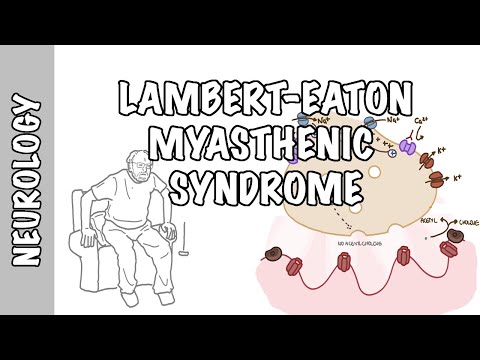
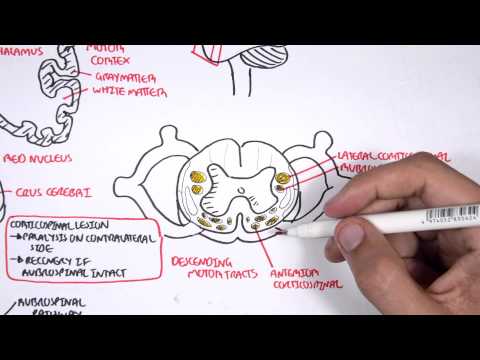
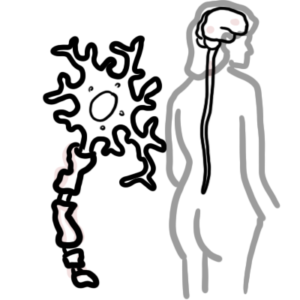
0:00 Myasthenia gravis is the most common disorder of neuromuscular transmission, it 0:10 is an autoimmune 0:11 disorder characterized by variable weakness involving the eyes, ocular, bulba 0:17 to do with 0:17 speech and swallowing, the limbs and their respiratory muscles. 0:23 The classic presentation is a fluctuating weakness that is more prominent in 0:27 the afternoon. 0:29 The autoimmune attack occurs at the communication between the motor nerve and 0:36 skeletal muscles. 0:37 This area is called the neuromuscular junction. 0:45 The end of the motor nerve is the terminal bulb which houses vesicles 0:51 containing acetylcholine, 0:52 A-C-H. Normally when an action potential arrives at the terminal, the influx of 1:00 sodium ions 1:01 through voltage-gated sodium channels causes depolarization and opens voltage-g 1:07 ated calcium 1:08 channels. 1:10 Calcium influx triggers the release of acetylcholine into the neuromuscular 1:16 junction. 1:16 Acetylcholine is a neurotransmitter which binds onto acetylcholine receptors on 1:21 the muscle 1:21 fibres. 1:23 This causes an influx of sodium ions into the muscle which eventually causes 1:29 muscle contraction. 1:33 Once muscle contraction occurs, acetylcholine is broken down into acetylcholine 1:38 and choline 1:38 which gets recycled to make more acetylcholine for the nerve. 1:42 The cycle continues. 1:51 There is another important receptor called the musk receptor which stimulates 1:56 the expression 1:57 of acetylcholine receptor. 1:59 So when you have more acetylcholine receptor this allows for more acetylcholine 2:04 binding 2:04 and therefore muscle contraction. 2:12 Myosyrogravus is an acquired autoimmune disorder of the neuromuscular junction 2:18 characterized 2:19 by weakness and fatigueability of skeletal muscles. 2:23 The exact etiology is unclear but one theory is an association with hyperpl 2:28 astic thymus 2:29 or a thymoma which is a tumor from the thymus gland. 2:35 Automunity occurs here at the T cell and B cell co-stimulation which results in 2:40 the development 2:41 of antibodies against acetylcholine receptors, the ACHR. 2:47 Acylcholine receptor antibodies are the most common antibodies found in myosy 2:53 rogravus and 2:54 it's associated with the thymoma we mentioned and have a strong ocular 2:59 involvement which 3:01 we will talk about. 3:03 The antibodies bind to the acetylcholine receptor and cause an antibody 3:09 mediated complement attack. 3:11 The complement attack means that they will activate complement protein, a 3:16 series of proteins 3:17 important in triggering and promoting the immune response. 3:21 So the complement activation and the immune attack will reduce the number of 3:27 acetylcholine 3:28 receptors and the destruction of the acetylcholine receptors over time will 3:34 lead to muscle 3:35 fatigueability and weakness. 3:42 Myosyrogravus can also be caused by certain medications. 3:46 Penicilamine induces the production of acetylcholine receptor antibodies. 3:51 Other medication causing myosyrogravus which has been found include chloroquine 3:57 which is 3:57 an antiparasitic agent and quinidine and antiarithmic. 4:04 Some patients with myosyrogravus who are seronegative for acetylcholine 4:10 receptor antibodies meaning 4:12 that they don't have acetylcholine receptor antibodies, they have antibodies 4:18 directed against 4:18 another target on the surface of the muscle membrane. 4:22 This is the muscle specific receptor tyrosine kinase or musk for short which we 4:29 mentioned. 4:30 Now musk receptor antibodies will attack the musk receptor and therefore reduce 4:37 acetylcholine 4:39 receptor expression. 