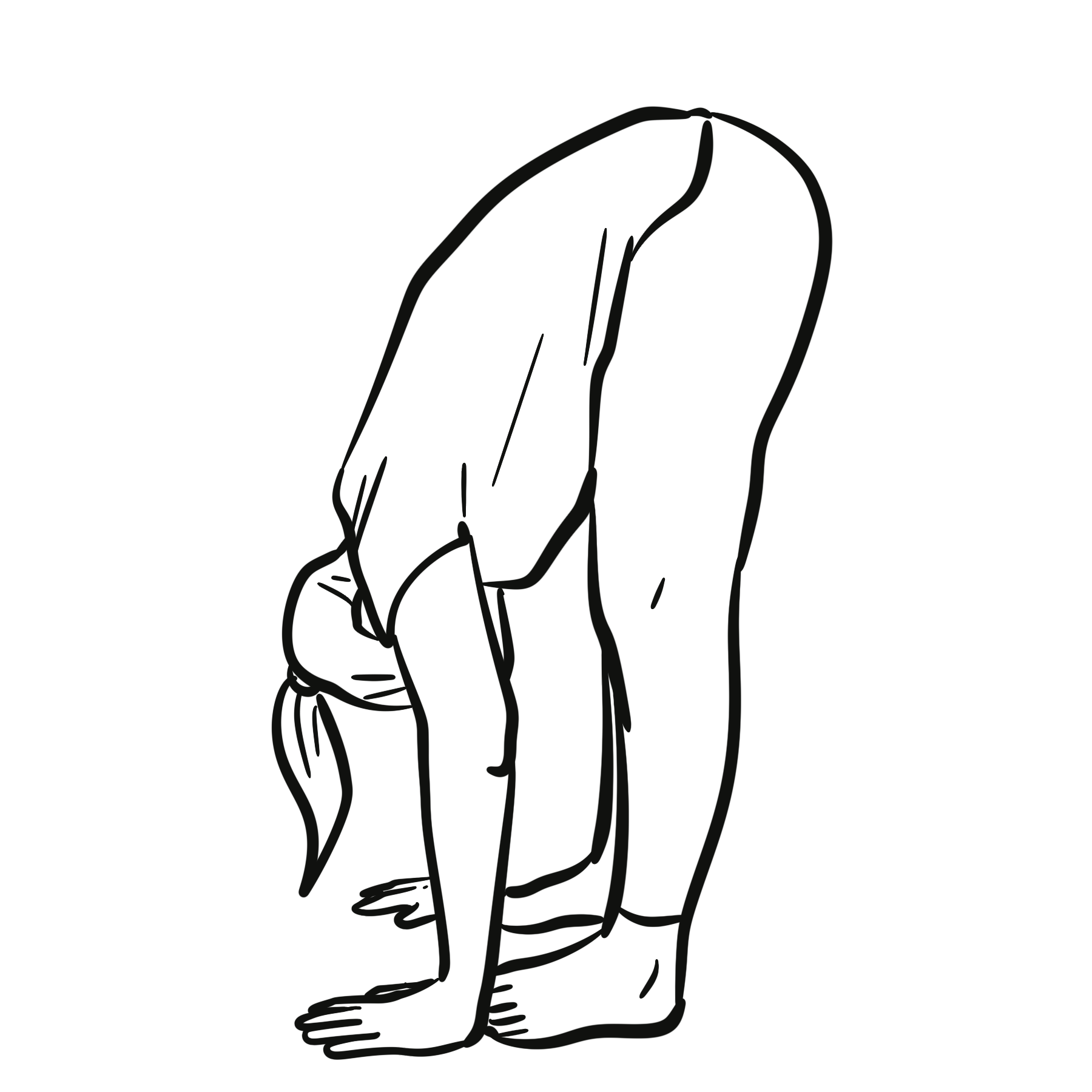
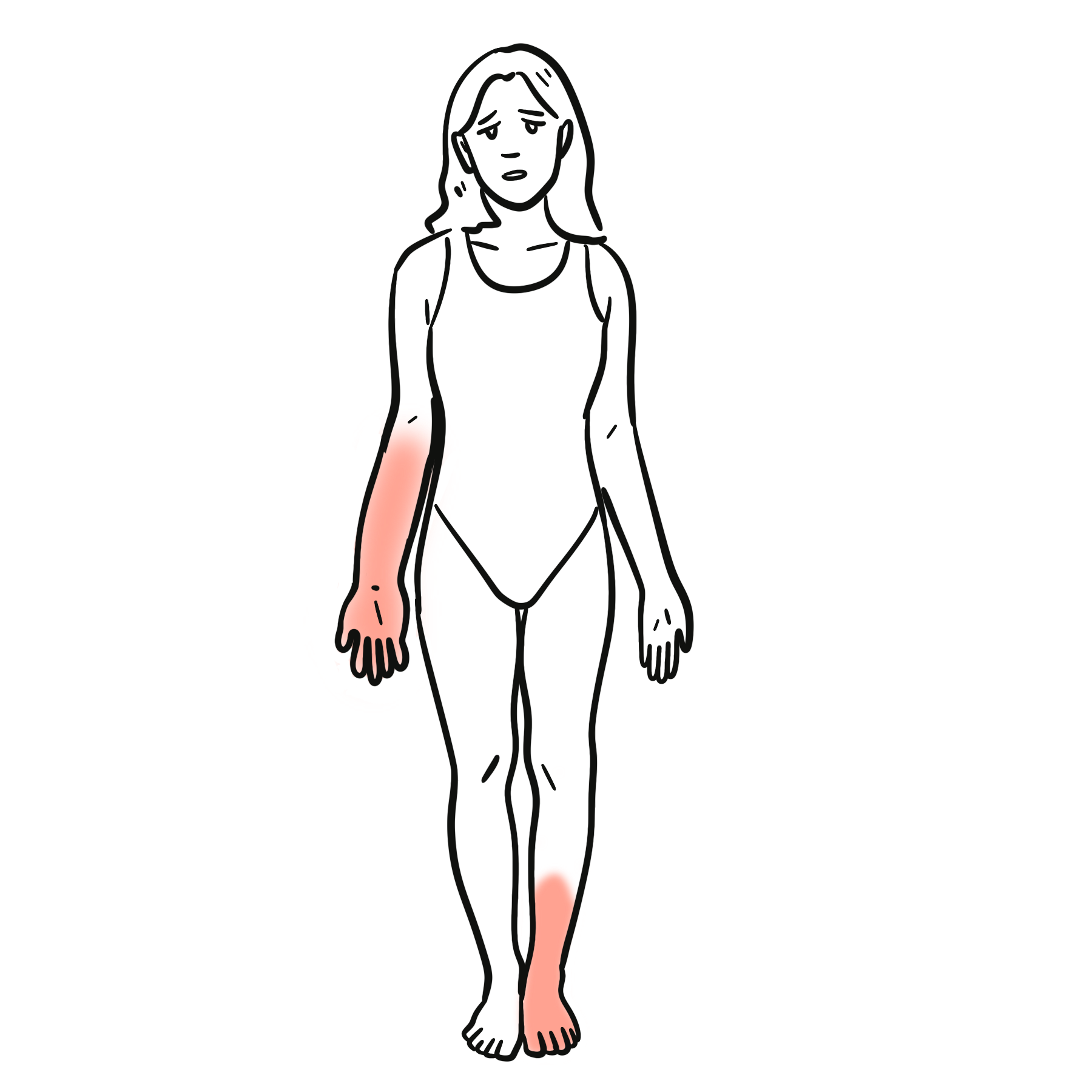
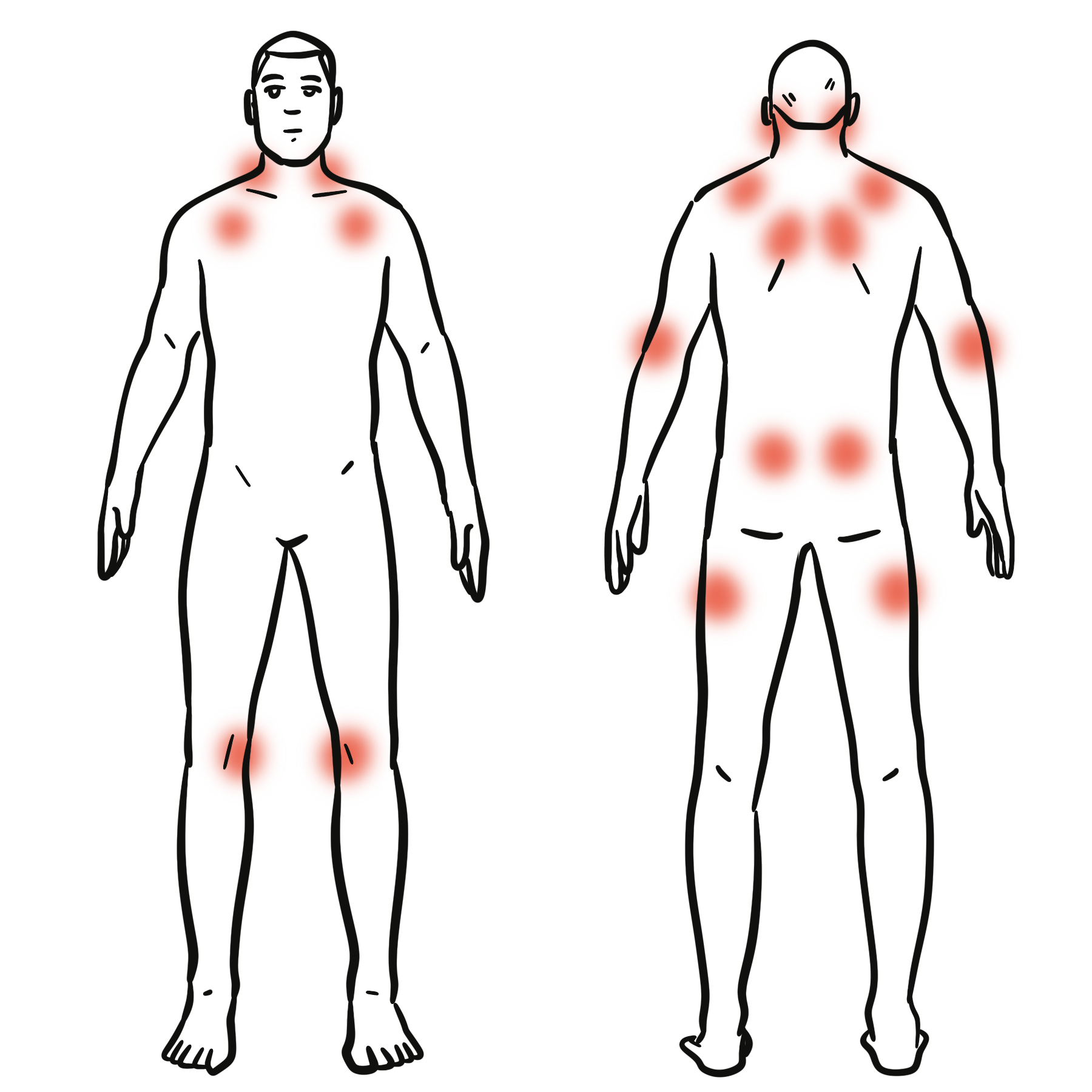
