Overview
Overview 3% of population have renal stones. Renal stones is the commonest reason for emergency urological admissions. Its peak presentation is during the summer months (dehydration). 90% of urinary calculi are radio-opaque and so are able to be visualised through imaging.
| Definition Nephrolithiasis: Refers to the condition of having stones (calculi) in the kidney or collecting system. Urolithiasis: Refers to the condition of having stones (calculi) anywhere along the urinary tract. |
| Watch Video Urinary (Kidney) Stones - Overview |
Ureter Anatomy and Phsyiology
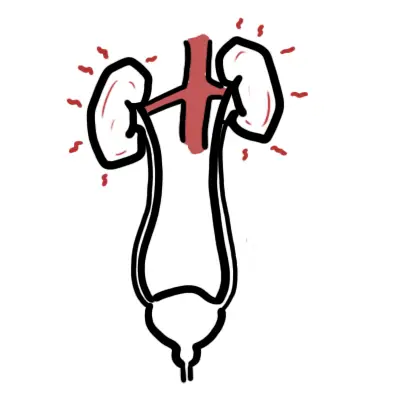
Sites of Contriction in the ureter
- Pelvi-ureteric junction - at its origin
- Pelvic brim - as it passess the external iliac artery
- Vesico-ureteric junction - before it enters the bladder
| Remember These sites are common sites where renal stones can get stuck. |
Risk Factors
| Composition of stone | Factors favouring stone formation |
| Calcium oxalate | Hypercalciuria, hyperoxaluria, hypocitraturia, and dietary risk factors such as a low calcium intake, high oxalate intake, high animal protein intake, high sodium intake. |
| Uric acid | Gout and diseases involving rapid cell turnover, such as leukaemias, lead to uric acid à uric acid stonesA low pH favours (chronic diarrhoeal states, gout, diabetes, obesity). |
| Cystine | Usually associated with a genetically determined defect in the renal transport of certain amino acids, including cystine |
| Magnesium Ammonium Sulphate (Struvite) | Persistent alkaline urine due to an UTI (Proteus or Klebsiella). |
| Common Risk Factors | Low fluid intake, previous nephrolithiasis, Family Hx of nephrolithiasis. |
Signs and Symptoms
Clinical Presentation
- Severe intermittent, stabbing pain radiating from loin to groin
- Microscopic haematuria (rarely macroscopic)
- Nausea/vomiting
- Fever
| Side note Struvite staghorn calculi classically present with recurrent UTIs. |
Examination
- Fever
- Tachycardia
- loin or renal angle tenderness
- Iliac fossa tenderness if the calculus has passed into the distal ureter
Differential Diagnosis
- Bladder carcinoma
- Aortic aneurysm
- Myocardial Infarction
- Acute Cholecytitis
- Ectopic pregnancy
- Mesenteric Ischaemia
- Appendicitis
- Acute pancreatitis
Investigations
- Urinalysis and MCS - Microscopic haematuria is seen in the majority of patients with renal stones. Assess level of calcium, uric acid, oxalate and citrate
- FBC and differential - Raised WBCs may suggest pyelonephritis/UTI/pyonephrosis (infection above obstructed stone).
- EUC
- Include sodium, potassium, chloride, bicarbonate, creatinine, urea, calcium, uric acid, and phosphorus.
- Assesses renal function
- Hypercalcaemia may suggest hyperparathyroidism as an underlying aetiology
- Hyperuricaemia may indicate gout
- Urine b-HCG (female) - exclude ectopic
- Plain abdominal X-ray: calculi that contain calcium are radiodense
- Renal ultrasound
- Non-contrast helical CT
Renal Stone
- Renal stones are crystalline mineral depositions that form from microscopic crystals in the loop of Henle, distal tubules, or the collecting duct.
- This is usually in response to:
- Elevated levels of urinary solutes such as calcium, uric acid, oxalate, and sodium.
- Decreased levels of stone inhibitors such as citrate and magnesium.
- Low urinary volume
- Abnormally low or high urinary pH.
- All of these can lead to urine supersaturation with stone-forming salts and subsequent stone formation.
- Calcareous stones account for more than 80% of stones. Uric acid stones represent about 5–10%, trailed by cystine, and struvite.
| Remember Approximately 80% of calcium kidney stones are calcium oxalate. |
Pathophysiology
The driving force behind stone formation is the supersaturation of urine.
- Ureteric colic from nephrolithiasis is secondary to obstruction of the collecting system by the stone.
- If the stone is sharp or larger than the normal lumen of the ureter (approximately 3 mm), it causes excessive distension of this muscular tube.
- The stretching of the collecting system or ureter is due to an increase in intraluminal pressure.
- This causes nerve endings to stretch and therefore the sensation of renal colic.
- The pain is referred to the cutaneous areas innervated by spinal cord segments and sensory ganglia, which also receive visceral afferents from the ureter, mainly T11- L2.
- A stone in the upper ureter typically causes pain in the loin, while a stone in the lower ureter typically causes pain in the loin and iliac fossa, with radiation to the testis or labia, or groin.
- The pain passes inferoanteriorly “from the loin to the groin” as the stone progresses through the ureter.
- Pain can also be due to local inflammatory mediators, oedema, hyperperistalsis, and mucosal irritation.
- Stones may collect anywhere from the collecting ducts to the urethra, but most common are:
- Pelvi-ureteric junction
- Pelvic brim
- Vesico-ureteric junction
Management
It is not necessary to treat every kidney stone. As a rule of thumb, the younger the patient, the larger the stone and the more symptoms it is causing, the more inclined we are to recommend treatment.
Treatment options for kidney stones
- Extracorporeal lithotripsy
- Percutaneous nephrolithotomy
- Open stone surgery
| Percutaneous nephrolithotomy is the removal of a kidney stone via a ‘track’ developed between the surface of the skin and the collecting system of the kidney. |
Acute management for ureteric stones
- NSAIDs or opioids
- Watchful waiting
- Emergency temporary relief
- Stent insertion
- Percutaneous nephrostomy (if infection)
| Indication for intervention to relieve obstruction and/or remove the stone |
| Pain |
| Bacteriuria |
| Fever |
| Impaired renal function |
| Prolonged unrelieved obstruction |
| Social reasons |
| Remember Almost 70% of stones 5mm or less and almost 50% of stones 6–10mm in diameter will pass spontaneously over a period of 3–6 weeks or there- abouts. |
Treatment for ureteric stones
- Extracorporeal lithotripsy
- Ureteroscopy
- Percutaneous nephrolithotomy
- Open ureterolithotomy
- Laparoscopic ureterolithotomy
- Percutaneous antegrade ureteroscopy
Treatment of bladder stones
- Removed via cystoscopy
Prevention of future stones
- Education about risk factors
- Drink more water
- Eating foods and drinks in calcium is good, rather high calcium intake is associated with a low risk of stone formation
- ↓sodium intake
- ↓animal proteins
- ↓alcohol
- ↑vegetables
- ↓thiazide diuretics
Complications and Prognosis
Complications
- Recurrent UTI
- Recurrent calculi
- Obstruction
- Trauma