Overview
- Overweight and obesity are common worldwide and are associated with many conditions, particularly diabetes, hypertension and dyslipidemia.
- Overweight and obesity are defined as a moral or excessive fat accusation that presents a risk to health
- Obesity is now dramatically on the rise in low and middle-income countries
- Management should include diet, physical activity, and behaviour change components. Long term follow-up is needed
- Bariatric surgery is a treatment option for some patients with severe obesity, particularly those with type 2 diabetes. Such patients should be assessed for their suitability for this treatment
Aetiology and Risk Factors
Aetiology
- Multi-factorial
- Energy intake > energy expenditure over a prolonged period
- Intake – cultural expectation, food availability, financial resources, likes and dislikes, emotional (anger, boredom), lack of satiety, dieting -> food cravings
- Change in Base Metabolic Rate (BMR)
| Side note Expenditure – Base Metabolic Rate (70%), thermogenesis (20%), exercise (10%). Base metabolic rate Approximately 1800 calories a day for 70kg man.Increase BMR – Sever exercise, fever, catecholamines, caffeine, thyroid hormones, smokingDecrease BMR – Age, female 10% below male, menopause. |
- Epigenetics
- Environmental factors are responsible for the increase in average weight of the population
- Genetic factors explain 30-50% of variation in body weight between individuals
Risk Factors
- Genetic prediposition
- Inactivity
- Unhealthy diet and eating habits
- Family lifestyle
- Quitting smoking
- Pregnancy
- Lack of sleep
- Certain medications
- > 40 yo
- Social and economic issues
- Hypothyroidism
- Hypercortisolism
- Corticosteroid therapy
Clinical Manifestation
| Remember Assess any environmental, social, and family factors, including family history of overweight or obesity and comorbidities. |
Clinical Presentation
- Varies
Physical examination
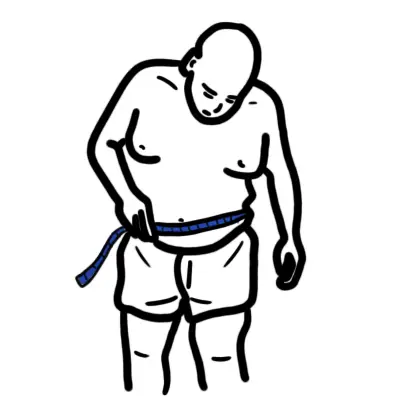
- ↑↑ BMI and Waist
- Hypertension
- Acanothosis Nigricans
- Striae
- Hepatomegaly
- Gait and mobility
- hypothyroidism?
- Cushings disease?
Assessment of weight and obesity
- Adipocity (fat tissue) is an important measurement of body weight, not total body weight.
- Body mass index (BMI) is a good, but imperfect measurement of adiposity.
- BMI = weight (in Kg)/ Height (m)2
| Think Limitations of BMI on: |
| Muscular people |
| Elderly people |
| Young children (centile charts) |
| Classification | BMI | Risk of morbidities |
|---|---|---|
| Underweight | <18.5 | Increased |
| Normal weight | 18.5–24.9 | Low |
| Overweight | >25 | Increased |
| Obese I | 30–34.5 | Moderate |
| Obese II | 35.0–39.9 | Severe |
| Obese III | >40 | Very severe |
- Waist circumference is a useful indicator of central adiposity that can also be used to indicate cardio metabolic risk
- Distribution of body fat is crucial (PEAR is better than APPLE)
| Side note An adult’s waist circumference is measured halfway between the inferior margin of the last rib and the crest of the ilium in the mid-axillary plane. The measurement is taken at the end of normal expiration. |
Diagnosis
- Primary Hypothyroidism
- Secondary Hypothyroidism
- Cushing’s Disease
- Glucocorticoid therapy
Investigations
- Glucose
- Cholesterol/lipid profile
- LFT
- Thyroid function test
- Cortisol test
| Remember Investigate comorbidities and other factors to an appropriate level, depending on the person, timing of assessment, degree of overweight or obesity, and previous assessments. |
Treatment
| Facts about obesity |
| Genetics factors play a big role, but heritability is not destiny. Life-style modification (environmental change) can promote weight loss as much as pharmaceutical agents available |
| Trying to go on a diet is effective in losing weight but generally does not work well in the long-term |
| Exercise increases health regardless of body weight or weight lost |
| Physical activity or exercise in a sufficient dose aids in long-term weight maintenance |
| Continuing doing things that promote weight loss helps maintain weight loss |
| Programs that involve overweight children and their parents help promote greater weight loss or maintenance |
| Meal replacement products help promote greater weight loss |
| Pharmaceutical medication can help with weight loss and maintenance as long as the agents continue to be used. |
| In appropriate patients, bariatric surgery results in long-term weight loss and reductions in the rate of incident diabetes and mortality |
Significant benefit (a reduction in mortality and morbidity) can be obtained with moderate weight loss (5-10%). Energy Balance is key!
Lifestyle modifications
- Diet and eating habit
- Physical activity
- Behavioural modification
Pharmacotherapy
Medications can have an adverse effect on weight by influencing either food intake (hunger) or energy expenditure. Medication should be considered in people who have a BMI >25
- Orlistat
- Sibutramine
- Phentemine (not good for long terms as risk of dependence and abuse increases)
- Antidepressants
- Antipsychotics
- Insulin
Bariatric Surgery
The most effective treatment for the morbidly obese
- Roux-en-Y Gastric bypass (30% of body weight lost)
- Gastric banding -> can induce reflex -> Barrats -> adenocarcinoma
- Sleeve Gastroectomy
| Indications for Bariatric Surgery |
| Other approaches were unsuccessful |
| BMI >35 |
| Understands surgery and risks |
| No uncontrolled psychological conditions |
| Dedicated to life-style change and follow-up |
Complications and Prognosis
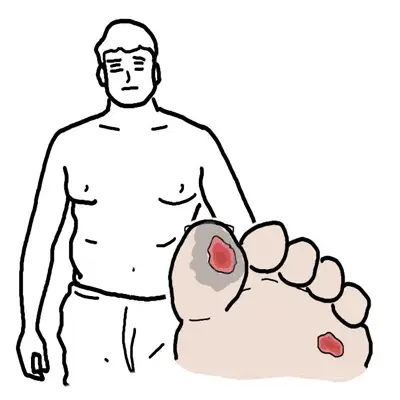
Complications
- All-causes of death (mortality)
- Metabolic Syndrome
- Hypertension
- Dyslipidemia
- Type 2 diabetes
- Coronary heart disease
- Stroke
- Gallbladder disease
- Osteoarthritis
- Sleep apnea and breathing problems
- Some cancers (endometrial, breast, colon, kidney, gallbladder, and liver)
- Low quality of life
- Mental illness such as clinical depression, anxiety, and other mental disorders
- Body pain and difficulty with physical functioning
| Metabolic Syndrome is a cluster of risk factors comprising of excess abdominal weight, lipid abnormalities, hypertension and elevated glucose levels. |