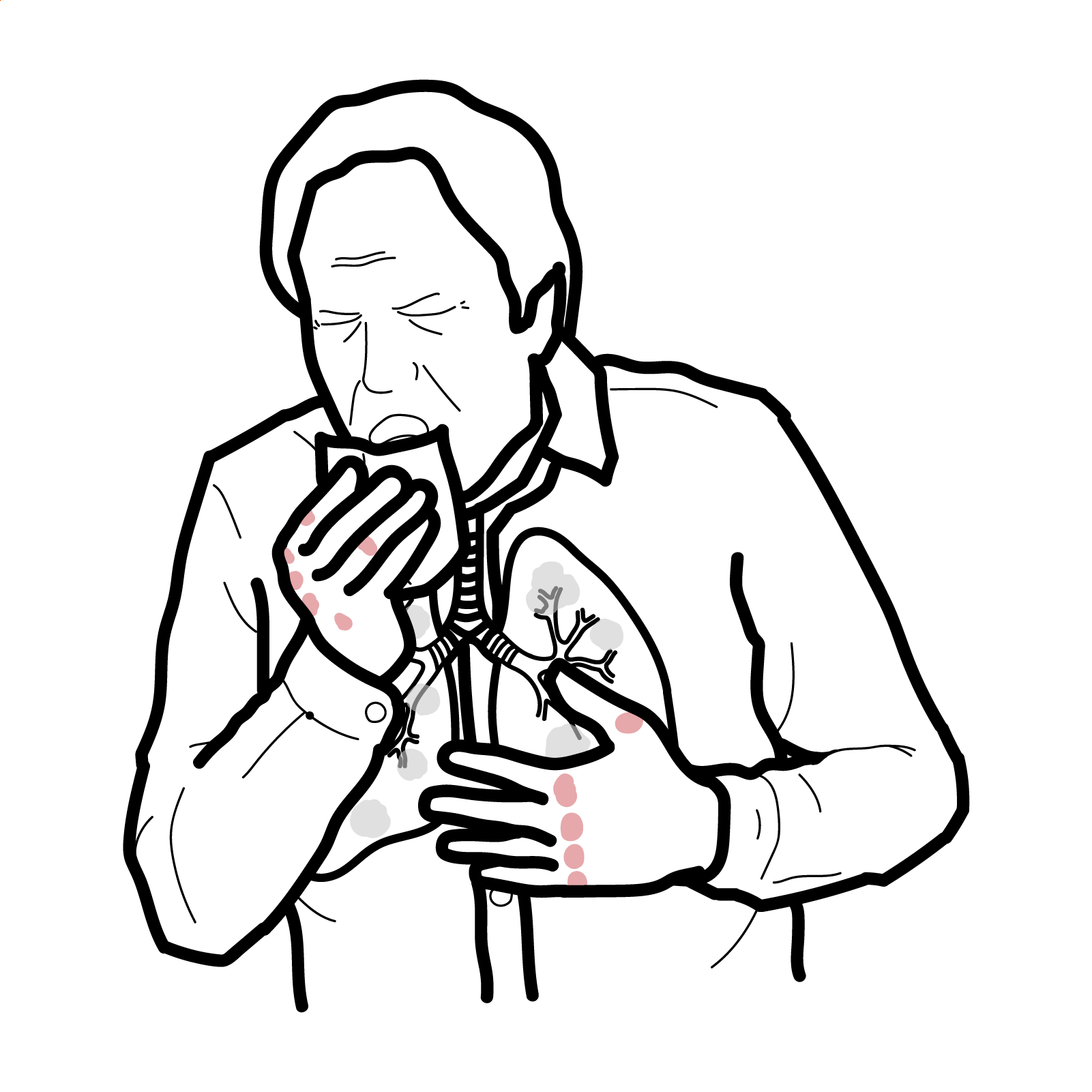
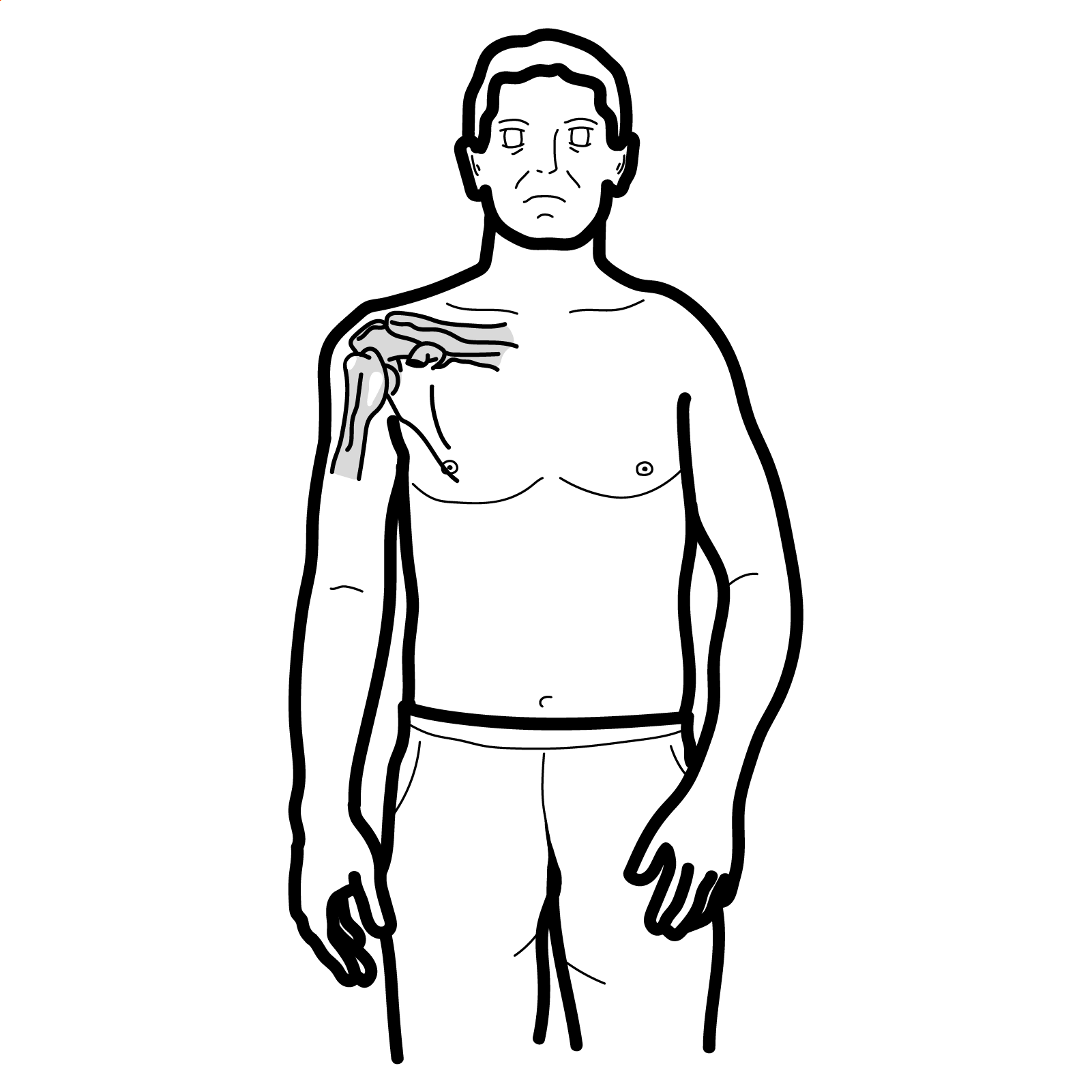
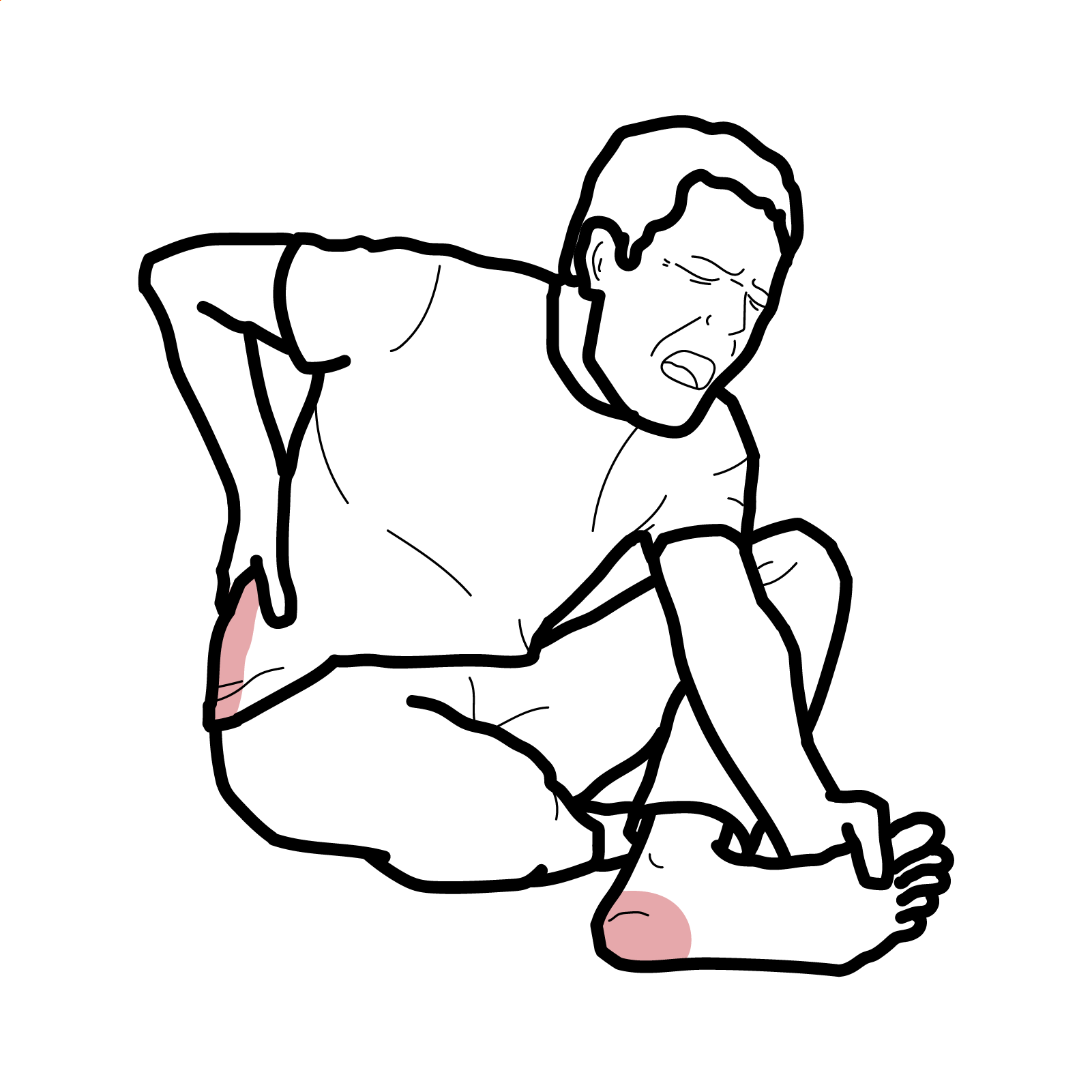
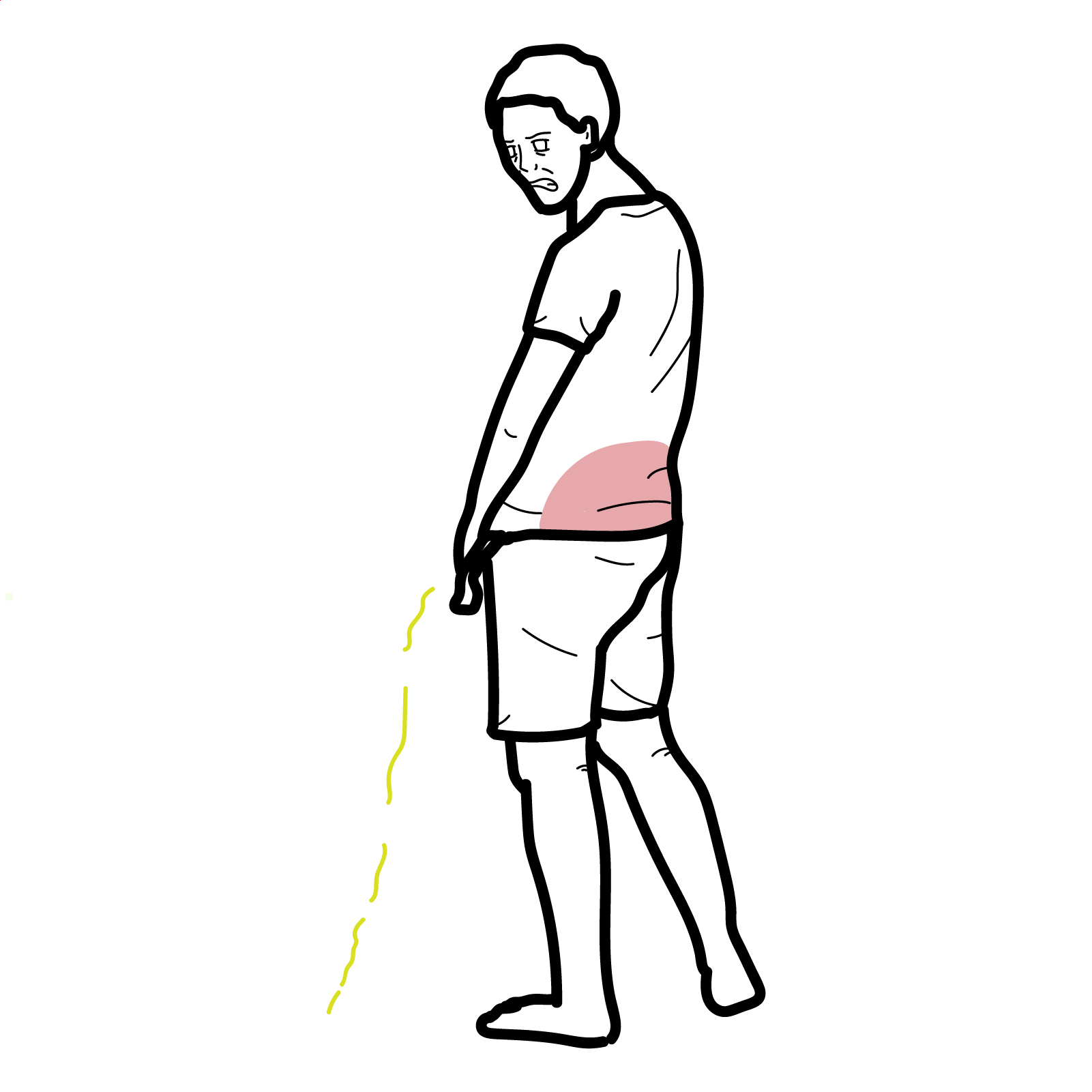
