Overview
Overview Benign prostatic hyperplasia (BPH) is a non-malignant enlargement of the prostate gland. There is an increase in stromal and glandular components.
Anatomy
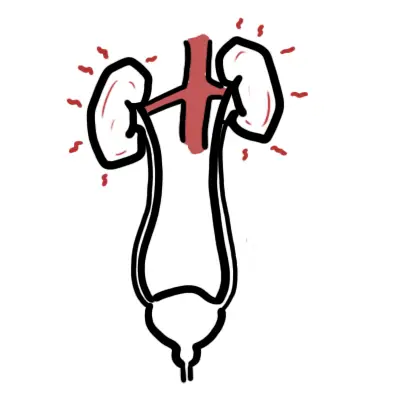
The prostate is an male organ that sits inferior to the bladder and surrounds the first part of the urethra. It is oval shaped and approximately 4cm thick.
The prostate gland is divided into three zones the central, transitional and peripheral.
- Peripheral zone - closest to rectum majority of cancer occurs here
- Transitional zone - the middle area of the prostate in between the central and peripheral zone. It surrounds the urethra. The majority of benign prostatic hyperplasia occurs here
- Central zone - lies anterior to the transitional zone and so lies farthest from the rectum
There are three main arteries that supply blood to the prostate the inferior vesicular artery, branches of the internal pudendal and inferior rectal artery.
Function of the prostate gland is to produce fluid that help nourish the sperm during ejaculation. The seminal vesicles, another structure that passes by the prostate, produces the majority of semen (fluid). Another function is that the prostate plays a role to help control urine flow. The prostate is under involuntary control.
Signs and Symptoms
Storage - FUNI
- Frequency
- Urgency
- Nocturia
- Incontinence
Voiding - PATHI
- Poor Stream
- Abdominal straining
- Terminal dribbling
- Hesistency
- Intermittency
| Per Rectal examination |
| Normal Prostate: Bi-lobed, central furrow, firm and smooth Prostatic Hyperplasia: Unable to palpate top of prostate Prostitis: Tender and boggy Carcinoma: Hard, nodular |
Differential Diagnosis
- Prostatitis
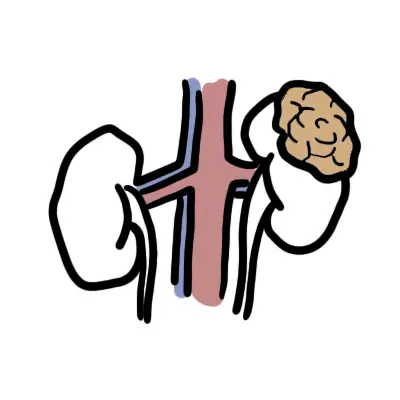
- Prostate Cancer
- Urinary Tract Infection
- Bladder Cancer
| Differences between BPH and Prostate Cancer | ||
| BPH | Prostate Carcinoma | |
| Signs and symptoms | Voiding and storage symptoms | Voiding, storage symptoms, weight loss, loss of appetite, night sweats. |
| Rectal Examination | Firm, smooth, enlarged | Hard, stony, nodular, irregular, no median groove |
| Location | Transitional Zone | Peripheral Zone |
Investigations
BPH is very common in the elderly man. If BPH is suspected it is important to perform PSA and urinalysis to rule out other differentials. This should always follow a Digital rectal examination. Other investigations:
- EUC
- Renal ultrasound
- Cystoscopy
Pathophysiology
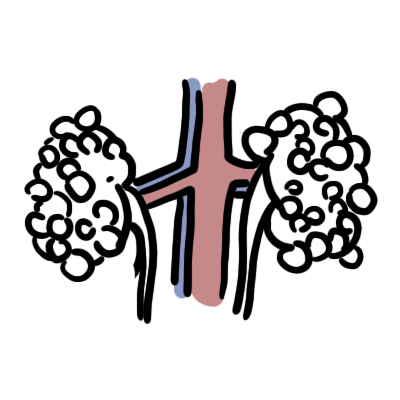
Hyperplasia of the epithelial and stromal compartments, particularly in the transitional zone, may be attributed to various factors including shifts in age-related hormonal changes creating androgen/oestrogen imbalances.
BPH involves hyperplasia of both epithelial and stromal prostatic components. A key characteristic of BPH is increased stromal: epithelial ratio. Over time, prostatic hyperplasia can result in bladder outlet obstruction. Obstruction has both a prostatic component due to increased epithelial tissue, particularly in a transition zone, and a dynamic component due to increases in stromal smooth muscle tone.
Management
Medical Treatment
- Watch and wait
- α-antagonists
- 5α-reductase
| Pharmacology α-antagonists relaxes smooth muscle of prostatic urethra to decrease outlet resistance; side effects include dizziness and hypotension (especially postural). |
| Pharmacology 5α-reductase inhibitors blocks the conversion of testosterone to dihydrotestosterone (DHT); side effects include loss of libido and erectile dysfunction. |
Surgical Treatment Reserved for those with complications and not responding for treatment
- Transurethral resection of the prostate (TURP)
- Open retropubic prostatectomy
- Transurethral incision in the prostate (TIUP)
- Bladder neck incision
Complications and Prognosis
Complications UTI is a common complication of BPH because of the change in urine flow and stasis of the bladder.
Prognosis
- The majority of patients with BPH can expect at least moderate improvement of their symptoms
- Lower urinary tract symptoms (LUTS), secondary to BPH, may affect sexual wellbeing including erectile function. Medical therapy for BPH may also effect sexual function, beneficially and harmfully, so this must be considered on an individual basis.