Rheumatoid Arthritis
Rheumatoid arthritis is a common systemic inflammatory disease characterized by the presence of a destructive polyarthritis with a predisposition for affecting the small joints of the hands and feet and the wrists. Rheumatoid arthritis (RA) is the most common inflammatory arthritis, with a lifetime prevalence of up to 1 percent worldwide. Like many autoimmune diseases, the etiology of RA is multifactorial.
Arthritis: Inflammaed joint
Arthlagia: Pain in a joint
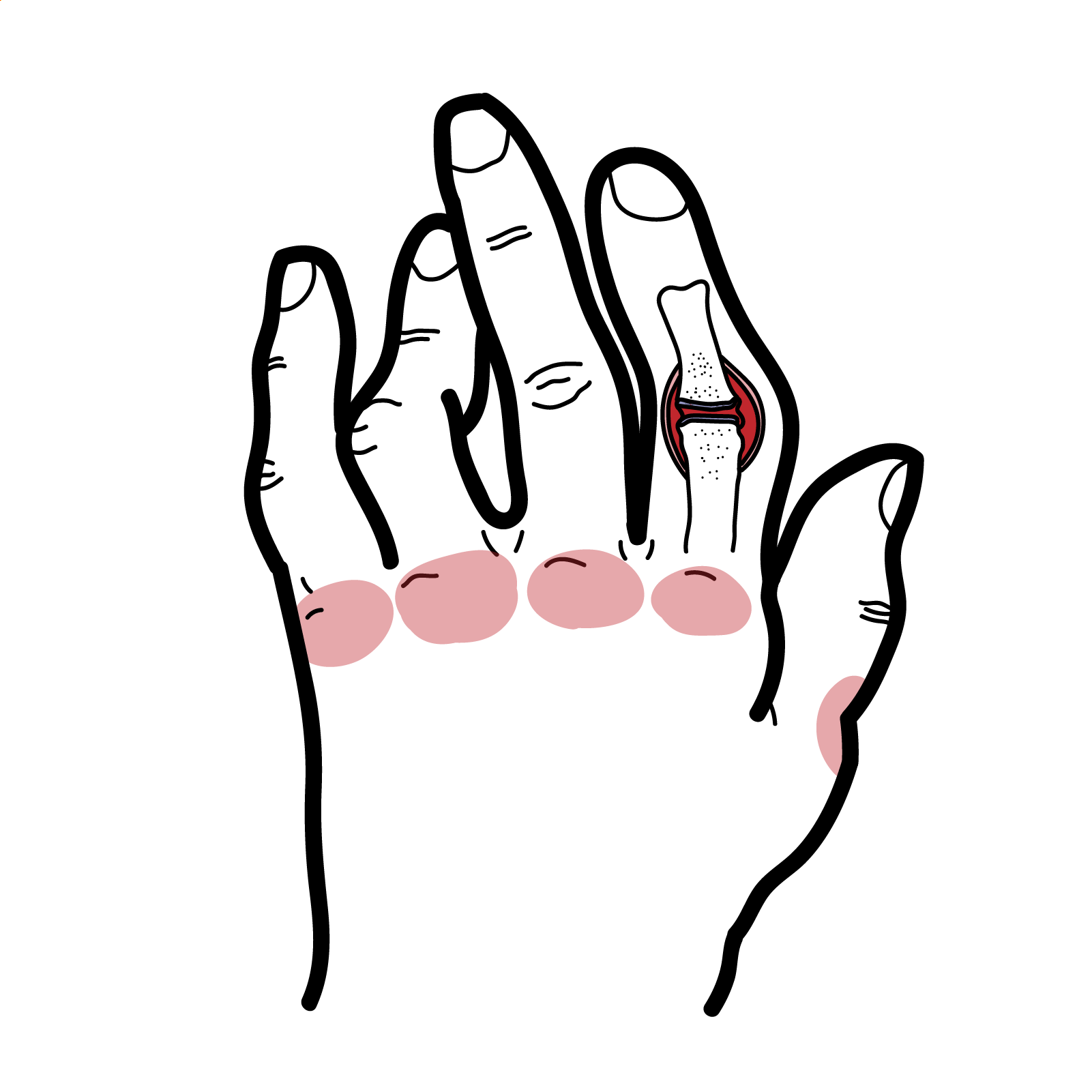
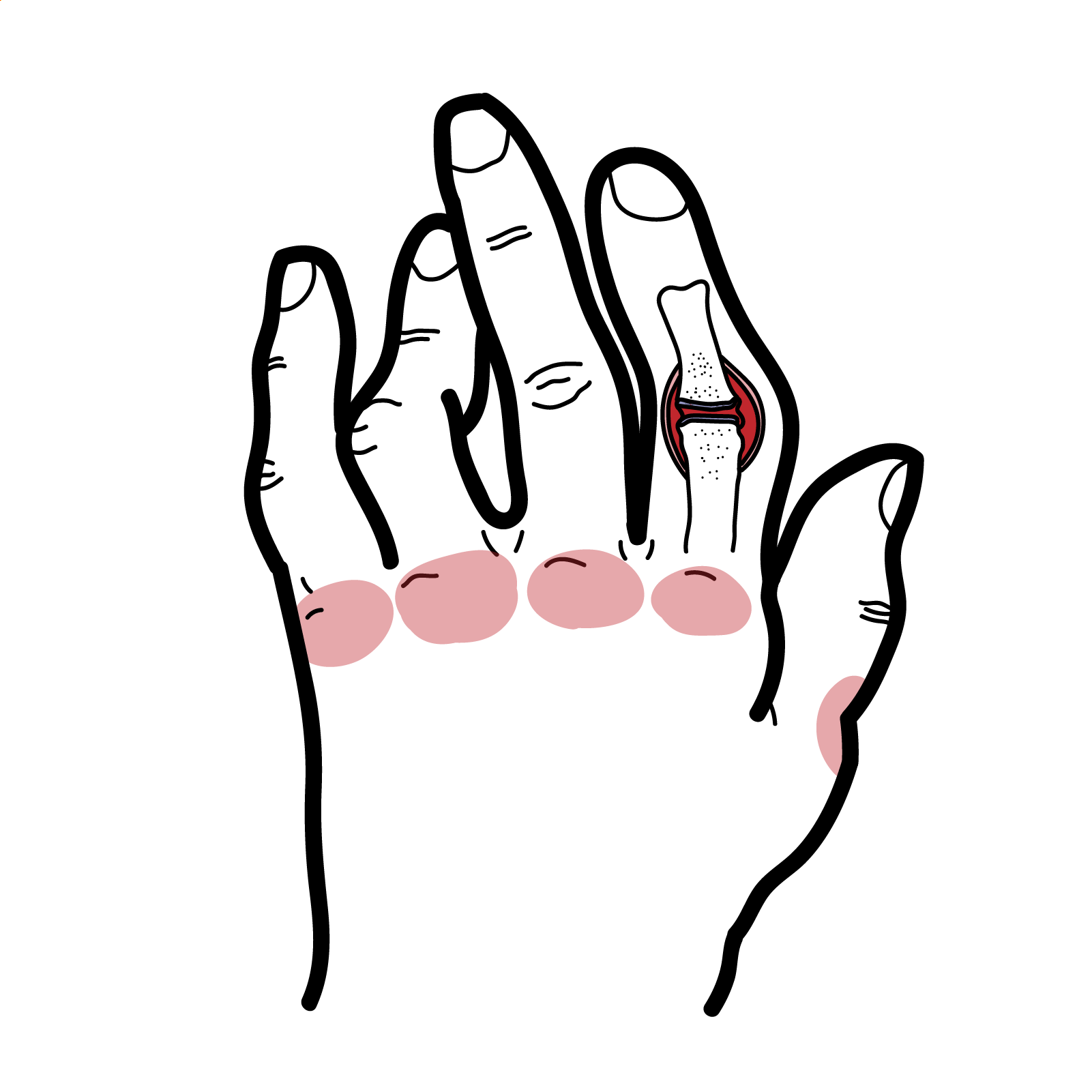
Rheumatoid arthritis: Characterized by symmetric polyarticular inflammation of the synovium, typically of the small joints of the hands (MCP and PIP), wrists and feet. This inflammation results in pain and stiffness, and can lead to progressive joint damage resulting in deformities and loss of function. Associated organ damage also contributes to severe disability.
Juvenile Rheumatoid arthritis: Heterogeneous group of several disease subtypes that are characterized by the onset of arthritis before the age of 16 years and has symptoms lasting at least 6 weeks.
Epidemiology
The main problem is RA is inflammation of the synovium.
Pregnancy often causes RA remission, likely because of immunologic tolerance. Breastfeeding decrease the risk of RA.
General Patients with RA typically present with pain and stiffness in multiple joints. The wrists, proximal interphalangeal joints, and metacarpophalangeal joints are most commonly involved. Morning stiffness lasting more than one hour suggests an inflammatory etiology.