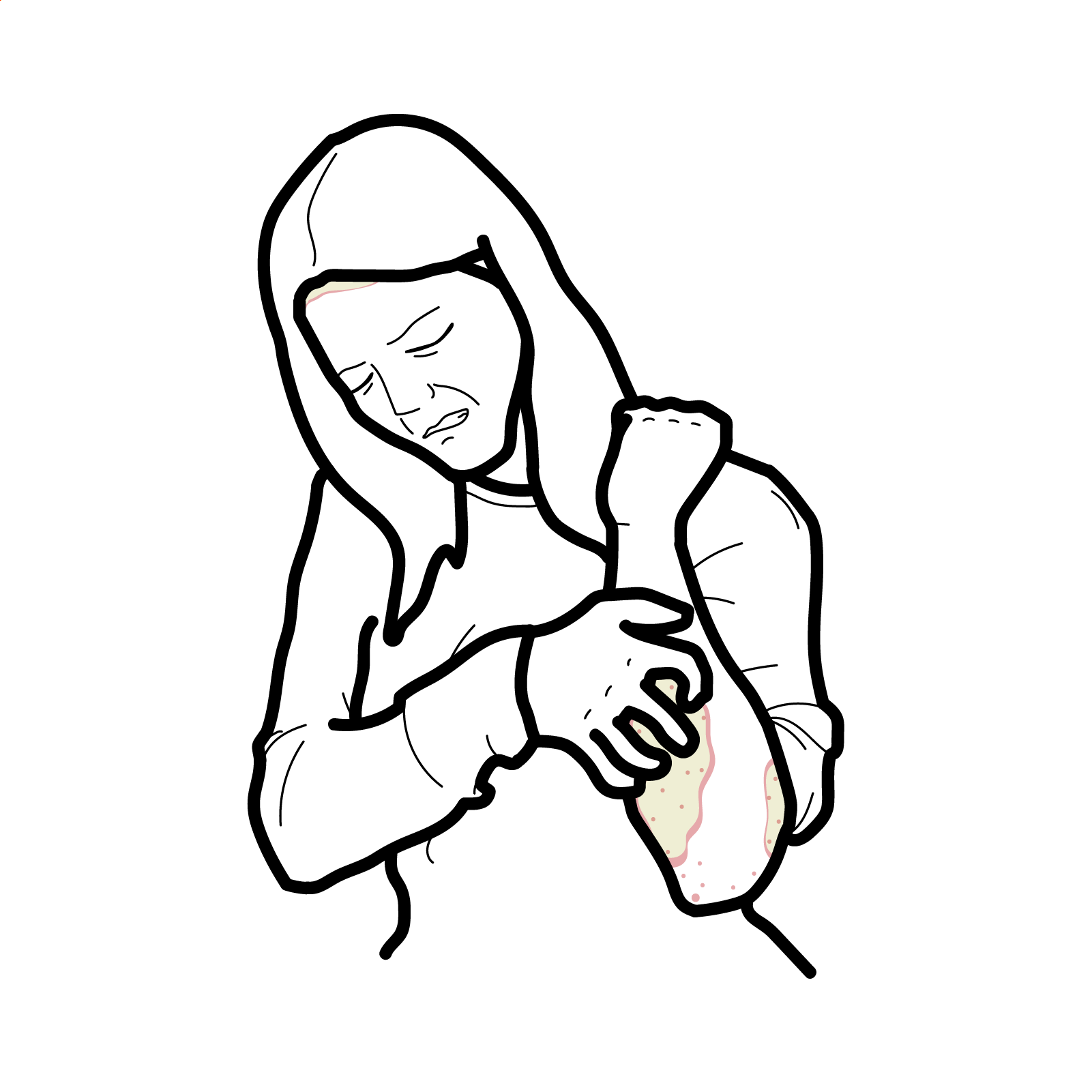
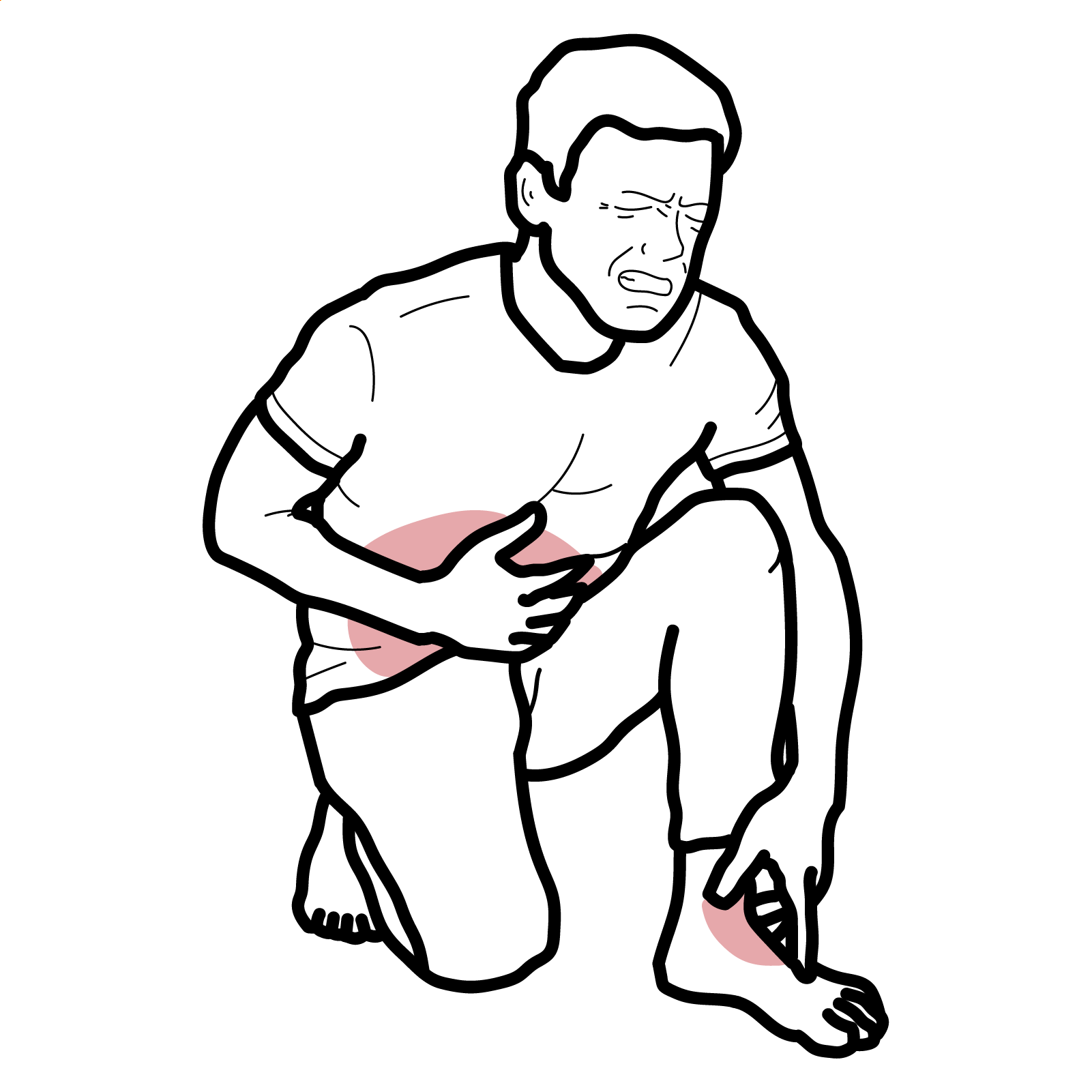
- Diffuse bone pain (pelvis, ribs, hips), fatigue, proximal