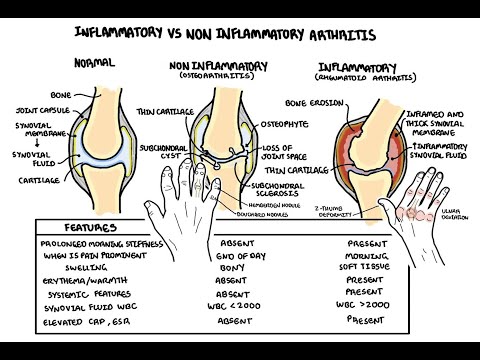
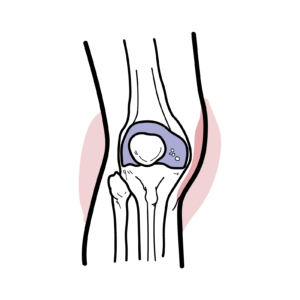
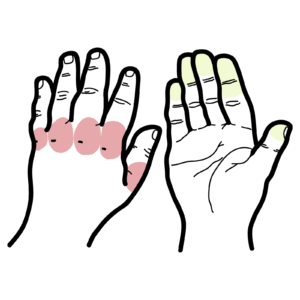
0:00 Hello, in this video, we're going to look at rheumatoid arthritis, which is a 0:09 systemic 0:11 rheumatological disorder affecting multiple joints. 0:16 The clinical presentation of rheumatoid arthritis is arthritis, which is symm 0:20 etrical. 0:21 We have pain, swelling, as well as nodules around the area. 0:25 That involvement is early in the disease, and affects the metacapa forangial 0:29 and proximal 0:30 interflangial joints. 0:33 In rheumatoid arthritis, there's also extroarticulate involvement, which we'll 0:38 look at later on. 0:39 But first, let us look at the hand involvement in rheumatoid arthritis, and see 0:44 how it differs 0:45 to osteoarthritis. 0:48 So here is rheumatoid arthritis and osteoarthritis. 0:51 So in osteoarthritis, the joints affected are the distal interflangial joints, 0:56 as well 0:57 as proximal interflangial joints, whereas in rheumatoid arthritis, it is the 1:01 proximal 1:02 interflangial joints and the metacapa forangial joints. 1:06 As well, you can have other joint involvement, such as the wrist. 1:12 So these joints are affected early in the disease in rheumatoid arthritis. 1:18 But as the disease progresses, you can have other features occurring in the 1:22 hands. 1:23 These are swanic, butoniae, or zediformity of the thumb. 1:28 So in swanic, what you have is you have the distal interflangial joints flexed. 1:35 But the proximal interflangial joints hyper-extended. 1:40 In butoniae, it's the opposite. 1:42 You have the distal interflangial joints hyper-extended, and the proximal inter 1:46 flangial joints flexed. 1:47 The zediformity of the thumb is essentially the thumb looking like a zed. 1:53 It's sort of bent, hyper-extended. 1:57 In the hands, the hands can also deviate medially. 2:00 This is referred to as ulna deviation. 2:05 So they were the features of the hands in rheumatoid arthritis. 2:12 Let us actually look at what happens inside the joints. 2:16 So let us zoom into a finger here. 2:19 And just to recap the anatomy, here we have the bone, the joint capsule, the 2:25 synovial membrane, 2:28 also known as a synovium. 2:30 The synovial membrane, also known as a synovium, which produces the synovial 2:35 fluid, which helps 2:36 in lubrication as well as supplying nutrients to the area. 2:40 Then we have the cartilage here in blue. 2:44 In rheumatoid arthritis, you essentially have inflammation of the synovial 2:50 membrane. 2:51 You have a sinovitis. 2:53 And this causes pain and swelling, which occurs in rheumatoid arthritis. 2:59 This also leads to bone and cartilage erosion, breakdown. 3:04 Another feature we can see in the joints of rheumatoid arthritic patients is 3:10 angiogenesis. 3:12 So that was the macroscopic view of the joint, just an overview. 3:16 Let's look at it in a lot more detail at a cellular level. 3:21 Let us zoom into this area and see what cells are involved. 3:26 So just to show where we are, here we have the bone, the synovium. 3:33 Here is the fluid here in yellow, and blue is the cartilage. 3:37 And again, I'm joined the synovium really big because it is inflamed, right? 3:43 The synovial membrane. 3:44 The synovial membrane is made up of the cells known as fibroblast-like synovial 3:51 sites. 3:52 And these guys are very important in the pathogenesis of rheumatoid arthritis. 3:58 So again, rheumatoid arthritis is where we have inflammation of the synovial 4:01 membrane, 4:02 of the synovium. 4:04 Now the exact trigger of the inflammation of the disease is really not quite 4:13 known. 4:14 However, we are now looking at what cells we can find here and what cells are 4:19 involved. 4:20 So we have macrophages here, and they're normally around here as well. 4:24 But they essentially begin secreting cytokines, such as TNF alpha, interleukin- 4:29 1 and interleukin-6, 4:31 which of course leads to inflammation. 4:35 The cytokines also stimulate the fibroblast-like synovial sites. 4:41 When the fibroblast-like synovial sites are stimulated, they essentially become 4:45 activated 4:46 and then they begin to proliferate. 4:49 At the same time, they also begin assisting in the rank L expression, 4:54 stimulating the 4:54 rank L expression, which together with the cytokines here will stimulate oste 4:59 oclast 5:00 activity, which will lead to bone erosion, what we find in rheumatoid arthritis 5:07 . 5:07 When the fibroblast-like synovial sites are stimulated and proliferate, they 5:12 also begin 5:12 secreting proteases. 5:15 These proteases essentially cause the cartilage to break down, so we get cart 5:20 ilage degradation. 