Examination
Hand changes as rheumatoid arthritis progresses
Consider rheumatoid arthritis in any patient presenting with joint pain, swelling, and morning stiffness of over 30 minutes.
Extra-articular involvement
Caplan’s Syndrome Combination of rheumatoid arthritis and pneumoconiosis that manifests as intrapulmonary nodule.
Feltys’ Syndrome Triad: Rheumatoid arthritis, splenomegaly, neutropaenia.
Non-inflammatory Arthritis
Inflammatory Arthritis
More info on the Differential Diagnosis of Arthritis
Still’s Disease (Systemic-onset juvenile idiopathic arthritis) Triad Persistent high spiking fevers, arthlagia, and a distinctive salmon-colored bumpy rash.
| RADIOLOGICAL CHANGES IN JOINT | |
| Rheumatoid Arthritis | Osteoarthritis |
| Loss of joint space | Loss of joint space |
| Joint deformity | Osteophytes |
| Soft tissue swelling | Subarticular sclerosis |
| Juxtaarticular osteopaenia | Subchondral cysts |
| Other Conditions with positive RF (sero-positive) |
| Sjogrens syndrome (<100%) |
| Felty’s syndrome (<100%) |
| Rheumatoid arthritis (~75%) |
| Infection |
| Systemic lupus erythamtosus (<40%) |
| Systemic sclerosis |
| Mixed connective tissue disease |
Spondylarthropathies tend to have sero negative results (RhF negative).
Feltys’ Syndrome Triad: Rheumatoid arthrits, splenomegaly, neutropaenia
Diagnosis – 1987 American College of Rheumatology criteria
Principles of managing Rheumatoid arthritis
A guided exercise program can improve quality of life and muscle strength in patients with RA.
Pharmacological treatment
Pregnancy do not use Methotrexate! change to hydroxychloroquine!
| Side effects of NSAIDS | |
| Gastrointestinal Tract | Gastric bleeding and perforation (elderly, chronic use) |
| Renal | Fluid retention and papillary necrosis |
| Hypertension | Interference with drugs such as thiazide diuretics |
| Myocardial infarction | |
| Pulmonary | Exacerbation of asthma, pneumonitis (naproxen) |
| Skin | Hypersensitivity, erythema multiforme |
| CNS | Tinnitus, fatigue |
| Hepatic | Drug-induced hepatitis |
Methotrexate Inhibits dihydrofolate reductase. Methotrexate is given weekly. Side effects: Liver effects, teratogenesis, hair loss, oral ulcers. Toxicity (stomatitis, GI disturbance, and alopecia) may be reduced by the addition of folic acid daily, without loss of therapeutic effect. May cause flare of rheumatoid nodule. NSAID use is contraindicated because there is the potential for interaction and hepatotoxicity. DMARD monitoring is needed to ensure patients do not suffer serious side-effects.
Starting treatment with combination disease-modifying antirheumatic drugs (including methotrexate), especially within three months of symptom onset, can slow disease progression and improve symptoms, function, and quality of life.
Anti-TNFα biological agent. TNF-α is a potent pro-inflammatory cytokine whose levels are elevated in RA. Anti-TNFa inhibit action of TNF-α and causes immunosuppression. Side effects: Tuberculosis, opportunistic infection.
Complications
Feltys’ Syndrome Triad: Rheumatoid arthrits, splenomegaly, neutropaenia.
Prognosis
Overview
Juvenile idiopathic arthritis is the most common cause of chronic arthritis in childhood. It is characterised by joint inflammation that often leads to joint destruction with physical disability and chronic pain that affects daily life. The disease encompasses all forms of arthritis that begin before the age of 16 years, persist for more than six weeks, and are of unknown cause. The most common risk factors are infections in combination with genetic susceptibility. Many other factors, such as stress and maternal smoking, are thought to contribute to the pathogenesis.
Differences from adult RA include the problem of growth retardation, a tendency to early fusion of the carpal bones, and erosions at the distal interphalangeal joints.
Clinical Presentation
Differential Diagnosis
Investigations
Diagnostic criteria
Management The disease currently has no cure, but clinical remission is a realistic treatment goal
Complications (Extra-articular manifestations)
Ophthalmology review is important in Juvenile Rheumatoid Arthritis.
Wasserman, AM. (2011). Diagnosis and Management of Rheumatoid Arthritis. American Family Physician. 84 (11). 1245-1252.
Harnden, K., & Jackson, A. (2016). Rheumatoid Arthritis. BMJ: Practice. 357.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion