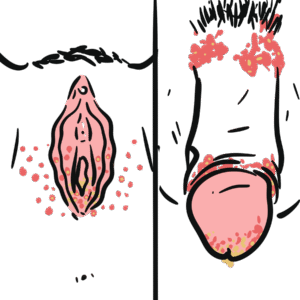
0:00 The human immunodeficiency virus, or HIV, is a retrovirus that infects CD4-T 0:16 lymphocytes 0:18 among many other cells, leading to the destruction of these CD4-T cells, and 0:24 thereby impairing 0:26 cell-mediated immunity and increases the risk of cancer and opportunistic 0:32 infections. 0:37 HIV-1 is the most common species worldwide. HIV-2 is restricted almost 0:47 completely to West Africa. 0:50 The structure of the virus is that it's a acosahedral, meaning a polyhedron 0:57 with 20 faces, 0:59 with a conical capsid, a protein shell of a virus. 1:05 The capsid contains two strands of RNA. 1:13 The capsid also contains two enzymes, essential for HIV replication. 1:19 The integrase and the reverse transcriptase. 1:24 The capsid also contains two strands of RNA, which holds the HIV's genetic 1:30 material. 1:32 HIV's RNA is made up of nine genes, which contain all the instructions to make 1:38 new viruses. 1:40 Three of these genes, gag, poll, and n, provide the instructions to make 1:47 proteins that will form the new virus particles, 1:51 consisting of the core proteins, the enzymes, and the envelope glycoprotein. 1:57 The outer shell of the virus is called the envelope, and is made up of lipid 2:02 layers, 2:03 which are covered in spikes of the glycoproteins I mentioned. 2:08 Here you can see glycoproteins GP41 and GP120. 2:14 These glycoproteins allow the HIV to lock onto the CD4 receptors on the CD4T 2:22 cells and enter the cell. 2:27 So let's take a look at how the virus does this, and also learn about the life 2:32 cycle of the HIV virus, 2:36 by looking at some key steps. 2:39 The HIV virus gains entry into the cell following sexual intercourse, which is 2:44 a major cause. 2:46 Once the virus is within the body, they will infect immune cells which have CD4 2:51 receptors on the surface. 2:53 The main cells here contain the CD4 receptors, are the CD4T lymphocytes. 3:00 When HIV makes contact with a CD4 cell, the GP120 spike on the surface of the 3:07 HIV lock onto the CD4 receptor, 3:11 and another co-receptor, CCR5, or CXCR4. 3:20 This first step is called attachment, and this step essentially will result in 3:25 the fusion of the viral membrane with the cell membrane. 3:29 The second step of the life cycle is fusion. 3:35 The process of fusion allows the HIV capsid to enter the CD4 cell. 3:42 The GP41 protein is used to fuse the HIV envelope with the cell wall. 3:49 The capsid releases the viral RNA, the reverse transcriptase, and the integrase 3:56 as well. 3:57 The third step is reverse transcription. 4:01 Here the HIV uses its reverse transcriptase enzyme to convert the RNA it 4:06 contains into a pro-viral DNA inside the cell. 4:12 So now you have the double-stranded blue DNA, which is the viral DNA. 4:17 Once this is done, the next step is integration. 4:22 The HIV's integrase enzyme attaches itself to the end of the pro-viral DNA 4:28 strands, and carries the viral DNA into the cell nucleus. 4:33 Once the pro-viral DNA enters the cell nucleus, it binds to the host DNA, and 4:39 then the HIV DNA strand is inserted into the host cell DNA. 4:46 After the pro-viral DNA is integrated into the DNA of the host, HIV either 4:51 continues to use the body's own cell machinery to replicate, 4:55 or it will remain dormant within the cellular DNA. 5:00 This stage is called latency, and the cell is described as "latently infected". 5:10 The next step is transcription. When the cell becomes active, the HIV uses the 5:18 host enzyme RNA polymerase to read the HIV gene to make messenger RNA and 5:22 genomic viral RNA. 5:25 This is called transcription. 5:29 Focusing on the mRNA, the next step is translation. 5:37 The messenger RNA provides the instructions for making new viral proteins, 5:42 including structural proteins, and the viral enzymes. 5:46 The viral genomic RNA and these viral proteins will prepare to be assembled. 5:54 In assembly and release, what happens is the enzymes and the HIV RNA will begin 6:00 to assemble into the new viruses at the cell wall. 6:04 After the new virus is assembled, it must leave the cell by pushing through the 6:09 cell wall. 6:10 The virus must take lipids, the fat from the cell wall, to make the surface gly 6:15 coproteins, including the GP120 and the GP41. 6:20 Shortly after the virus is released from the cell, the viral protease actually 6:26 cleaves some of the precursor proteins, which will help form the mature capsid 6:31 as we know it. 6:32 This makes the virus mature and infectious. The cycle can continue. This HIV 6:38 virus can then infect other people or infect other cells. 