myopathy (difficulty rising/climbing), waddling gait; height loss.
- Fractures: stress fractures/pseudofractures (Looser zones) at femoral neck, pubic rami, ulna, ribs; poor healing
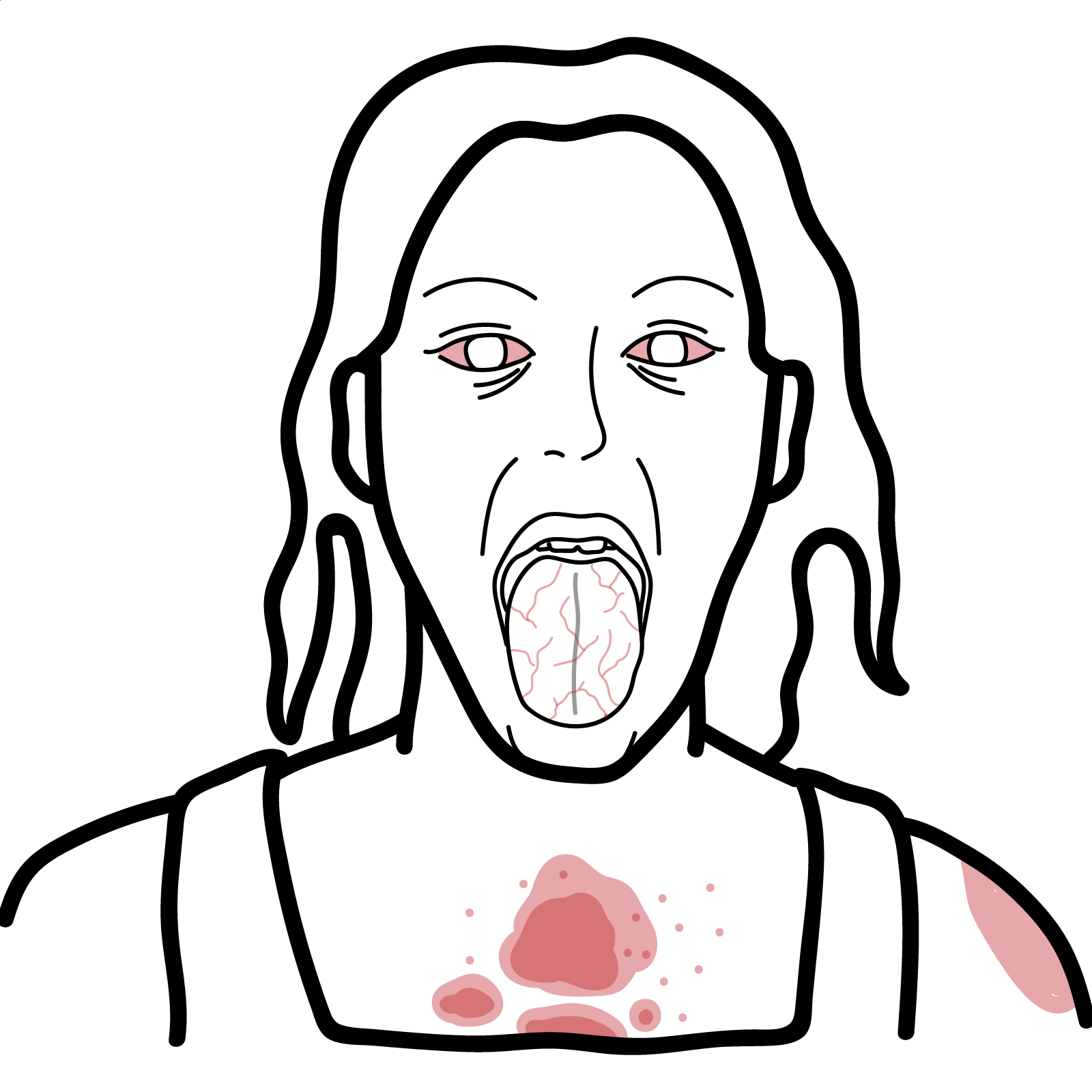
- Children (rickets): delayed growth, craniotabes, frontal bossing, widened wrists/ankles, rachitic rosary, Harrison sulcus, delayed motor milestones; limb deformity (genu varum/valgum).
