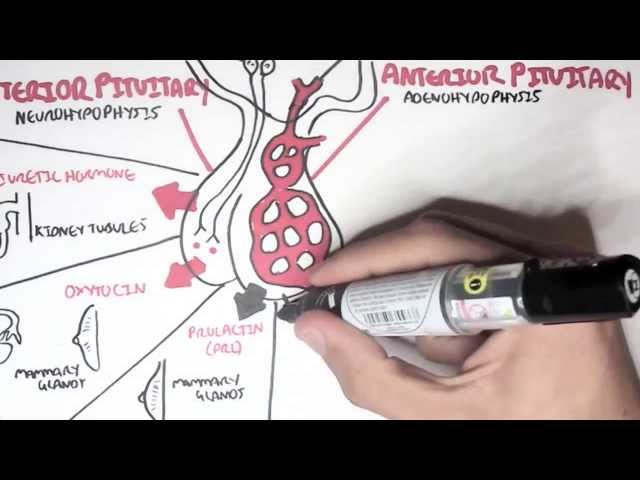
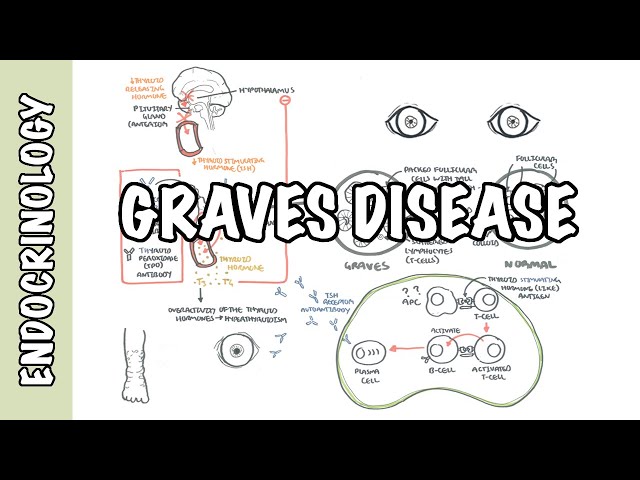
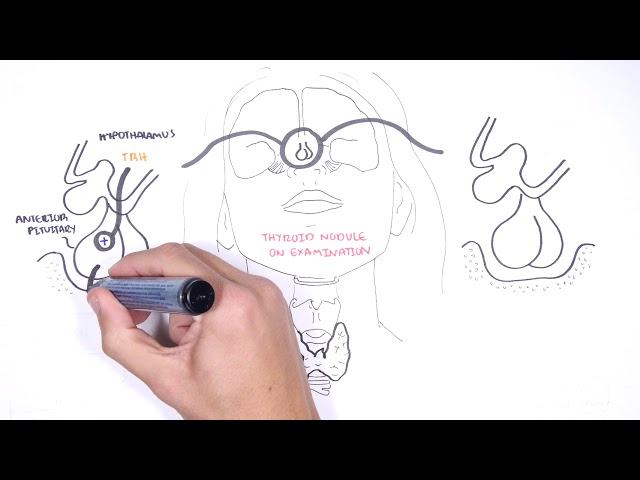
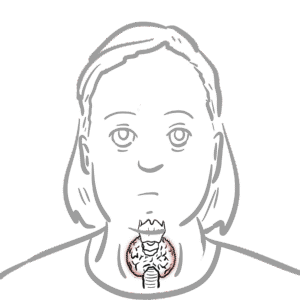
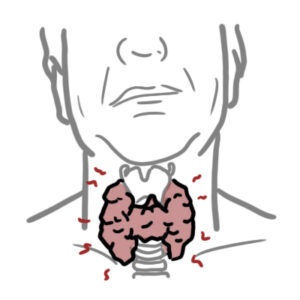
0:00 Hello, in this video we're going to talk about the hypothalamic pituitary 0:10 thyroid axis. 0:12 The hypothalamic pituitary thyroid axis plays the major role in regulating 0:17 thyroid hormone 0:18 homeostasis in the body. 0:20 The thyroid hormones are very important in fetal development and metabolism. 0:25 The thyroid structures are the hypothalamus, the pituitary gland, specifically 0:29 the anterior 0:29 pituitary gland, and the thyroid gland. 0:33 The thyroid gland is located at the base of the neck and wraps around the tr 0:36 achea just 0:37 below the crackword cartilage. 0:40 Here is a zoomed in structure of the hypothalamus and the pituitary gland. 0:46 The hypothalamic pituitary thyroid axis is under the control of neurons located 0:52 in the 0:52 median region of the PVN that synthesize and release thyrotropin releasing 0:59 hormone, TRH, 1:01 into the pituitary portal circulation. 1:04 TRH, which is a tripeptide, stimulates the release of TSH, thyroid stimulating 1:11 hormone, 1:12 from the anterior pituitary, which in turn travels towards the thyroid gland to 1:18 stimulate 1:18 the synthesis and the release of thyroid hormones. 1:22 Again, thyrotropin releasing hormone, TRH, stimulates the synthesis and 1:28 secretion of 1:28 thyroid stimulating hormone, TSH, which acts at the thyroid to stimulate all 1:35 steps of thyroid 1:36 hormone biosynthesis and secretion by binding onto thyroid stimulating hormone 1:41 receptors. 1:42 The thyroid hormones are triadothyronin, T3, and thyroxin, T4. 1:48 These thyroid hormones control this accretion of TRH and TSH by negative 1:55 feedback to maintain 1:56 the physiological levels of the main hormones of the hypothalamic pituitary 2:01 thyroid axis. 2:03 Reduction of circulating thyroid hormones, T3 and T4 levels, due to primary 2:08 thyroid failure 2:09 results in increased TRH and TSH levels. 