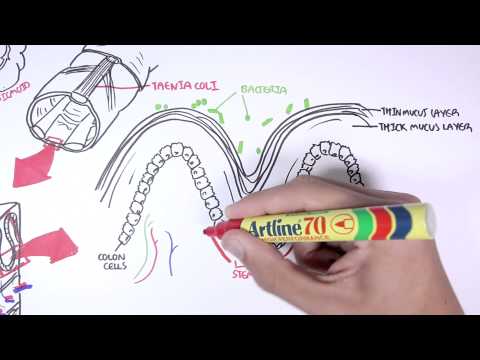
0:00 In this video we're going to talk about colorectal cancer. 0:07 This is an overview and introduction. 0:10 Colorectal cancer is the second most commonly diagnosed cancer, and is the 0:14 commonest gastrointestinal 0:16 malignancy. 0:18 The prevalence of colorectal cancer is increasing in the younger population, 0:22 and this could 0:23 be attributed to diet. 0:25 This is also the same with diverticular disease. 0:29 Family history is strong in colorectal cancer. 0:33 The risk factors for developing colorectal cancer include age, male sex, 0:39 smoking, family 0:41 history, as we discussed, diet high in red meat, and poor in fiber, Polyposis 0:48 syndrome, 0:49 or FAP, FAP, and HNPCC, or Lynch disease. 0:56 Other risk factors also include history of polyps, certain types of polyps that 1:03 is, personal 1:04 history of colon cancer, and also having inflammatory conditions of the bowel, 1:10 including all sort 1:11 of colitis and Crohn's disease. 1:15 The signs and symptoms or clinical presentation differ depending on where the 1:21 cancer or growth 1:22 occurs within the bowel. 1:25 Of course, this is just a summary. 1:27 People vary in their clinical presentation. 1:31 So here I am drawing a colon, ascending transverse descending sigmoid and the 1:42 rectum. 1:44 Cancer's tumours that occur on the right side account for 20% of cases of colon 1:49 cancer. 1:50 People are often asymptomatic, present with weight loss, and iron deficiency. 1:57 People also present with a palpable mass on the lower right quadrant of the 2:02 abdomen. 2:03 And this is because they are often asymptomatic, and so the tumour can grow 2:09 without notice 2:10 until signs of weight loss and anemia occurs. 2:15 Patients occurring in the descending sigmoid area account for the majority of 2:19 colon cancer, 2:20 75% of cases. 2:22 Patients can complain of dark red blood mixed in with stools, plus minus clots. 2:29 There can be increased bowel frequency, abdominal pain, and bloating flatulence 2:34 and mucous present. 2:40 As occurring in the rectal regions can present with deep red blood on the 2:44 surface of the stool. 2:47 People can also have abdominal pain, plus minus tenesimus. 2:51 You can imagine a growth in the rectum would cause sensation of incomplete 2:59 evacuation. 3:01 The colon is an amazing organ, general macroscopic differences between normal 3:07 and cancerous. 3:08 The colon have tine coli, which are separate longitudinal ribbons of smooth 3:13 muscles on 3:13 the outside of the ascending, transverse, descending, and sigmoid colons. 3:20 The tine coli contract lengthwise to produce the host drug, the bulges in the 3:26 actual colon. 3:28 The colon is supplied by arteries that branch from the inferior mesenteric 3:33 artery. 3:34 The inferior mesenteric artery further branches into smaller arteries, which en 3:40 astomers with 3:40 each other. 3:42 These have importance when part of the colon is being resected, because we want 3:48 to maintain 3:49 blood flow to the remainder of the colon. 3:53 When colon cancer occurs, the tumours can obstruct the lumen. 3:58 The chemical produced by the cancers can cause angiogenesis, formation of new 4:04 blood vessels, 4:05 which contribute to the bleeding found in colon cancer, so patients often 4:11 present with 4:11 rectal bleeding. 4:13 Athology, colon cancer can come in a few pathological forms, polyploid, ulcer 4:23 ative, stenosing and 4:26 infiltrative. 4:28 At the end of the day, these different pathological types can and will 4:33 eventually lead to some 4:34 form of obstruction. 4:39 The investigations performed for patients suspected of colon cancer, or any 4:45 form of mass, includes 4:47 an abdominal examination, followed by a per rectal examination. 4:53 And this is done with the proctoscopy, to check for any obvious masses and 4:58 sources of 4:58 bleeding, such as from internal hemorrhoids. 5:03 Colonoscopy is then considered, which is under general anesthesia, and involves 5:07 the doctor 5:08 inserting a colonoscope through the back passage and visualizing the colon. 5:13 Polyps can be taken out and sampled to check for malignancy. 5:19 Barium NMR colonography can also be performed. 5:22 Finally, you have blood investigations, which include LFT, FBC and the tumour 5:28 marker for 5:28 colon cancer, CEA. 5:33 Once and if the cancer is diagnosed, it is important to stage the cancer. 5:39 Staging investigations used include biopsies, CT scans and PET scans. 5:48 For staging itself, there are two forms of staging. 5:52 The first is the T-N-M staging, which looks at T, the primary tumour, N, the 5:58 lymph node, 5:59 and M, metastasis. 6:06 The second form of staging is juke staging, which looks at the five-year 6:10 survival, and 6:11 there are a total of four stages, plus stage zero. 6:16 Stage zero is nothing really, and nine. 6:19 The remaining of the stages, it depends on how deep the tumour is going, so 6:25 what layers 6:26 it's going into, and if it has metastasized. 6:30 So stage zero, there is a 90% five-year survival. 6:34 Stage two, the tumour is growing even deeper, 70% five-year survival. 6:39 Stage three, about 30%, stage four, it's less than 10% five-year survival with 6:47 metastasis. 6:49 Management of colon cancer. 6:51 Colon cancer is potentially curative with surgical resection of the colon, co 6:55 lectomy, 6:56 with also surgical resection of the lymph nodes, lymph adenectomy. 7:02 Surgical resection of the colon, colectomy, is performed depending on where the 7:07 tumour 7:08 is located on the colon, and when surgically removing parts of the colon, it is 7:13 important 7:14 to take into consideration the blood supply of that part of the colon, as well 7:19 as the 7:19 lymph drainage of that part. 7:22 Tumors that occur on the right side of the log intestine or in the right trans 7:29 verse area 7:30 requires a right hemiclectomy extended. 7:38 Tumors occurring on the left side require left hemiclectomy. 7:45 Tumors occurring in the sigmoid and upper rectum require a high anterior rese 7:51 ction. 7:51 Tumors in the rectum require APER abdominal resection. 8:00 Also during this procedure, some patients may require having a temporary or 8:05 even a permanent 8:06 colostomy bag pouches, which while others get the colon joined to the other 8:13 parts, to 8:13 the remaining parts of the colon eventually. 8:16 Of course, together with colectomy, there is adjuvant chemotherapy with or 8:21 without radiotherapy. 8:23 Chemotherapy usually involves a five-floor uracil. 8:28 If the cancer has metastasized, that organ can be potentially removed. 8:33 And finally, there is also a palliative care. 8:43 [BLANK_AUDIO]