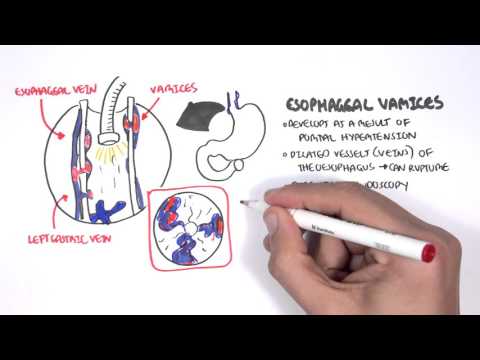
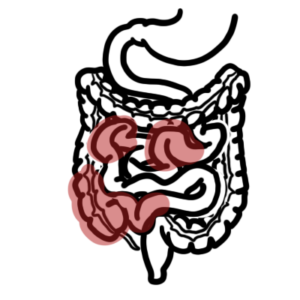
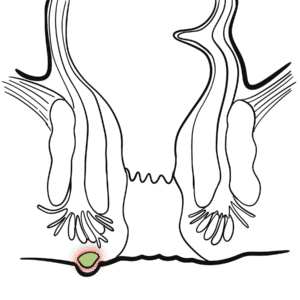
0:00 Patients with acute upper gastrointestinal bleeding commonly presents with he 0:10 matemesis, 0:11 which is vomiting of blood or coffee ground-like material, and/or malena, which 0:16 is a black 0:17 tarry stool. 0:19 The initial evaluation of patients with an acute upper gastrointestinal bleed 0:24 involves 0:25 an assessment of hemodynamic stability and resuscitation if necessary, 0:30 diagnostic studies, 0:31 usually endoscopy, and when possible, treatment of this specific cause. 0:37 Upper gastrointestinal bleeds, or upper GI bleed, can be differentiated from 0:43 lower gastrointestinal 0:44 bleeding based on clinical presentation. 0:46 We have malena and hematemesis for an upper GI bleed, and hematochizia, which 0:51 is fresh 0:52 blood and feces for a lower GI bleed. 0:55 Both may present with signs of anemia and blood loss, depending on the amount. 1:02 Upper GI bleeding can be differentiated from lower GI bleeding also based on 1:09 anatomy. 1:11 Upper GI bleeding occurs above the ligament of treats, whereas lower GI occurs 1:17 below the 1:17 ligament of treats. 1:18 The ligament of treats is a muscular band that suspends the fourth part of the 1:22 duodenum from 1:23 the right cruis of the diaphragm. 1:29 Now we will talk about the causes of upper GI bleeding, firstly the most common 1:35 , and 1:36 this is in descending order, and then we'll talk about the rare causes. 1:42 So probably the most common cause is gastric and/or duodenal ulcers. 1:46 Essentially ulcers form when there's more gastric acid secretion than there is 1:53 mucosal 1:53 defense. 1:55 The risk factors, common risk factors include hillocobacter pylori infection, 1:59 which is a 1:59 spiral bacterium that infects the superficial gastric mucosa and disrupts the 2:04 mucosa layer. 2:05 Non-steroidal anti-inflammatory drugs are also common cause, physiological 2:10 stress, excess 2:11 gastric acid, and rarely you get hyperacidity alone, and this can be due to a 2:17 syndrome, 2:18 for example, in patients with Zalinga Ellison syndrome. 2:27 Severe or erosive gastritis or duodenitis is another cause. 2:31 The term gastritis and duodenitis are used to denote inflammation associated 2:37 mucosal 2:37 injury. 2:40 The risk factors are also the same for peptic ulcer disease, as mentioned 2:46 earlier. 2:47 Severe or erosive esophagitis, as the name suggests, is severe inflammation of 2:52 the esophagus. 2:53 It's associated with gastroesophageal reflux disease, gourd or gourd. 3:00 On endoscopy, what you see is erosive damage to the esophageal mucosa. 3:06 Other risk factors include medication use, including non-steroidal anti- 3:10 inflammatory 3:11 drugs, oral bisphosphonates, tetracyclins and infections, including candida and 3:17 herpes 3:17 simplex virus. 3:20 Candida represents itself as white streaks in the esophagus, usually associated 3:24 with 3:24 some immunodeficiency. 3:28 A very important cause of upper GI bleeding is gastroesophageal varices, and 3:34 these usually 3:34 develop as a consequence of portal hypertension in approximately 50% of 3:39 patients with cirrhosis, 3:41 and variceal hemorrhage occurs at an annual rate of about 10%. 3:46 Varices may be identified in the esophagus and/or the stomach. 3:50 They may also be seen at sites other than the esophagus of the stomach, such as 3:54 the 3:54 small bowel, these are known as ectopic varices. 