Overview
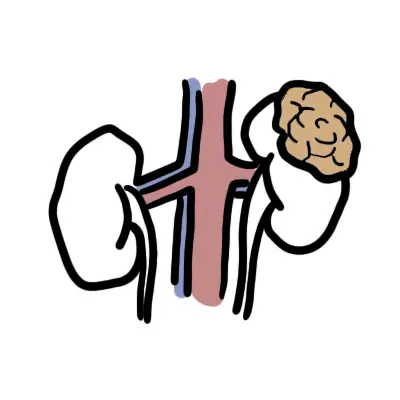
Overview Renal cell carcinomas (originate within the renal cortex) are responsible for 85% of all primary renal neoplasms. Transitional cell carcinomas of the renal pelvis are the next most common (~8%). Renal medullary carcinoma is a rare form of RCC seen in sickle cell disease. The most common pathological type of renal cell carcinoma is clear cell carcinoma.
| Definition Von Hippel–Lindau disease: Autosomal dominant disorder, bilateral renal cell carcinomas are common and haemangioblastomas, phaeochromocytomas and renal cysts are also found Renal cell carcinomas (RCC): arise from proximal tubular epithelium. They are the most common renal tumour in adults. They rarely present before the age of 40 years, the average age of presentation being 55 years. |
| Nephroblastoma (Wilms' tumor) is common in children and make a majority of childhood primary renal carcinomas. |
Classification
Renal cell carcinoma can be pathologically classed:
- Clear cell (80%)
- Papillary (chromophilic) (10%)
- Chromophobe (8%)
- Oncocytic (5%)
- Collecting duct (Bellini's duct) (very rare)
| Remember Clear cell carcinoma strongly asscoiated with Von Hippel Lindau (VHL) syndrome. |
Renal Anatomy
Kidneys are bean shaped organs that sits retroperitoneally at vertebral levels T11-L3. Above each kidney are the adrenal glands. The kidney is surrounded by a renal capsule. Surrounding the kidney + adrenal glands is the renal fascia also known as the Gerota's fascia.
Gerota's Fascia (renal fascia) surrounds the kidney + adrenal glands and extends to the renal vein and renal artery and wraps around the inferior vena cava and abdominal aorta.
The kidneys is divided into three sections:
- Renal cortex - renal arches and renal columns
- Renal Medulla - pyramids, papillae, major calyx, minor calyx
- Renal Sinus - Pelvis, renal vessels and lymphatics
Arterial Supply
- Aorta → Renal artery (L2 level) → Segmental artery → Interlobular artery → Cortical radiate artery → Afferent Arteriole → GLOMERULUS
Venous Drainage
- GLOMERULUS → Efferent arteriole (has branches forming the Vasa recta) → Arcuate vein → Interlobar vein → Renal Vein → Inferior vena cava
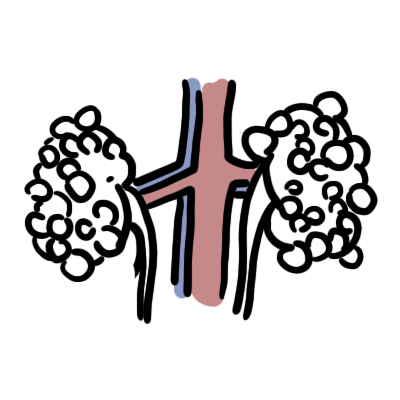
Nephrons
- Functional units of Kidneys
- Nephron's are structurally divided into two types:
- Cortical
- Juxtamedullary
- Nephron is a long tube that is divided into the following sections:
- Bowman's capsule - where the GLOMERULUS sits and filters blood into the nephron
- Proximal convulated tubule
- Loop of Henle
- Distal convulated tubule
- Collecting duct
The collecting ducts then drain into the Minor calyx → Major calyx → Renal pelvis → Ureter → Urinary bladder.
Risk Factors
| Risk Factors |
| Age >40 years old |
| Hypertension |
| Obesity |
| Polycystic Kidney Disease |
| Smoking |
| Chronic analgesic use |
| Sickle cell disease |
| Renal stones |
| Chronic hepatitis C infection |
| Aromatic amines |
| Cyclophosphamide |
| Schistosoma haemotabium (squamous cell carcinoma) |
| Chronic irritation (squamous cell carcinoma) |
| Aristolochic acid |
Signs and Symptoms
Asymptomatic until the disease is advanced
- 25% of individuals either have distant metastases or advanced loco regional disease
Symptomatic
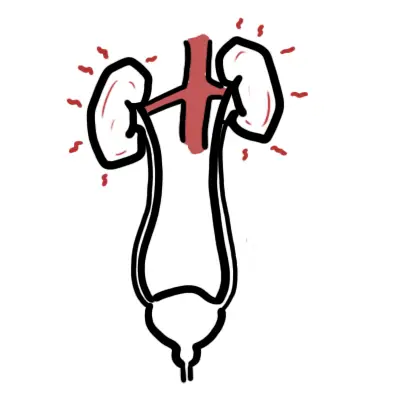
- Haematuria +/- blood clots
- Abdominal or flank mass
- Left sided scrotal varicoceles
- Inferior vena cava involvement
- Lower extremity edema
- Ascites
- Hepatic dysfunction (possibly related to a Budd-Chiari syndrome)
- Pulmonary emboli
- Paraneoplastic syndrome - many types
- Anaemia
- Constitutional symptoms - fever, nightsweats, weight loss
- Hypercalcaemia - Bone metastasis or paraneoplastic syndrome (PTHrP)
| Think Haematuria with blood clots are almost always due to nonglomerular bleeding. |
| Side note Up to 20% to 30% of RCCs present with paraneoplastic syndromes. |
Investigations
- FBC- anaemia
- EUC - renal function
- CMP - paraneoplastic syndrome or bone met association
- LFT - ↑ALP suggest bone mets?
- Ultrasound
- CT scan
Aetiology
- Family History - increases chance of RCC
- Von Hippel Lindau (VHL) syndrome
| Von Hippel Lindau (VHL) syndrome ~30% of VHL patients develop RCC. estimated 60% to 70% of patients with sporadic clear cell RCC also have VHL mutations. in VHL there is anactivation of one VHL allele (found on chromosome 3p); a second loss-of-function mutation is an early initiating event for VHL cancers such as RCC. |
Pathophysiology
Management
Surgery treatment
- Nephrectomy is performed unless bilateral tumours are present or the contralateral kidney functions poorly
Medical treatment Used for metastatic disease
- Interleukin-2 and interferon
- Medroxyprogesterone acetate
- Anti-VEGF
| Remember Chemotherapy is rarely used as tumours are not chemosenstitive. |
Complication and Prognosis
Prognosis
- Outcome following nephrectomy is unpredictable
- Tumours that are pathologically confined to the kidney confer a good prognosis
- Cure is likely if the tumour is <4cm in diameter and if there are no adverse pathological features
| Side note Periodic radiological follow-up is recommended in most cases so that locally recurrent or metastatic disease can be detected at an early stage. |