4:45 Most receptor antibodies have no thymoma association and are common in females 4:52 and bulba and ocula 4:53 involvement is common. 5:00 Clinical features of myosyrogravus, clinically myosyrogravus can be divided 5:05 into three types. 5:07 Oculomyosyrogravus which only involves the eyes, generalize myosyrogravus which 5:11 is more 5:12 predominantly the limbs, so weak arms and feet and legs or an overlap between 5:17 the two. 5:20 Features of oculomyosyrogravus include ptosis and diplopia from the oculomus 5:26 being affected. 5:28 Myosyrogravus may also be remembered associated with thymomas particularly if 5:32 they have acetylcholine 5:34 receptor positive antibodies. 5:38 This is often present with proximal muscle weakness which is fatigable. 5:43 This is more so for generalize myosyrogavus. 5:46 And then you have also respiratory muscle weakness, bulba involvement which 5:53 causes weakness 5:54 of the muscles in the throat leading to dysarthria, dysphagia, difficulty 5:59 swallowing and fatigue 6:00 ability. 6:03 Interestingly myosthenia crisis is a medical emergency characterized by severe 6:09 weakness 6:10 involving bulba and respiratory muscles requiring intubation or non-invasive 6:17 ventilation. 6:18 Because myosyrogavus is an autoimmune disease there is an association with 6:22 other autoimmune 6:23 diseases including thyroid disease, shrogan syndrome and systemic lupus eryth 6:32 matosis. 6:33 Most clinicians feel that there are three stages to the disease that is myost 6:37 henia gravis. 6:39 There is an active phase with the most fluctuations and the most severe 6:44 symptoms that occurs in 6:45 the five to seven years after onset. 6:50 Most myosthenia crisis occurs in this early period. 6:55 This is typically followed by a more stable second phase and in this phase the 7:00 symptoms 7:00 are stable but persists. 7:03 They may worsen in the setting of infection, medication tapering or a surgery. 7:10 In many patients though this is followed by the third phase in which remission 7:16 may occur 7:18 with the patients free of symptoms of any therapy or even off medications 7:25 entirely. 7:27 So what are the investigations to order when someone has suspected myosthenia 7:31 gravis. 7:32 There's this thing called the ice pack test. 7:34 Basically the test is based on the physiological principle that neuromuscular 7:40 transmission 7:40 improves at lower muscle temperatures. 7:45 And so placing ice over the eye for five minutes improves the ptosis 7:50 temporarily. 7:51 There's a test called the endrophonium test also known as the tensilone test. 7:57 This is used to diagnose myosthenographis before acetylcholine receptor 8:02 antibody test 8:02 became the common method. 8:05 The endrophonium is a short-acting acetylcholinesterase inhibitor. 8:10 So symptoms improve rapidly after the administration of this drug. 8:17 EMG is also very important which assesses basically the muscles and the nerves. 8:23 So with repeated stimulation of the nerve it will produce a decrementing 8:29 amplitude because 8:30 the muscle becomes fatigable. 8:33 There are serological tests to order. 8:35 So the first most important one is the presence of acetylcholine receptor 8:41 antibodies which 8:41 is seen in 85% of cases of patients with myosthenia gravis. 8:46 This is usually associated with ocular generalized or overlap myosthenia gravis 8:53 with varying severity. 8:56 There is also musc antibodies which is present in 8% of cases of myosthenia 9:01 gravis. 9:02 Musc is often associated more so with generalized myosthenia gravis. 9:09 There's presence of also the LRP for antibody which is only found in 1% and 9:14 this is usually 9:15 associated with mild symptoms. 9:19 There's also seronegative myosthenia gravis which is surprisingly quite common 9:24 6% of cases. 