3:59 As with most other causes of upper gastrointestinal bleeding, endoscopy is a 4:02 diagnostic modality 4:03 of choice for esophageal gastric varices, and here you can see dilated veins. 4:13 The management of esophageal varices include band ligation, which is a standard 4:17 treatment. 4:18 You can also have sclerotherapy when band ligation is not technically feasible. 4:23 Also, there is early trans jugular intra-hypatic podosystemic shunts, or tips 4:29 for short. 4:30 The varices is usually managed with some sort of injection in the form of cyan 4:35 olacrylate, 4:36 which is glute. 4:42 Portal hypertensive gastropathy, also known as congestive gastropathy, is 4:46 caused by portal 4:47 hypertension. 4:49 The pathogenesis of portal hypertensive gastropathy may be related to both 4:54 congestion and hyperimia 4:55 in the stomach. 5:00 Angiotisplasia, also known as vascular ectasia, is essentially ectatic dilated, 5:09 thinned walled 5:11 vessels, is essentially ectatic dilated, thinned walled vessels, which can be 5:21 seen as spider 5:22 nevi in the stomach. 5:25 The vessels here are thin walled and are usually lined by endothelium alone, 5:30 not the 5:30 muscle, and so, as a consequence, it can easily rupture. 5:40 Dulophoys lesion is a dilated aberrant submucosal vessel that erodes the over 5:44 lying epithelium 5:45 in the absence of a primary ulcer. 5:48 The etiology of dulophoys lesion is unknown. 5:51 Additionally, events triggering bleeding are not well understood. 5:55 Patients who bleed from dulophoys lesions are typically men with comorbidities, 6:00 including 6:00 cardiovascular disease, hypertension, chronic kidney disease, diabetes, and 6:09 alcohol abuse. 6:11 Mallory-wise syndrome is characterized by longitudinal mucosal lacerations, int 6:17 ramural 6:18 dissections, they're called, in the distal esophagus and the proximal stomach. 6:23 And these are usually associated with forceful retching. 6:28 The lacerations often lead to bleeding from submucosal arteries. 6:32 These tears usually heal spontaneously. 6:40 Very important cause of upper gastrointestinal bleeding, although less common, 6:46 are mass 6:46 lesions, including polyps and cancers. 6:49 Many plasms of the upper gastrointestinal tract account for less than 3% of all 6:53 cases 6:54 with severe upper gastrointestinal bleeding. 6:57 The bleeding here is usually slow. 7:00 In a majority of cases, actually, no lesions are identified. 7:04 And so when patients present with upper GI bleeding and get an endoscopy, there 7:07 's actually 7:08 no lesions identified, even with a pill cam. 7:14 Now we'll talk about other rarer causes of upper gastrointestinal bleeding. 7:22 Gastric ancho-vascular-ectasia gave, also known as watermelon stomach, is an 7:28 uncommon 7:29 cause of upper gastrointestinal bleeding. 7:32 The term watermelon stomach is derived from the characteristic endoscopic 7:36 appearance of 7:37 longitudinal rows of flat reddish stripes radiating from the pylorus in the an 7:42 terum that 7:42 resemble the stripes on watermelon. 7:45 The red stripes represent "ectatic" and "saculated" mucosal vessels. 7:50 Gave is seen in patients with liver cirrhosis and/or systemic sclerosis. 7:59 Hemobilia, or bleeding from the hepatobiliary tract, is a rare cause of acute 8:03 upper gastrointestinal 8:04 bleeding. 8:05 It should be considered in any patients with acute upper GI bleed and a recent 8:09 history 8:09 of hepatic parenchymal or biliary tract procedures of any sort. 8:17 Hemosuchus pancreaticus, or bleeding from the pancreatic duct, is another rare 8:20 cause 8:21 of upper GI bleeding. 