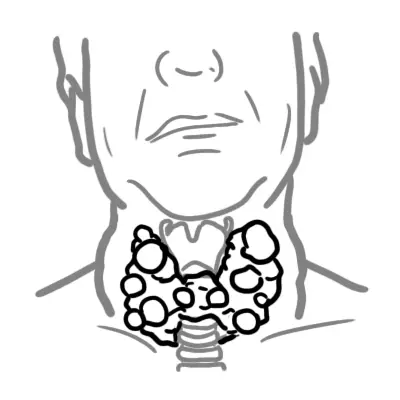
Overview Goitre refers to an enlarged thyroid gland. Thyroid nodules are common in the general population, especially in women. Goitre results from follicular cell hyperplasia at one or multiple sites within the thyroid gland. Goitre can be classified based on morphology into diffuse or nodular.
Prevalence rates range from 5 to 50%. Factors associated with increasing numbers and size of thyroid nodules include Graves disease and pregnancy. Low iodine intake is associated with an increased incidence of hyperfunctioning nodules (also called toxic adenomas). Thyroid nodules always raise the concern of cancer, although <5% are cancerous.
| Definition Goitre: Enlarged thyroid gland (Latin gutur meaning throat) Thyroid Nodule: Cause of goitre. It is a discrete lesion distinct from the surrounding thyroid parenchyma. Most nodules are benign and only 5% to 12% of the nodules detected on ultrasonography are malignant. Most thyroid nodules, including thyroid cancers, are asymptomatic. |
| Thyroid Nodule based on Morphology | |
| Diffuse | Nodular |
| Pregnancy | Multinodular goitre |
| Graves Disease | Adenoma |
| Hashimoto's Disease | Carcinoma |
| Drug induced (lithium, amiodarone) | |
| Iodine Deficiency | |
| Thyroid Nodule based on Thyroid function status | |
| Toxic | Non-toxic (simple) |
| Graves Disease | Pregnancy |
| Thyroiditis | Drug induced (lithium, amiodarone) |
| Multinodular goitre | Iodine Deficiency |
| Risk Factors raising suspicion of thyroid malignancy |
| Age (<20 or >60) |
| Rapidly enlarging nodule |
| Localised symptoms including dysphagia, stridor or hoarseness |
| Previous exposure to radiation |
| Family History |
| Familial polyposis coli |
| Lymphadenopathy |
| Hashimoto disease |
Clinical Examination Nodules may be:
| Remember Thyroid lump with normal TFT is thyroid malignancy until proven otherwise |
Malignancy
| Side note Pemberton's sign is facial erythema and jugular venous distension upon raising the arms. It is a sign of superior venacaval obstruction caused by a substernal mass. |
| AETIOLOGY OF GOITRE | |
| Diffuse | Nodular |
| Pregnancy | Multinodular goitre |
| Graves Disease | Adenoma |
| Hashimoto's Disease | Carcinoma |
| Subacute thyroiditis (de Quervain's) | |
| Drug induced (lithium, amiodarone) | |
| Endemic (iodine deficiency) | |
| Differential Diagnosis of Neck Swelling | |
| Congenital conditions | Thyroglossal tract abnormalities Brachial cyct |
| Tumours | Thyroid Salivary glands Carotid body (Chemodectoma) Sarcoma Lipoma |
| Lymph nodes | Primary Malignancy (Lymphoma, leukemia) Secondary Malignancy (oesophagus, mouth, nasopharynx) Inflammatory Conditions (tonsilitis, mononucleosis, HIV) |
| Diverticulae | Oesophagus |
The primary goal when evaluating a thyroid nodule is to determine whether it is malignant.
First line Investigations
If ↓TSH
If TSH normal or ↑TSH
| Remember Fine Needle Aspiration is for diagnosing malignancy |
| AETIOLOGY OF GOITRE | |
| Diffuse | Nodular |
| Physiological (Pregnancy) | Multinodular giotre |
| Graves Disease | Adenoma |
| Hashimoto's Disease | Carcinoma |
| Subacute thyroiditis (de Quervain's) | |
| Drug induced (lithium, amiodarone) | |
| Endemic (iodine deficiency) | |
| Remember Thyroid Carcinomas are mainly follicular or papillary (most common). Medullary cancers are rare. |
Non-toxic goitre
Toxic Goitre (overactive thyroid or nodule)
Malignant/suspicious thyroid or nodule
| Indication for thyroid surgery |
| Troubling compressive symptoms |
| Fail to respond to medical therapy |
| Suspicious thyroid nodule |
| Malignant thyroid nodule |
| Cosmetic |
Complications of thyroidectomy
