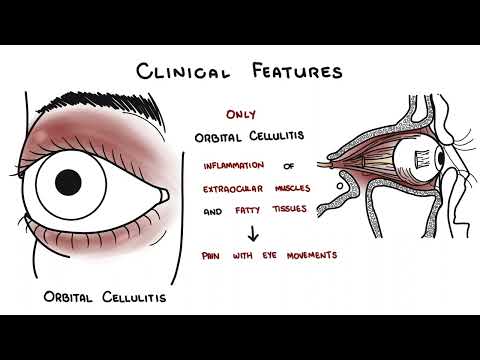
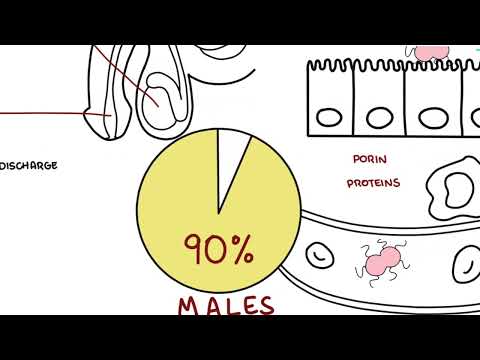
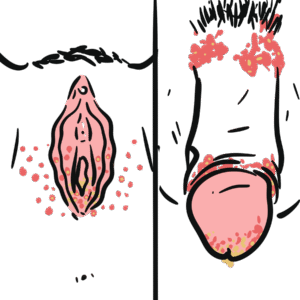
0:00 Hello in this video, we're going to talk about cellulitis and erycipolis, which 0:10 are 0:11 bacterial skin infections. 0:16 Cellulitis is a bacterial skin infection of the dermis and the subcutaneous 0:20 tissue. 0:21 The normal presentation of cellulitis is an infection in the lower limb, such 0:27 as near 0:27 the tibia, for example. 0:29 A good differential for cellulitis is another bacterial skin infection called 0:34 erycipolis, 0:35 which is actually known as superficial cellulitis, because it is infection of 0:40 the superficial 0:41 dermal layer. 0:43 So let's just learn about erycipolis first, but first of all recap the anatomy 0:47 of the 0:48 skin. 0:49 The skin anatomy, the skin layers, two main ones, epidermis and the dermis. 0:55 Below the dermis is your subcutaneous tissue, also known as a hyperdermis, 0:59 which is what 1:00 actually makes up your superficial fascia. 1:03 Below the superficial fascia is a deep fascia, a layer of connective tissue 1:08 which surrounds 1:09 organs such as your muscle here. 1:13 Erycipolis is an infection involving this area here, which is the superficial 1:18 dermis. 1:19 Again, it is a superficial dermal infection. 1:26 The main causative agent is usually Group A streptococcus, which is also known 1:33 as strep 1:34 pyogenes. 1:35 It is essentially a cocchi, a gram positive cocchi. 1:40 The clinical presentation of erycipolis, classic one is an example of a patient 1:45 coming 1:45 in with sort of a swelling inflamed butterfly appearing rash, which is a good 1:51 differential 1:52 for systemic lupus erythmatosis. 1:56 Besides from this, the patient can present with systemic features such as fe 2:00 vers, chills, 2:02 riagos, as well as lymphatic involvement. 2:06 Erycipolis can also present in the lower limbs, such as in around the tibia for 2:10 example, and 2:12 it has the cardinal features of inflammation, which is very important. 2:15 These are warmth, erythema, which is redness, tenderness, as well as swelling. 2:22 If we were to look at erycipolis again in this skin diagram, we can see that 2:28 the whole 2:29 skin area is markedly raised and it forms distinct borders. 2:35 This is because you have inflammation of the superficial dermis, which pushes 2:38 everything 2:38 up. 2:39 In this area, you also have your lymph vessels and its valves coming all the 2:44 way up to the 2:45 superficial dermis, and that is why you commonly get lymphatic involvement. 2:52 Now that was erycipolis, let's compare that to cellulitis. 2:56 The classic presentation of cellulitis, as I mentioned, is in the lower limbs, 2:59 such as 3:00 around your tibia, and this is classically in patients with risk factors such 3:05 as diabetes. 3:06 The other common presentation is in children around the eye. 3:10 This is called periorbital cellulitis, and like erycipolis, cellulitis has a 3:15 cardinal 3:15 features of inflammation. 3:17 You have warmth, you have erythema, you have tenderness, and you have swelling. 3:23 So let's take a closer look at cellulitis and see what happens in the skin 3:31 itself. 3:33 This is bacterial infection involving the dermis, more specifically the deep 3:39 dermis 3:40 and the subcutaneous tissue. 3:43 And because it is a more deeper infection, a deeper dermal infection and subcut 3:47 aneous 3:48 tissue, the appearance of the skin is only a little bit of swelling, it's only 3:53 slightly 3:53 raised, and you have more of an indistinct border. 