8:24 It is most often found in patients with chronic pancreatitis or pancreatic tum 8:36 ours. 8:36 Aortointeric fistulas, as the name suggests, is a connection between the aorta 8:42 and the 8:42 small intestine. 8:43 It is a very rare cause of acute GI bleeds and is most often eatrogenic. 8:50 Usually following an aortic graft procedure and you have a leak. 8:54 It is associated with high mortality rates and represents a true medical 8:58 emergency. 8:59 The third or fourth portion of the duodenum is the most common site for aorto 9:03 interic 9:04 fistulas. 9:06 This disorder should be considered in all patients with massive or repetitive 9:09 upper GI bleeding 9:10 and a history of thoracic or abdominal aortic aneurysm prosthetic graft. 9:24 Cameron lesions are erosions or ulcers occurring in the sack of a high atal her 9:30 nia. 9:31 They have been described in up to 5% of patients with high atal hernia who 9:34 undergo upper endoscopy 9:36 Another important cause to consider is eatrogenic bleeding after an endoscopic 9:42 procedure. 9:43 For example, maybe removing a polyps or having a biopsy of the upper 9:50 gastrointestinal tract. 9:53 Clinical presentation of an acute upper GI bleed include hematemesis, malena, 9:59 signs of 9:59 anemia, so you have fatigue, you have shortness of breath, tachycardia, orthost 10:03 atic hypertension, 10:06 and then you have the signs based on the actual underlying cause. 10:10 So upper abdominal pain for a peptic ulcer disease, odinophagea, gastroesophage 10:16 al reflux, 10:16 dysphagia for esophagitis or esophageal ulcers. 10:21 History or someone dry-wrenching or coughing indicates Mallory-wise tear. 10:30 A history of dysphagia, early satiety, involuntary weight loss, kexia, consider 10:38 malignancy. 10:39 If you have acites and jaundice, consider varicyl hemorrhage or poral hypert 10:48 ensive gastropathy. 10:51 The initial management for upper GI bleeding, acute upper GI bleeding, involve 10:57 resuscitation, 10:58 insertion of two large IV cannulas, performing baseline bloods, including coag 11:05 ulation profile 11:06 and group and hold and cross-match, administering crystalloids which will 11:11 correct hemodynamics 11:13 in majority, also administering intravenous proton pump inhibitors. 11:19 And of course, this can be followed by blood products, and for blood transf 11:22 usions, there 11:23 are certain indications, but basically you want to transfuse everyone when 11:26 there are hemoglobin 11:27 less than 70. 11:30 For people at higher risk, you transfuse less than 80. 11:34 Different protocols vary. 11:36 Platelets are rarely indicated, but you can consider if there are actively 11:39 bleeding and 11:40 there are platelets are less than 50. 11:43 Importantly to correct coagulopathy if present, with vitamin K, fresh frozen 11:47 plasma, prothrombonyx. 11:50 Imaging the patient with a CT abdomen would be warranted, but fundamentally an 11:54 endoscopy 11:55 should be performed within 24 hours, as this reduces hospital lengths of stay 11:59 and reduces 12:00 blood transfusion requirements. 12:04 Thank you for watching. 12:05 So in summary, upper GI bleeding presents with hematemesis and malena with and 12:11 without 12:11 signs of anemia. 12:12 We learned about the different causes, the most common are ulcers of the gast 12:17 ric duodenum, 12:18 and you have other rare causes we talked about. 12:21 The management involves resuscitation.