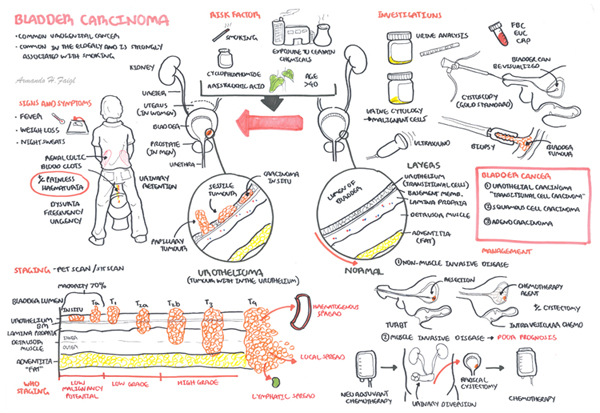
| Three main types of bladder carcinoma |
| Transitional cell carcinoma (Most common) |
| Squamous cell carcinoma |
| Adenocarcinoma (Rare) |
Overview Transitional cell tumours can affect any part of the urinary epithelium. It is the second most common urological malignancy (Renal Adenocarcinoma is the most common, bladder adenocarcinoma is rare) and is one of the most common cause of cancer related death. Bladder cancer occurs most commonly from the fifth to seventh decades of life and is more common in men. Transitional cell tumour is also known as urothelial carcinoma and has a broad spectrum of morphology from low grade, sea weed looking, superficial papiliferous growths to invasive, solid mass.
| Definition Transitional endothelial cells: Endothelial cells that can change shape Transitional cell Tumours (TCT): Spectrum of disease from benign superficial growths to invasive carcinomas. TCTs may affect any part of the urinary epithelium (bladder, ureter). |
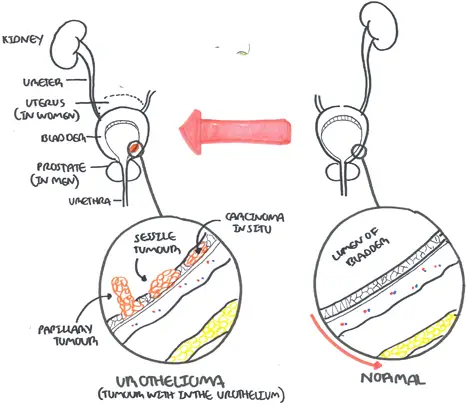
| Side note Transitional epithelial cells are found in the bladder, ureter and part of the kidneys and urethra. Therefore transitional cell carcinoma can occur in any of these areas. |
An empty urinary bladder sits behind the pubic symphysis, when filled the bladder rises and is higher and can be readily palpated and percussed. In children the urinary bladder sits higher normally.
Extending of the dome of the bladder to the umbilicus is the median umbilical ligament, a fibrous cord that represents the obliterated urachus.
Layers of the bladder
Detrusor muscle is made up of smoother muscle fibers arranged at random in a longitudinal, circular and spiral manner without any layer formation or orientation. However at the internal meatus, the detrusor muscle forms three specific layers:
Arterial Supply
In females the uterine and vaginal artery also send some blood supply
Venous drainage Surrounding the bladder is a rich venous supply that drains essentially to the internal iliac veins → common iliac veins → IVC
Lymphatic Drainage
Innervation
Micturition Physiology
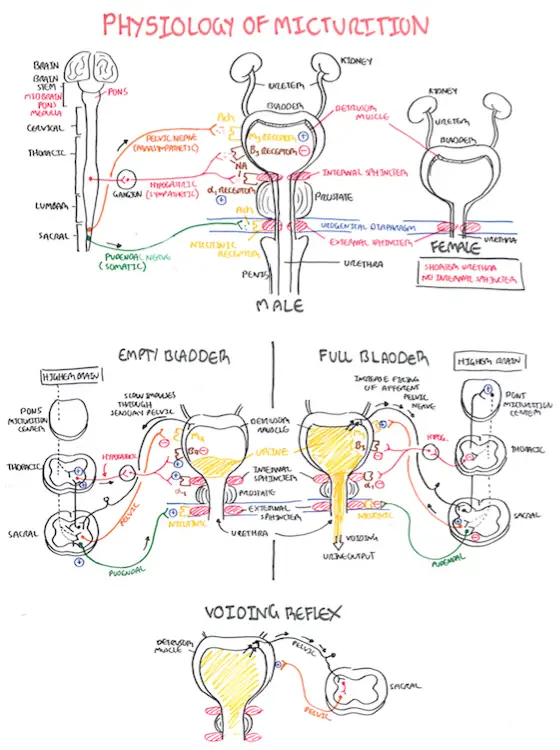