6:44 The root of transmission of the HIV virus is via sexual intercourse, majority 6:50 of cases. It can also be transmitted parentially, so through the blood, or 6:56 vertical transmission from mother to baby. 7:01 So we looked at the life cycle of HIV and how it infects a CD4 T cell, and how 7:07 it also replicates within these cells. 7:10 But what does the body actually do when HIV infects the CD4 T cell? How does 7:17 the body's immune system respond to the HIV infection? 7:23 Next, we will focus on the pathophysiology and the natural history and 7:28 progression of HIV. 7:30 So what happens is you have these dendritic cells, which are the first to 7:35 recognize a HIV virus, and present them to the immune system to mount an immune 7:41 response. 7:42 What they do is that they engulf the virus, process them, and then present them 7:48 on their cell surface via a MHC class II. 7:52 They then travel to the lymph nodes and what's called the galt gastric- 7:56 associated lymphoid tissue, carrying this viral particle, where they activate or 8:03 stimulate CD4 T lymphocytes. 8:08 The CD4 T cell will then activate B cells and plasma cells to produce 8:12 antibodies against HIV. CD4 T cells will also activate CD8 T cells, also known 8:19 as the cytotoxic T cells. 8:24 During this time, the HIV continues to infect cells. The only cells that can be 8:28 infected by the HIV virus are those that have the CD4 receptor. 8:34 These cells, as mentioned, are the monocytes, macrophages, dendritic cells, 8:40 microglial cells, but more specifically, the T lymphocytes. 8:45 The greatest concentration of these cells is in the gut-associated lymphoid 8:50 tissue and lymph nodes. 8:52 As the virus replicates within the CD4 T lymphocytes, it kills the cells and 8:57 spreads again. 8:59 About three to four weeks after the initial infection, the HIV viral load 9:05 increases and is detected. 9:08 The HIV P24 antigen is also detectable. 9:13 The HIV antibody is detectable in weeks two to four, roughly. 9:19 And once this occurs, this is called seroconversion. 9:24 When you get seroconversion, where you get presence of the antibodies, as well 9:27 as you get this increase in the viral load, this causes what's called serocon 9:32 version sickness or seroconversion illness, which manifests as symptoms of acute 9:38 HIV infection. 9:40 Interestingly, these symptoms are very non-specific, and they include fevers, 9:46 fatigue, myalgia, rash, headache, pharyngitis, and lymphadenopathy. 9:52 Really, symptoms of a standard viral infection which vary and are self-limiting 9:59 and go away by up to two weeks. 10:02 So in summary, the acute infection, which are in the first weeks, causes an 10:09 increase in viral load of the HIV virus. 10:13 You get the presence of HIV P24 antigen. 10:17 You get presence of the antibodies against HIV, which actually begin to appear 10:22 between weeks two and four. 10:24 And you also get the CD8 T cell being activated. 10:31 In this period, you also get seroconversion illness, which can be very mild and 10:38 even go unnoticed. 10:41 Only a small proportion of the infected CD4 T lymphocytes allow the virus to 10:47 replicate and, you know, get released again. 10:52 These infected T lymphocytes usually express MHC class 1 molecules with the 10:58 viral antigen, which essentially tags them so that they are recognized as an 11:04 infected cell, 11:05 which allows the cytotoxic CD8 T lymphocyte to destroy them, controlling the 11:12 infection. 11:14 Unfortunately, as the HIV infects more and more CD4 T lymphocytes, they are 11:20 able to form mutations in their genetic material, 11:24 which allow them to evade the immune system, hide from the immune system. 11:29 And they do this by down-regulating the MHC class 1 expression, essentially 11:33 making it unrecognizable by the immune system. 11:37 HIV hides within CD4 cells, where they remain dormant. 11:43 HIV infection will not really cause further illness for some years. 11:50 And this period is known as the asymptomatic phase, which is roughly about 10 11:57 years. 11:58 HIV infected C4 remains dormant and slowly reduces the CD4 T cell count. 12:07 The viral load of the HIV remains steady, because the CD8 T cell, the cytotoxic 12:14 T cell, keeps their numbers in circulation at bay. 12:20 In the asymptomatic phase, the viral load and HIV antibodies are detectable, 12:26 and remember, the CD4 count will slowly go down here. 12:31 During the asymptomatic phase, CD4 T cell count and viral load tests can 12:36 monitor the progression of the HIV disease. 12:41 Looking at the two stages we have learned so far, using this graph, with time 12:47 on the x-axis, 12:49 we can see the viral load will increase in the first few weeks during the acute 12:54 infection, 12:55 but then drop and remain relatively stable, because the immune cells, such as 13:00 the CD8 cytotoxic T cell, keeps it in check for around 10 years. 