5:21 And the cartilage also secrete proteases, and it's sort of like a feedback loop 5:28 . 5:28 Another interesting feature of where of the fibroblast-like synovial sites is 5:32 that when 5:33 it's stimulated, when it's activated, these guys can actually migrate from 5:39 joint to joint, 5:39 so they can migrate from the hand joint on one side to the hand joint on the 5:43 other. 5:43 And this is why we get symmetrical arthritis in rheumatoid arthritis. 5:50 We also can find T cells in the area in the synovium. 5:54 T cells make up about 50% of the immune cells in this area, so they're very 5:59 important in 5:59 the pathophysiology. 6:01 T cells promote inflammation, essentially, and they secrete interleukin 17, 6:07 which will 6:08 promote macrophage activity, as well as stimulate the fibroblast-like synovial 6:14 sites. 6:14 The T cells also help in the expression of rank L, which will stimulate osteocl 6:19 ast for 6:19 bone erosion. 6:23 We also find plasma cells in the area, and plasma cells only make up a small 6:27 majority, 6:28 about 5% of the immune cells, and they essentially assist in inflammation 6:33 through cytokines, as 6:34 well as through antibodies. 6:38 Now in the fluid, in the synovial fluid, not in the synovial membrane, in the 6:43 synovial 6:44 fluid, we can find neutrophils, and neutrophils, they essentially produce prote 6:50 ases and reactive 6:51 oxygen species, which will essentially cause bone and collagen, degradation, 6:57 erosion. 6:58 So they contribute to inflammation. 7:01 In the synovial fluid, we also find the immune complexes, which is a feature of 7:06 rheumatoid 7:07 arthritis. 7:08 These immune complexes are essentially antibodies that bind to one another, and 7:12 they essentially 7:13 promote inflammation. 7:14 So those are the cells that we can find in inflamed joint in rheumatoid 7:20 arthritis. 7:21 And another feature around this area is that we see angiogenesis. 7:25 Also the cytokines that are produced by all these cells, they help increase 7:29 vascular permeability 7:30 and expression of adhesion molecules on the vasculature, allowing for these 7:36 immune cells 7:37 to migrate into the joints. 7:42 But where do all these cells come from? 7:45 Why do they migrate into these joints and cause rheumatoid arthritis? 7:49 Well as I mentioned, we don't actually know, but there are a few theories out 7:54 there. 7:54 So let's go to the pre-rheumatoid arthritis phase before a person has rheumat 7:59 oid arthritis. 8:01 And there are many possible things that could contribute to the development of 8:04 rheumatoid 8:04 arthritis. 8:05 These include genetics, epigenetic modifications, smoking, a bacteria called p 8:12 oreferomonas gingivalis, 8:14 which can lead to gingivitis, essentially these things, they can cause 8:19 modification of 8:20 otobantigens. 8:22 What do I mean by modifications of otobantigens? 8:25 It essentially, what I essentially mean is modification of your own antigens to 8:31 make it 8:32 seem foreign to the immune cells. 8:34 So these things can lead to modifications of your own antigens leading to an 8:41 immune response. 8:42 And the modifications of otobantigens include what's known as stitulonation. 8:49 So not only this, things can occur in the joints, such as you can have a synov 8:54 ial injury 8:55 or hyperplasia, or you can have infection within the joint. 9:00 And this will trigger a cytokine release and it will cause inflammation. 9:04 This inflammation that occurs in the joints can also lead to modification of ot 9:10 obantigens, 9:11 also modification of your own antigens, making it seem foreign. 9:17 And this also includes stitulonation. 9:20 So because you have modifications of your own antigens, this will be recognized 9:25 by antigen 9:25 presenting cells. 9:27 And it will essentially activate the antigen presenting cells to initiate an 9:31 immune response. 9:32 The antigen presenting cell will migrate to the lymph nodes, where here I'm 9:36 drawing the 9:37 lymph node. 9:39 Remember the lymph node here is green, and within the lymph node we have the 9:42 germinal 9:43 center where we have B cells. 9:45 Anyway, the antigen presenting cell will activate T cells here in the area, so 9:50 we can 9:50 have CD4 T cell activation. 9:55 And when the CD4, when the T cell is activated, the CD4 T cell, it can activate 10:00 the B cells 10:00 in the germinal center, and this can be through co-stimulation. 10:05 When the B cells are activated, they will begin to, you know, proliferate, they 10:09 will 10:09 begin to class switch, and they will become plasma cells. 10:14 Then plasma cells will then produce otobodies. 10:18 They will produce the antibodies against your own antigen essentially. 