| Watch Video Physiology of Micturition |
| Risk Factors |
| Age >40 years old |
| Smoking (main factor) |
| Aromatic amines |
| Cyclophosphamide |
| Schistosoma haemotabium (squamous cell carcinoma) |
| Chronic irritation (squamous cell carcinoma) |
| Aristolochic acid |
| Remember The most common presentation of bladder cancer is painless haematuria |
Painless haematuria: Microscopic (invisible) or macroscopic
Irritative symptoms
Obstructive symptoms
Signs and Advanced disease
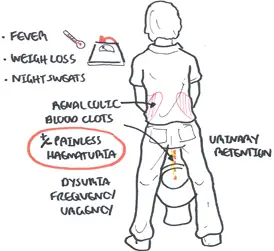
| Remember >40 year old presenting with painless haematuria is bladder malignancy (+/- risk factors) until proven otherwise |
| Side note All patients with macroscopic haematuria or persistent microscopic haematuria should be referred to a urologist for evaluation. |
| WHO Grading of transitional carcinoma |
| Urothelial papilloma |
| Papillary urothelial neoplasms of low malignant potential (PUNLMP) |
| Low-grade papillary urothelial carcinoma (PRESENTS MOST COMMON) |
| High-grade papillary urothelial carcinoma |
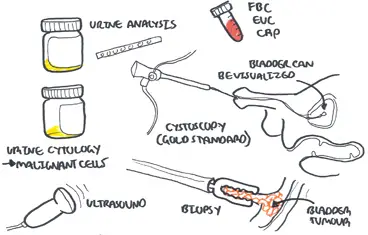
Staging uses MRI and CR scanning to detect local or systemic spread
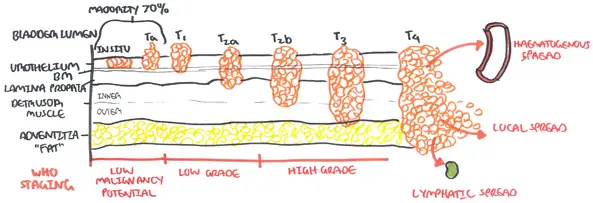
| Side note To make it easy think of Low-grade as being non-muscle invasive and high grade as muscle invasive |
70% are superficial in nature at diagnosis, being confined to the mucosa. Transitional cell carcinoma must be differentiated from other forms of bladder cancer
| Bladder Carcnoma | Pathological change |
| Transitional cell carcinoma (most common) | papiliferous growths "seaweed" to solid, invasive looking tumour |
| Squamous cell carcinoma | |
| Adenocarcinoma (rare) |
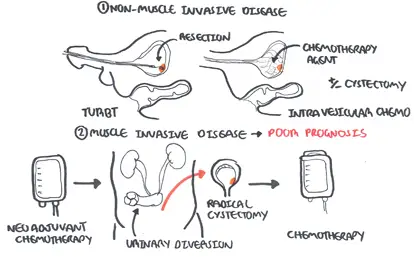
Transitional carcinoma can invade the muscle layer of the bladder and this will tailor management:
| Bladder Carcnoma | Management |
| Transitional cell carcinoma (most common) | Transurethral resection +/- Chemotherapy +/- Radical cystectomy |
| Squamous cell carcinoma | Cystectomy or radiation therapy |
| Adenocarcinoma (rare) | Cystectomy or partial cystectomy + Chemotherapy |
Follow-up
Complications
Prognosis
Mainly focusing on Transitional cell tumours