13:05 This is the asymptomatic phase. Until eventually, after about 10 years, if left 13:11 untreated, the viral load will begin to increase. 13:17 Looking at the CD4 cell count, from day one of infection, the CD4 cell count 13:24 slowly dwindles, because as we have learned, the HIV infects CD4 cells, such as 13:31 the CD4 T cells, 13:33 and slowly causes them to die during the asymptomatic phase. 13:39 Here you have seroconversion illness, where the body begins producing 13:43 antibodies. 13:44 The B cells, plasma cells begin producing antibodies by weeks 2 to 4, of the 13:50 initial infection. 13:52 The CD8 T cells are created to destroy the HIV infected cells. 13:58 HIV levels begin to fall in the blood, because of this, and after a few weeks 14:04 to months, the viral load and CD4 levels will stabilize at a level known as the 14:11 set point. 14:13 HIV gradually reduces the number of CD4 T cells in the body, until the CD4 cell 14:20 count falls below 200 cells per millimeters cubed. 14:26 When the T cell count is this low, they are at risk of developing AIDS, also 14:34 known as acquired immunodeficiency syndrome. 14:39 AIDS is defined by a CD4 cell count of less than 200 cells per millimeters cub 14:45 ed, or if they develop an AIDS-related illness. 14:50 When someone has AIDS, their risk of infection increases, their risk of malign 14:55 ancy increases, as well as other comorbidities. 14:59 AIDS-defining infections are very important. 15:03 Once the CD4 cell count drops below 200, you are likely to develop certain 15:08 infections. 15:10 Some infections develop at a much lower CD4 cell count. 15:15 People with a CD4 cell count below 500 also develop AIDS-defining illnesses, 15:21 including carposis, sarcoma, invasive cervical cancer, and tuberculosis. 15:27 I have a separate video that goes into a lot of detail into the AIDS-defining 15:31 illnesses. Please have a look. 15:35 Let's talk about screening and diagnosis of HIV. 15:39 What you do is, if you suspect someone has HIV, you can do what's called a 15:42 combination assay, which is basically looking at the HIV antibody, as well as 15:47 the presence of the P24 antigen. 15:51 If positive, you can do what's called the antibody differentiation assay, which 15:58 essentially will tell you which type of HIV the person has, either HIV1 or HIV2 16:05 . 16:06 If the combination assay is negative, meaning there's no HIV antibodies present 16:11 , you can check the HIV viral load by looking at the HIV RNA nucleic acid 16:19 amplification test, or NAAT. 16:24 If the viral load is positive, you can also diagnose HIV, because they have 16:29 viruses in the blood. If the viral load is negative, then this person does not 16:34 have HIV at that particular time. 16:37 Other investigations for HIV, one's confirmed. Firstly, you always want to get 16:43 the viral load by looking at the HIV RNA, and this is to look at a baseline, 16:49 also performing T cell subsets to establish a CD4 cell count. 16:54 You can also perform viral resistant testing at baseline. For blood count, EUC 17:07 's LFT glucose, fasting lipids, check for latent TB, performing a tuberculine 17:10 skin test, and interfere on gamma release assay. 17:12 Hepatitis viral serology, serology for syphilis and other sexual transmitted 17:21 infections, serology for toxoplasmosis, as well as cervical pap smear. 17:28 The management of HIV just briefly. Education is very important. Again, the 17:33 infection is treatable, and a person can have a normal life. Educate them on 17:39 safe sex condoms, as well as educating them on the complications of the disease 17:45 and the medications. 17:47 Treatment involves antiretroviral therapy, and it's important to treat the 17:53 person right away, and it is lifelong treatment. 17:58 Monitor for complications, specifically opportunistic infections that may arise 18:03 , AIDS-defining illnesses, as well as medication side effects. 18:08 I will have a separate video that will focus on the pharmacology of HIV, and I 18:13 'll put the link at the end of the video. 18:16 In summary, HIV is a virus that essentially infects CD4 cells, such as your CD4 18:24 T cells, and what they do here is that they replicate within the cells, or they 18:29 can remain dormant. 18:31 What they will do over time is that they will deplete the CD4 count, and when 18:36 the CD4 count is depleted, it will increase the risk of opportunistic 18:41 infections. 18:43 Treating person with HIV early with antiretroviral therapy is important. Thank 18:47 you for watching.