- Hypophosphataemic forms: dental abscesses, enthesopathy, hearing loss, disproportionate lower-limb deformity; adults with TIO—severe bone pain, weakness, multiple insufficiency fractures
- Hypocalcaemia features (in severe deficiency): tetany, seizures, cardiomyopathy in infants.
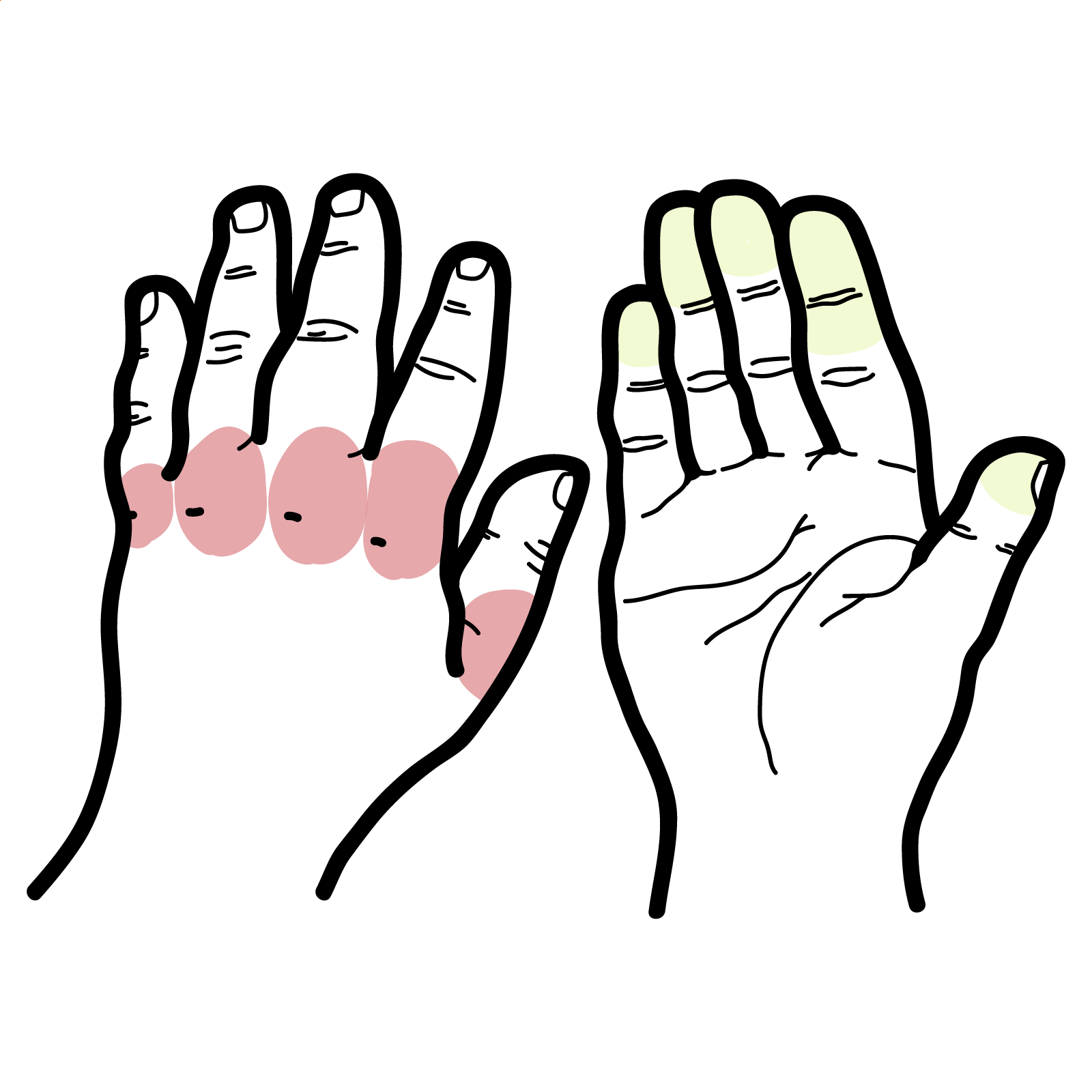
Clinical examination
- muscle weakness (hip flexors/abductors)
- antalgic/waddling gait
- bone tenderness
- in kids—widened metaphyses and deformities.