2:15 Whereas if there is high thyroid hormones, so high T3 and T4, the opposite 2:20 occurs. 2:21 You have low TRH and low TSH. 2:33 The functional units of the thyroid glands are the follicles made up of foll 2:38 icular cells. 2:39 The center of the follicle is the colloid. 2:42 The thyroid gland has a rich blood supply, and here are the capillaries, which 2:46 will bring 2:47 TSH thyroid stimulating hormones to these cells. 2:52 Next to the follicles are the parafolicular cells, also known as C cells, which 2:57 produce 2:58 calcitonin, another hormone, which we will not talk about, but has an important 3:03 role 3:03 in calcium homeostasis. 3:07 Moving closer now at the interaction between the capillary and the follicle, 3:12 the capillaries 3:13 of course brings thyroid stimulating hormone to the area. 3:18 The inner part of the follicle is the colloid, the center. 3:23 On the follicular cells you have thyroid stimulating hormone receptors. 3:28 When thyroid stimulating hormone reaches the thyroid follicular cells, it binds 3:32 to thyroid 3:33 stimulating hormone receptors, causing a number of things. 3:37 Firstly, it will stimulate tharglobulin production, tharglobulin will enter the 3:44 colloid. 3:45 Tharglobulin contains tyrosine groups, which are important in making the 3:50 thyroid hormones. 3:52 TSH also stimulates the expression of channels, such as sodium iodide channels, 3:57 allowing circulating 3:58 iodide to enter the follicular cells. 4:02 From here iodide enters the colloid via another channel, and becomes oxidized 4:09 to iodine. 4:10 Iodine and tharglobulin is what makes our thyroid hormones, T3 and T4. 4:17 T3 and T4 will enter circulation. 4:21 The thyroid hormones travel in circulation bound to proteins, the main protein 4:26 being 4:27 thyroxine binding protein, and here it will target the different cells around 4:32 our body 4:32 to elicit an effect, so increasing metabolism. 4:36 And that concludes a brief overview of the hypothalamic pituitary thyroid axis, 4:42 as well 4:42 as some physiology of the thyroid gland.