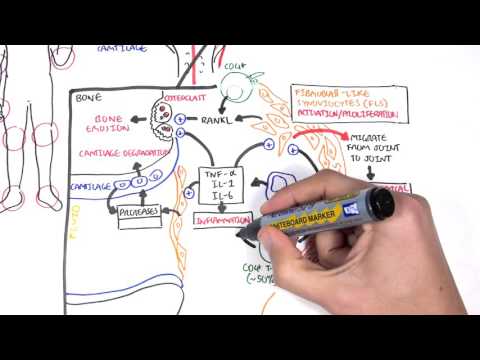
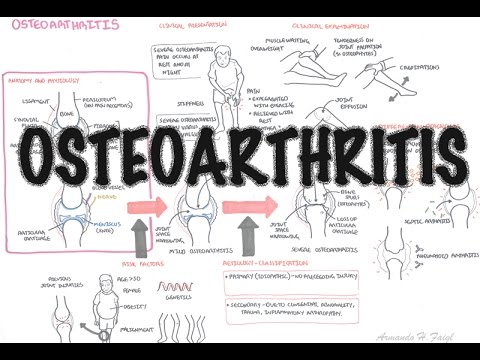
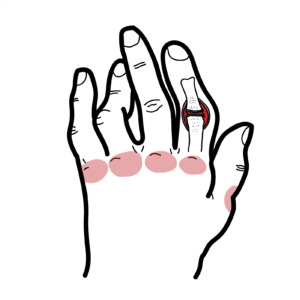
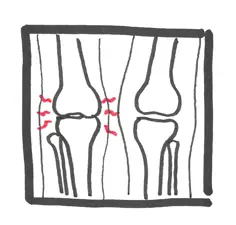
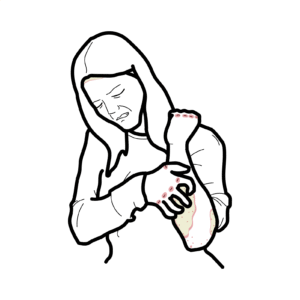
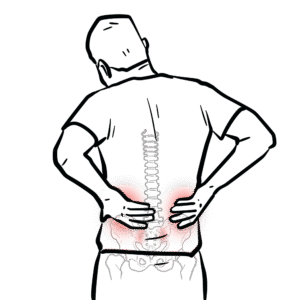
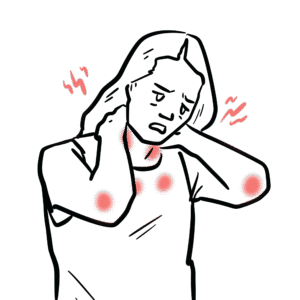
0:00 In this video, we're going to talk about the differences between inflammatory 0:07 arthritis 0:08 and non-inflammatory arthritis. 0:11 In this video, we will compare osteoarthritis, which is a typically non- 0:15 inflammatory arthritis 0:16 to rheumatoid arthritis, a very common inflammatory arthritis. 0:21 Let us review a normal synovial joint, which is the most common type of joint 0:25 found in 0:25 the human body. 0:26 An example of a synovial joint is the knee. 0:30 Now the synovial joint here consists of two bones. 0:35 The articulating surface of the joint now contains cartilage. 0:41 Cartilage minimizes friction on joint movement and also acts as a shock absor 0:47 ber. 0:48 The joint has a capsule, this surrounding structure consisting of an outer fib 0:53 rous pot 0:53 and an inner synovial layer called the synovial membrane. 0:58 The synovial membrane is actually very important because it provides and 1:01 produces synovial fluid. 1:03 The synovial fluid located within the joint cavity of a synovial joint has 1:08 three primary 1:09 functions, lubrication. 1:11 It also distributes nutrients and acts as a shock absorber. 1:17 Let's take a look at now some features of non-inflammatory arthritis, which is 1:24 osteoarthritis. 1:26 Here is a hand of someone with osteoarthritis. 1:30 Looking into this osteoarthritic joint, there are some noticeable changes. 1:36 First of all, there is thinning of the cartilage, there is loss of joint space. 1:43 The loss of space triggers bone cells to grow and form osteocytes. 1:50 There is sub-condrel sclerosis where the area below the cartilage becomes hard 1:56 and compacted. 1:57 And you can also find something called sub-condrel cysts, which are really 2:02 fluid-filled sacs within 2:03 the bone. 2:05 These changes cause the features we see in a hand and in a joint of someone 2:11 with osteoarthritis. 2:13 Inflammatory arthritis on the other hand, such as rheumatoid arthritis is much 2:18 more aggressive 2:19 and can cause deformities if not treated appropriately. 2:23 Here are hands of someone with advanced rheumatoid arthritis. 2:29 A joint that is actively inflamed can cause bone erosions eventually. 2:34 There is inflammation and thickening of the synovial membrane, causing a tender 2:41 , painful 2:42 and red joint. 2:43 In rheumatoid arthritis, interestingly, the distribution of inflammation is 2:47 symmetrical, 2:49 involving the knuckles, the metacarpophalangeal joints and the proximal inter 2:54 phalangeal joints. 