Diagnosis
- ↑ALP
- Vitamin D deficiency
- Hypocalcaemia and/or hypophosphataemia; ↑PTH (secondary hyperparathyroidism)
Imaging
- X-ray—Looser zones/pseudofractures; children—metaphyseal cupping/fraying, widened growth plates
- Bone densitometry: BMD may be low but nonspecific; do not confuse with osteoporosis
- Bone biopsy (rare/definitive): trans-iliac biopsy with double tetracycline labels shows ↑osteoid volume and prolonged mineralisation lag time; useful when diagnosis unclear or before treating suspected adynamic bone disease
Other
- In FGF23-mediated forms—low phosphate, high/normal FGF23, low/normal 1,25-(OH)2D, ↓TmP/GFR
- Tubular phosphate handling: calculate TmP/GFR; low in renal phosphate wasting (FGF23 excess, Fanconi).
- Search for cause: coeliac serology, renal panel, urinary phosphate/glucose (Fanconi), medication review; for Tumour induced osteomalacia—whole-body MRI or 68Ga-DOTATATE PET/CT to localise tumour
Think
Persistent low phosphate with normal calcium points strongly to FGF23 or renal tubular causes—check TmP/GFR and FGF23 early [2,3,8].
Differential Diagnosis
- Osteoporosis: normal mineralisation, low bone mass; ALP often normal; no Looser zones (DIF).
- Osteogenesis imperfecta: fracture history, blue sclerae, dentinogenesis imperfecta; genetic testing (DIF).
- Hyperparathyroidism: high Ca, low phosphate, subperiosteal resorption not Looser zones (DIF).
- Osteitis fibrosa/renal osteodystrophy: CKD context; PTH very high; bone biopsy pattern (DIF).
Treatment
- General principles: correct biochemical abnormalities, relieve pain and myopathy, heal fractures, and treat the cause
- Nutritional vitamin D deficiency (adults): cholecalciferol 3000–5000 IU daily or 50,000 IU weekly for 6–8 weeks, then maintenance 800–2000 IU/day; add elemental calcium 1–1.5 g/day if dietary intake low; monitor ALP, Ca, PO4, PTH at 8–12 weeks [11].
- Children (nutritional rickets): treat per Global Consensus—age-specific vitamin D and calcium dosing; ensure ongoing maintenance and prevention strategies
- Malabsorption/bariatric: higher/parental vitamin D dosing; treat underlying disease; ensure calcium and magnesium repletion [11].
- Hypophosphataemic forms (FGF23-mediated):
- XLH: first-line burosumab (anti-FGF23 mAb) improves phosphate, rickets severity, pain and physical function; alternative/legacy therapy = divided oral phosphate + active vitamin D (calcitriol/alfacalcidol) with monitoring for nephrocalcinosis
- Tumour-induced osteomalacia: localise and resect tumour (curative); if unresectable or occult, burosumab or phosphate + calcitriol therapy [2].
- Renal disease: treat CKD-MBD per nephrology guidance, active vitamin D analogues as indicated; correct acidosis.
- Pain/fractures: protected weight-bearing, physiotherapy for proximal weakness; manage fractures (often heal rapidly after repletion).
Remember
Avoid high-dose intermittent (“stoss”) vitamin D in infants/children unless per protocol; ongoing prevention via supplementation/fortification for high-risk groups is guideline-endorsed [1,12].
Think
Persistently high ALP after normalisation of 25-OH-D suggests unrecognised phosphate wasting—check phosphate and TmP/GFR.
Complications and Prognosis
Complications
- Children: permanent skeletal deformities (genu varum/valgum), short stature, dental enamel defects/abscesses, hypocalcaemic seizures, cardiomyopathy in severe cases
- Adults: recurrent insufficiency fractures/pseudofractures, chronic pain, proximal myopathy, falls, impaired function; nephrocalcinosis with phosphate-calcitriol therapy; kidney stones if overtreatment
Prognosis
- Nutritional deficiency: excellent with timely repletion; radiographic healing in months, strength improves over weeks; relapse without maintenance or if risk factors persist
- FGF23-mediated disease: better growth/function and pain with burosumab; poorer outcomes with delayed diagnosis, longstanding deformity, CKD, or unresectable TIO
- Poor prognostic factors: late presentation, persistent hypophosphataemia, severe deformity, coexistent CKD/malabsorption, inadequate adherence to supplementation
Table 1. Biochemical patterns (simplified)
| Pattern | Ca | PO4 | ALP | PTH | 25-OH-D | 1,25-(OH)2D | FGF23 | TmP/GFR | Likely mechanism |
| Nutritional Vit D deficiency | low/normal | low/normal | ↑ | ↑ | ↓ | low/normal | normal | normal | reduced calcitriol substrate |
| Calcium deficiency | low | low/normal | ↑ | ↑ | normal | ↑ | normal | normal | low calcium intake |
| XLH/TIO (FGF23-mediated) | normal | low | ↑ | normal/↑ | normal | low/normal | ↑ | low | renal phosphate wasting [3,8] |
| HHRH (FGF23-independent) | normal/high Ca | low | ↑ | low/normal | normal | ↑ | low | low | SLC34A3; hypercalciuria |
References
- Munns CF, Shaw N, Kiely M, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101(2):394-415. (Oxford Academic)
- Florenzano P, Hartley IR, Jimenez M, et al. Diagnosis and management of tumor-induced osteomalacia: Perspectives from clinical practice. J Endocr Soc. 2021;5(9):bvab099. (Oxford Academic)
- Carpenter TO, Whyte MP, Imel EA, et al. FGF23, hypophosphatemia, and emerging treatments. JBMR Plus. 2019;3(8):e10190. (Oxford Academic)
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30. (historical background)
- Shoback DM, Rosen CJ. Vitamin D for the prevention of disease: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2024;109(8):1907-1932. (Oxford Academic)
- Bhan A, Rao SD. Osteomalacia and vitamin D status: a clinical update. JBMR Plus. 2020;4(8):e10447. (Wiley Online Library)
- Takeuchi Y, Fukumoto S. FGF23-related hypophosphataemic rickets/osteomalacia: diagnosis and new treatment. J Mol Endocrinol. 2021;66(2):R57-R65. (jme.bioscientifica.com)
- Endocrine Society. Vitamin D for the Prevention of Disease Guideline page (summary). 2024. (Endocrine)
- ANZSPED copy of the Global Consensus PDF (for algorithms). 2016. (media.anzsped.org)



Discussion