9:26 It's really similar presentation to someone with seropositive myosthenia gravis 9:31 . 9:31 However, more likely to have purely ocular disease so eye disease, ptosis and 9:37 whatnot 9:38 and tend to have better response to treatment and outcome. 9:44 It's worth noting a condition that is a good differential for myosthenia gravis 9:50 which is 9:50 Lambert-Eton myosthenic syndrome. 9:53 And I will have a separate video on this that we'll talk about in more detail. 9:58 Speaking of differential diagnosis of myosthenia, again, Lambert-Eton syndrome. 10:05 Some fun facts. 10:06 It is a perineoplastic syndrome characterized by presynaptic antibodies against 10:11 voltage gated 10:12 calcium channels. 10:14 Botulism which is caused by Clostridium botulinum which produces a toxin that 10:20 inhibits presynaptic 10:22 acetylcholine release and therefore weakness. 10:26 Medication specifically amino glycosides may interfere with acetylcholine 10:30 transport across 10:32 the neuromuscular junction. 10:36 Another differential is Gilean barre syndrome which is an acute autoimmune 10:40 disease causing 10:41 demyelination of predominantly motor neurons. 10:46 Modern neuron disease is another differential. 10:48 It is a degenerative neurological condition affecting both lower and upper 10:54 motor neurons 10:55 resulting in muscle weakness. 10:58 The differential diagnosis of myosthenia gravis specifically only involving the 11:05 eyes so ocular 11:06 myosthenia include millifisher variant of Gilean barre syndrome, thyroid o 11:13 phthalmopathy, 11:15 even diabetes ophthalmopathy, as well as brainstem and motor cranial nerve 11:27 lesions. 11:29 Management of myosthenia gravis, so first and foremost, is awareness of 11:33 medications with 11:35 which may potentiate or worsen the symptoms of myosthenia gravis. 11:40 There is a role of thymectomy which is specifically if someone has myosthenia 11:47 gravis with acetylcholine 11:49 receptor positive antibodies. 11:54 Immunosuppressive agents are very important in the management of myosthenia 11:58 gravis and 11:58 really the main goal of immunosuppressive agents is to reduce the immune system 12:04 because 12:04 fundamentally it is an immune disease, it is an autoimmune disease and so the 12:09 most common 12:10 one is steroids which suppresses the lymphocytes through different mechanisms 12:17 and is used especially 12:19 during periods of exacerbations of myosthenia. 12:23 Other immunosuppressive agents include cyclosporin, an interleukin II inhibitor 12:27 which targets 12:28 T cells and as a thioprine which targets both B and T cells. 12:34 For myosthenia gravis with Bulba involvement, myosthenia crisis or when someone 12:40 does not 12:41 respond to those immunosuppressive agents I mentioned earlier, agents such as 12:47 intravenous 12:48 immunoglobulins can be used which aims to normalize the immune system and 12:53 plasma feresis 12:54 which aims to remove the plasma containing the antibodies and then replacing 13:00 this. 13:00 However, probably the most important one, first line in someone who has 13:05 symptoms of 13:05 myosthenia gravis is acetylcholineasterase inhibitors such as oral pyrostigmine 13:11 which 13:12 really aims to keep acetylcholine in the neuromuscular junction so that it can 13:18 promote contraction. 13:20 In summary, myosthenia gravis is an autoimmune disorder characterized by 13:26 generalized weakness 13:26 and fatigueability worse in the afternoon. 13:29 There are prisons of anti-bodies against acetylcholine receptor. 13:33 It may be ocula involvement, generalized involvement or an overlap syndrome. 13:39 First line treatment is pyrostigmine and then other immunosuppressive agents 13:43 and phymectomy 13:44 may be warranted.