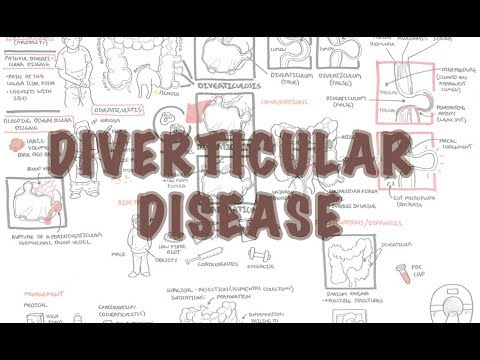
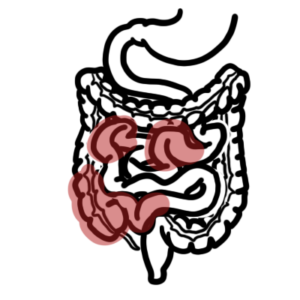
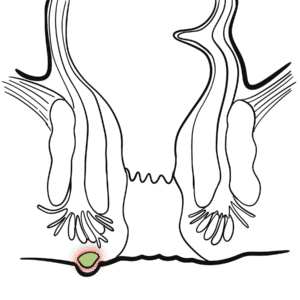
0:00 Hello, in this video, we're going to talk about hemorrhoids, anal hemorrhoids. 0:08 This is an overview and introduction. 0:11 Now, hemorrhoid plexi are normal anatomical structures located within the anal 0:17 canal. 0:17 If the hemorrhoid plexi enlarge, they can protrude outside the anal canal, 0:22 causing symptoms. 0:25 It is important to note that hemorrhoid plexi essentially are the veins, the 0:30 rectal veins, 0:31 forming a plexus. 0:33 So when we think of hemorrhoids, we have to remember veins. 0:36 Now, let's compare the normal with the abnormal. 0:41 We need to review the anatomy. 0:45 So the pectonite line, also known as a dentate line, is a clinically important 0:49 landmark. 0:50 Due to the fact that it is visible and approximates the level of certain 0:55 anatomical changes. 0:57 And these changes I'm talking about are embryological in origin. 1:01 So anything above the pectonite line, we say, is endoderm in origin. 1:07 And anything below the pectonite line is ectoderm in origin. 1:11 And why does this matter? 1:13 Well, if it's endoderm in origin, which is above the pectonite line, it means 1:17 that 1:18 it's essentially part of the abdominal organs. 1:20 And so pain could be very diffuse and not really localized. 1:26 However, if it's an ectoderm in origin, so the cells below the pectonite line, 1:33 ectoderm 1:34 in origin means essentially the skin. 1:36 And as we know, our skin is very sensitive. 1:39 So when pain occurs below the pectonite line within the ectoderm area, this 1:44 will cause 1:46 very localized pain and quite painful pain for that matter. 1:53 There are muscles also surrounding the anal canal. 1:57 These are the internal sphinteric muscles, which is controlled involuntarily. 2:02 And then the external anal sphincter, which is under voluntary control. 2:06 The levato ani is another important muscle that makes up the pelvic floor. 2:12 Hemroid plexi, plexuses, or plexi, are here. 2:16 And there is an external and internal hemorrhoid plexus. 2:20 And again, these are normal anatomical structures. 2:24 In the condition known as hemorrhoids, these plexi enlarge and can cause some 2:30 serious discomfort. 2:32 The enlargement can be from external hemorrhoids or from internal hemorrhoids. 2:38 And internal hemorrhoids are located above the pectonite line. 2:45 The side and symptoms of hemorrhoids differ a bit depending if it's an external 2:49 hemorrhoid 2:50 or if it's an internal hemorrhoid. 2:53 An internal hemorrhoid can often be painless, but there can be a feeling of 2:57 rectal fullness 2:58 or discomfort and mucus discharge. 3:02 Internal hemorrhoids are quite painful, they can cause sudden, severe peri anal 3:07 pain and 3:08 a peri anal mass might be felt. 3:11 And there can be pain on defecation, particularly if the thrombosis occurs 3:17 within the external 3:18 hemorrhoids. 3:19 And again, it makes sense because external hemorrhoids are below the pectonite 3:24 line. 3:24 And as we know, below the pectonite line is ectodermin origin and so it's very 3:29 well 3:30 localized pain. 3:33 The risk factors for developing hemorrhoids include increased intra-abdominal 3:38 pressure, 3:39 severe constipation, pregnancy, obesity, portal hypertension and heavy lifting. 3:46 All of these essentially cause some form of increase in intra-abdominal 3:51 pressure, which 3:52 means more pressure within the abdominal cavity. 3:57 When you have more pressure, the veins must overcome this pressure as it drains 4:03 back through 4:03 the abdominal cavity. 4:05 And because there's so much pressure in the abdominal cavity, these veins 4:10 enlarge. 4:11 And the veins being, in this case, the rectal veins, they enlarge. 4:16 So we learned about the signs and symptoms and the risk factors of hemorrhoids. 4:21 One examination, we want to position the patient in the left lateral position 4:27 and needs up 4:27 to the chest to expose the anal area. 4:30 And on general inspection, external hemorrhoid may be visible. 4:35 However, the use of a proctoscope or an anoscope might be useful to examine for 4:41 internal hemorrhoids. 4:44 Hemorrhoids can also be staged. 4:46 The internal hemorrhoids can be staged from one to four. 4:51 And it is important to stage because this means treatment will also differ. 4:58 Looking more closely at the anatomy, the middle rectal vein and the inferior 5:02 rectal vein drain 5:04 the anal area. 5:07 The middle rectal veins drain into the inferior mesenteric vein. 5:12 And the inferior rectal drains eventually into the inferior vena cava through 5:18 the pudendal 5:19 vein. 5:23 And of course, we have to remember the pectinate line or the dentate line. 5:27 The internal hemorrhoid plexi above the pectinate line and the external hemorrh 5:33 oid plexa lies 5:34 below the pectinate line. 5:37 The internal hemorrhoids, stage one, there is slight enlargement of the 5:42 internal hemorrhoid 5:43 plexus. 5:46 Stage two, the hemorrhoid can go past the pectinate line. 5:55 Stage three, further protruding down where it is visible in the anal sphincter. 6:02 And stage four is where the hemorrhoid has fully protruded out. 6:08 In an external hemorrhoid, as mentioned, the pain is there because the cells 6:12 around the 6:13 area are from an ectodermal, embryological origin, thus causing pain. 6:19 The pain is even more severe when thrombosis of the external hemorrhoids occur. 6:26 External hemorrhoids with thrombus can be very painful but often resolved 6:30 within two weeks. 6:32 And they often also leave skin tags. 6:41 So let's look at treatment now. 6:44 Treatment for stage one in two internal hemorrhoids consists of high fiber diet 6:49 , a sits bath. 6:50 And a sits bath is a warm, shallow bath that cleanses the perineum, which is 6:56 the space 6:56 between the rectum and the genital area. 7:02 Steroid creams and promoxin can also be used. 7:07 Promoxin is an aesthetic and an anti-proritic agent, so anti-itching. 7:15 Four stage three and four rubber band ligation can be done. 7:20 And a rubber band ligation is essentially a procedure in which the hemorrhoids 7:25 are tied 7:25 off at its base with rubber bands. 7:28 And this will cut off the blood supply. 7:31 Other options include photo-quadulation, where infrared light is used to break 7:36 down the hemorrhoid. 7:38 Hemoidectomy can also be performed, which is essentially cutting the hemorrhoid 7:42 out.