10:24 So then what? 10:26 Well you have now CD4 T helper cells, and then you have the antibodies and the 10:32 plasma 10:32 cells, and they will also have homing receptors and stuff like that, which will 10:37 allow them 10:37 to migrate to joint tissue. 10:39 So that is how they move into the joints in rheumatoid arthritis. 10:45 So I hope that made sense. 10:47 Now it's important to talk about the antibodies, because they are an important 10:50 feature in rheumatoid 10:51 arthritis. 10:52 We have two main antibodies found, and these are, we look at one of them at a 10:58 time. 10:59 The first one is the rheumatoid factor, which is an IgM antibody, and it's 11:04 present in 75% 11:05 of people with rheumatoid arthritis. 11:08 What these guys do is that they target FC portion of IgG antibodies, so the 11:14 constant region, 11:16 and they essentially are the ones that form the immune complex and can deposit 11:21 in the 11:22 synovial fluid. 11:25 The rheumatoid factor not only forms immune complexes with itself, but with the 11:31 IgG, as 11:32 well as complement proteins. 11:36 So it will promote inflammation. 11:40 The second antibody is the anti-cytulinated protein antibody. 11:47 Now these guys, as the name suggests, they target citulinated proteins. 11:52 These are things such as fibrin and filogrin. 11:57 Now they target citulinated proteins. 12:00 What are they? 12:01 Well citulinated proteins are essentially proteins who have arginine residues 12:07 that have 12:07 been converted to citulinate, and this sort of change makes it seem foreign to 12:14 the body, 12:15 and that is why when we have modifications of our otter antigens, such as citul 12:21 ination, 12:23 our body thinks it's foreign. 12:25 And unfortunately in our joints, we have these sort of tissues, so therefore 12:32 that's how this 12:33 antibody contributes to the pathophysiology. 12:38 But essentially these rheumatoid factor and anti-cytulinated protein antibodies 12:42 , they're 12:43 important for in helping diagnose rheumatoid arthritis. 12:47 Not everyone has rheumatoid factor, but the anti-cytulated protein antibody, it 12:51 is a 12:51 lot more specific for rheumatoid arthritis. 12:57 So I hope that all made sense. 12:59 Now it's important that we talk about the extarticular involvement within rhe 13:04 umatoid 13:05 arthritis. 13:06 So what I'm talking about is involvement of other organs around the body, and 13:09 how rheumatoid 13:10 arthritis causes problems there too. 13:13 So these extarticular involvement is a result of the cytokines produced within 13:18 the joints 13:19 and stuff, and these are mainly TNF alpha interleukin 1 and interleukin 6. 13:24 So within the blood, we have increasing inflammatory cytokines, and they 13:29 essentially contribute 13:30 to many things around the body. 13:33 For example, in the skin, they contribute to the nodule formation. 13:36 In the liver, because of the cytokines, the liver will begin producing more CRP 13:41 or ECR 13:42 proteins, which are inflammatory markers, as well as the liver will produce a 13:46 lot more 13:46 hepsidin, which will contribute to anemia in rheumatoid arthritis. 13:52 Cardiovascular involvement. 13:53 Well, these cytokines and this inflammation that's occurring will actually 13:57 promote arthroegesis, 13:58 so plaque formation. 14:00 And it can also lead to promote myocardial infection as well as stroke. 14:06 Neurological involvement include fatigue and depression, and these can be 14:10 attributed to 14:11 anemia. 14:12 But what involvement is very serious in rheumatoid arthritis, sorry, musculoske 14:19 letal involvement. 14:20 So these include osteopenia, which can lead to osteoporosis. 14:25 In the muscles, the inflammation causes can lead to insulin resistance, which 14:30 can result 14:31 in muscle weakness. 14:34 And also bone marrow involvement. 14:36 We can have thrombocytosis, which is a lot of platelet, which can contribute to 14:43 the 14:43 plaque from the thrombous formation, as well as we have anemia. 14:48 So I hope that made sense, and I hope you enjoyed this video. 14:52 So those are the extra-articular involvement of rheumatoid arthritis. 14:58 You also have lung involvement, such as plural fusion and lung infection. 15:04 But this can be attributed to the treatment used for rheumatoid arthritis, 15:08 which involves 15:09 glucocorticoids. 15:10 And as we know, glucocorticoids suppress the immune system. 15:14 I hope you enjoyed this video. 15:16 We looked at the clinical manifestations, the hand involvement, the pathophys 15:21 iology, the 15:22 causes, potential causes, as well as the articulate manifestations of rheumat 15:25 oid arthritis. 15:26 Thank you for watching. 15:27 Bye.