2:55 The inflamed synovial membrane produces more synovial fluid in the joint space, 2:59 causing 2:59 the joint to swell up. 3:01 There is an increased number of inflammatory cells such as neutrophils to the 3:05 area. 3:06 Every time the inflammation damages the cartilage causing thin cartilage, as 3:10 well as significant 3:12 damage and bone damage. 3:16 Typical features that differentiate osteoarthritis from rheumatoid arthritis. 3:21 First of all, osteoarthritis pain typically involves really any joint, but 3:26 typically the 3:27 distal interphalangeal joint, proximal interphalangeal joint, and first, copper 3:32 metacarpal 3:33 joints, although again, it can occur anywhere with overuse. 3:38 Bone growth can occur at specific sites, including the distal interphalangeal 3:42 joints. 3:43 These are called hembadins nodes, and at the proximal interphalangeal joints 3:47 called buschards 3:49 nodes. 3:50 In rheumatoid arthritis, the joints affected in the hands are namely the wrist, 3:54 the metacarpophalangeal 3:56 joint, and the proximal interphalangeal joint. 3:59 Over time, you can get ulna deviation and something called Z-deformity of the 4:07 thumb. 4:08 Now those are some visual features that differentiate osteoarthroid or 4:12 inflammatory arthritis. 4:13 Let us take a look at other features that differentiate between the two. 4:20 First of all, prolonged morning stiffness is typically absent in osteoarthritis 4:26 and 4:26 present in rheumatoid arthritis. 4:29 Pain is more prominent at the end of the day with osteoarthritis, and in the 4:34 morning 4:34 with rheumatoid arthritis. 4:37 Swelling of joints is described as bony in osteoarthritis, whereas swelling in 4:41 inflammatory 4:42 arthritis causes soft tissue swelling. 4:45 Over the joint of osteoarthritis, there is absent erythema, which is redness 4:49 and warmth. 4:50 While in rheumatoid arthritis, it is common to have redness and warmth during a 4:57 flare. 4:57 Systemic features are absent in osteoarthritis, whereas in rheumatoid arthritis 5:01 , there can 5:02 have other features such as fevers, red eyes, fatigue, low-grade fevers. 5:11 When fluidists take an out of a joint of someone with osteoarthritis, there is 5:15 typically 5:15 less than 2,000 white cell counts per area, whereas in rheumatoid arthritis and 5:20 other 5:20 inflammatory authorities, the white cell count is greater than 2,000 during a 5:26 flare. 5:26 Blood tests are also a good differentiator. 5:29 In osteoarthritis, inflammatory markers such as C-reactive protein and erythro 5:35 cyte sedimentation 5:36 rate are normal, whereas in rheumatoid arthritis, they are present and elevated 5:41 and obviously 5:42 elevated during a flare. 5:45 So in summary, this video provides an overview of the key differences between 5:49 non-inflammatory 5:50 and inflammatory arthritis, specifically focusing on osteoarthritis and rheumat 5:54 oid arthritis 5:55 through the examination of the joint structure, symptoms and very important 6:00 features. 6:00 Thank you for watching.