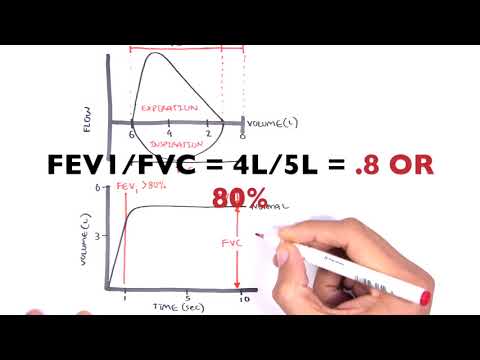
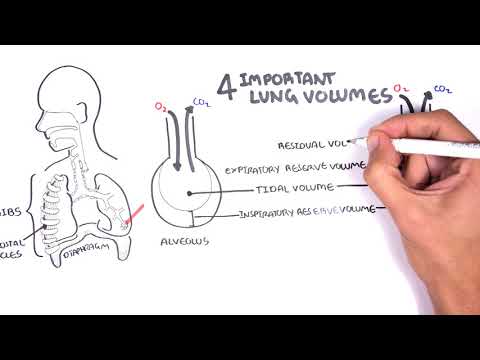
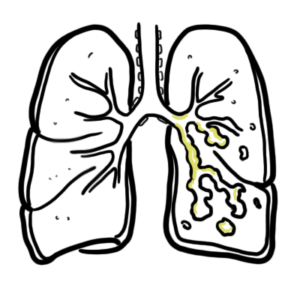
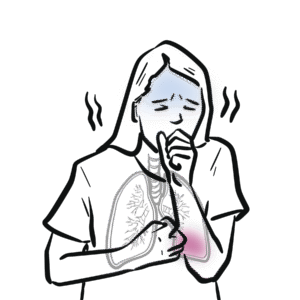
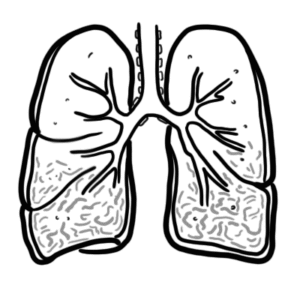
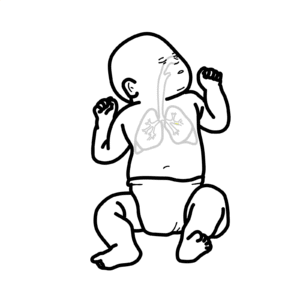
0:00 In this video we're going to look at asthma in adults. 0:08 This is an overview and introduction. 0:13 Asthma is a common lung disease affecting millions of people. 0:17 Asthma is caused by narrowing of the airways in the lungs. 0:21 Asthma can be treated successfully and is also related to other atopic 0:31 disorders. 0:33 Here I'm drawing the left and right lung. 0:36 The trachea bifurcates into the left and right lung. 0:40 The trachea gives rise to bronchi, which branch into smaller and smaller bronch 0:46 ioles until 0:47 the alveoli. 0:50 The normal bronchiol have smooth muscles, which help in narrowing and dilating 0:57 the lower 0:57 respiratory tract. 1:00 The respiratory tract is also covered with mucus, which helps in protecting the 1:07 airways. 1:08 In asthma there are three important changes. 1:12 You have smooth muscle contraction, which narrows the airways, smooth muscle 1:18 hypertrophy, 1:20 and mucus hypersecretion, all of which contribute to the narrowing of the air 1:26 ways. 1:27 These three features results in the signs and symptoms of asthma, which include 1:32 cough, 1:33 dystonia, or shortness of breath, and an expiratory wheeze. 1:39 Coastal with asthma also may present with recent respiratory tract infections. 1:45 There are some things you can also see inside the nose on the nasal concae. 1:50 You may see nasal polyploids, which can be a sign or a risk factor. 1:58 The risk factors for asthma include having a family history, a topic history, 2:05 an allergy, 2:07 having nasal polyploids, having gourd, and obesity. 2:20 Investigations for asthma. 2:21 Gold standard is measuring the peak expiratory flow rate, which is a test that 2:26 measures how 2:26 fast a person can exhale, can breathe out, and this tests lung function. 2:34 There is also the spirometry, which in asthma shows an obstructive pattern. 2:42 The spirometry will give you an FEV1 over FVC ratio, which is your forced expir 2:49 atory volume 2:50 at one second, over your forced volupacity. 2:54 This ratio is important in diagnosing obstructive diseases, including asthma. 3:01 A normal inspiration and expiration measurement will have sufficient volume and 3:06 flow on the 3:06 graph. 3:10 In asthma, there is decreased inspiratory volume, and expiration shows an 3:15 obstructive 3:16 pattern. 3:17 A FEV1 over FVC ratio of 80% of predicted or less is diagnostic for asthma. 3:27 Estration of a bronchodilator will improve lung function. 3:35 When asthma is diagnosed, proper education and management is required. 3:40 Management includes developing an asthma action plan for patients. 3:46 Medications include short-acting beta agonists, long-acting beta agonist, laba, 3:52 corticosteroids, 3:54 inhaled, starting with low dose, and then moving to higher dose if severity 4:00 increases, 4:01 and then oral corticosteroids can also be used in severe cases. 4:08 Immunomodulators can be used especially to help patients with allergies and 4:16 triggers. 4:17 Education about asthma and use of inhalers are also important. 4:23 Asthma can be mild, moderate, or severe. 4:26 Depending on the severity, different management options can be implemented. 4:31 One way is to develop a management plan for asthma, the step approach. 4:38 In general, asthma can be intermittent or persistent. 4:44 Intermittent means it comes and goes, such as exercise-induced asthma. 4:50 That means that it's always there. 4:54 The step approach covers six steps. 4:59 Step one is for intermittent asthma. 5:02 For persistent asthma is step two to six, six being the most severe. 5:10 For intermittent asthma, step one, short-acting beta agonists are used, and 5:16 this is for quick 5:17 relief. 5:18 In general, all patients with asthma should be on a short-acting beta agonist 5:24 for quick 5:25 relief. 5:27 Step two, you can add a low dose inhaled corticosteroid, and this is used as a 5:33 preventa, together 5:35 with the short-acting beta agonist, which is the reliever. 5:40 If patients cannot handle corticosteroids, other alternatives are available, 5:45 such as 5:46 the leukotrine receptor antagonist, Monteleucast. 5:52 Step three, a long-acting beta agonist can be used, together with the low dose 5:58 inhaled 5:59 corticosteroids and the short-acting beta agonist. 6:04 Step four, a long-acting beta agonist can be used, together with medium-dose 6:10 inhaled 6:11 corticosteroids and short-acting beta agonists. 6:17 Alternatives to the short-acting beta agonist, the long-acting beta agonist, or 6:23 the inhaled 6:24 corticosteroid dose are medications such as nidochromil, the leukotrine 6:31 receptor antagonist, 6:33 as I mentioned earlier, and theofoline. 6:37 These medications, again, can be used as alternatives to the Saba, Laba, and 6:44 the ICS. 6:45 For step five, a long-acting beta agonist can be used, together with a high 6:50 dose inhaled 6:51 corticosteroid and short-acting beta agonist. 6:56 Possibly, an immunomodulator can be added to this step to help with allergic 7:05 symptoms. 7:06 Step six, asthma is severe, and so in addition to all the medications in step 7:12 five, an oral 7:13 corticosteroid is also used.