3:59 Basically what you can do is, in the area of infection, you can use a marker 4:03 and draw 4:04 around it and date it. 4:06 The next day you can see whether the infection is getting worse, and this is 4:11 also a good 4:11 way to see if antibiotic treatment is working or not. 4:17 The main causative agent of cellulitis is staphylococcus species, such as staph 4:24 aureus, 4:25 as well as beta-humolytic streptococci, such as group A streptococcus. 4:36 Let's just now briefly look at the pathophysiology of both erycipolis and 4:42 cellulitis. 4:43 Basically you have bacteria who possess virulent factors, such as, you know, 4:48 your exfoliate 4:49 toxins and whatnot, and these virulent factors which will allow the bacteria to 4:56 penetrate 4:57 and invade the skin layers. 5:01 At the same time, the patient have their own risk factors, which will increase 5:06 their risks 5:07 of developing cellulitis. 5:10 And so both the bacteria factors and the patient's risk factors will allow for 5:15 inflammation 5:15 to take place in the dermis or the subcutaneous tissue area. 5:23 So what are these patient risk factors I am talking about? 5:26 Well, these risk factors include having a history of cellulitis, tigna pedis 5:31 interdigitalis, 5:32 which is basically a fungal infection between your toe webs, allowing basically 5:39 axis of bacteria 5:40 into the dermis area. 5:42 Also, if you have trauma, pre-existing skin conditions such as dermatitis also 5:46 increases 5:47 the risk. 5:49 Other risk factors include lymphodema, obesity, diabetes, as well as venous ins 5:59 ufficiency. 6:01 Celluditis and erycipolis can be difficult to distinguish, however both are 6:05 diagnosed 6:06 clinically. 6:12 Investigations that can be performed include culture of a wound foci. 6:18 So a focus within the wound can be cultured, however this is not often found. 6:25 An x-ray of the area of the limb can also be done if you suspect complications 6:29 such as 6:29 osteomyelitis. 6:30 Finally, you can also culture the tigna interdigitalis and you can also perform 6:30 blood cultures if 6:37 you suspect sepsis and bacteremia. 6:40 Also if you suspect the patient has an abscess, a contained infection, you can 6:52 order an ultrasound. 6:55 The management of cellulitis and erycipolis is actually the same. 6:59 Because the main causative organisms of both are gram-positive bacteria such as 7:03 staph aureus 7:04 and group A-sheptococcus, remember these guys gram-positive bacteria if they 7:09 have an 7:09 outer, thick peptidoglycan layer, and then they have a plasma membrane below it 7:15 , and 7:15 then inside the cell they have proteins such as ribosomes. 7:20 Well the management of erycipolis and cellulitis are antibiotics, first-line 7:25 penicillins such 7:26 as dichoxicillin and flucoxicillin. 7:29 The mechanism of action is that they inhibit cell wall synthesis, bacterial 7:34 cell wall synthesis. 7:38 If the patient is hypersensitive to penicillins, so they have some form of 7:43 reaction, you can 7:44 give cephalosporins, which are also beta-lactams and work the exact same way as 7:50 penicillins. 7:51 They inhibit cell wall synthesis of the bacteria. 7:54 However, if the patient is anaphylactic to penicillins, you probably don't want 7:59 to use 8:00 another beta-lactam, and so an alternative is a drug such as klindamycin. 8:05 Clindamycin works by inhibiting protein synthesis, and thus by disrupting 8:11 protein synthesis 8:11 you essentially cause stasis of bacterial function. 8:17 Complications of cellulitis and erycipolis are a lot. 8:21 Some common ones include sepsis as well as chronic edema. 8:25 Chronic edema occurs if you can imagine, if you have inflammation of the deeper 8:30 skin 8:30 layers, you're essentially increasing pressure, and thus you don't allow the 8:36 veins to return 8:36 blood to the heart, and so it backflows causing chronic edema. 8:41 I hope you enjoyed this video on erycipolis and cellulitis, thank you for 8:44 watching.