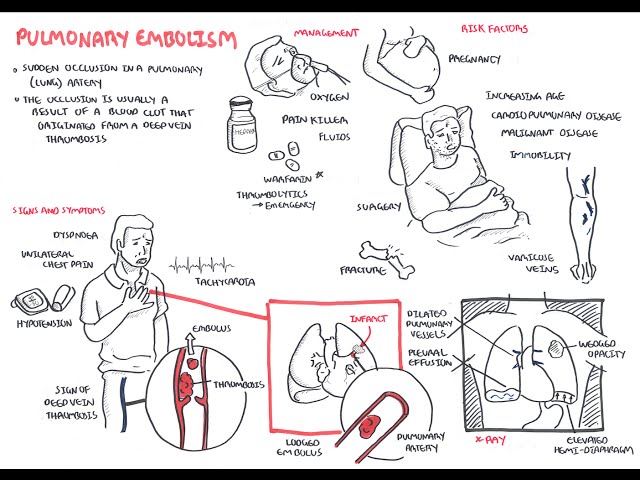
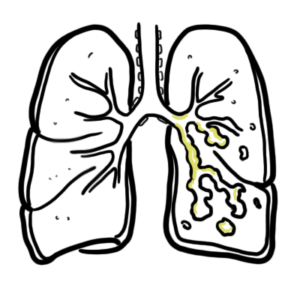
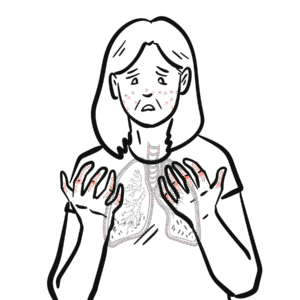
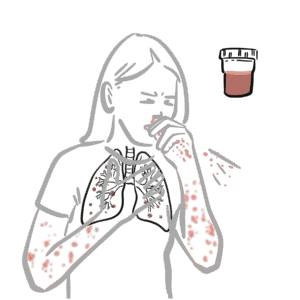
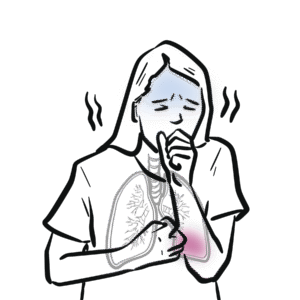
0:00 Idiopathic pulmonary fibrosis is the main idiopathic interstitial pneumonia, 0:08 which is 0:08 a diffuse parenchymal lung disease of unknown cause. 0:12 Again, idiopathic pulmonary fibrosis is a chronic progressive fibrotic inter 0:16 stitial lung 0:17 disease of unknown cause. 0:19 That primarily occurs in older adults. 0:24 Doctors suspect interstitial lung disease when an adult presents with 0:27 unexplained exertional 0:28 bistnea, chronic dry cough, or velcro-like inspiratory crackles of examination, 0:35 and 0:35 more specifically fibrosis of the lung bases. 0:40 The dyspnea is typically progressive over months to years. 0:44 A differential diagnosis is heart failure and chronic obstructive pulmonary 0:48 disease 0:48 COPD, which people are often misdiagnosed as. 0:53 Normally, our lungs allow for gas exchange, we inhale oxygen and blow out 0:58 carbon dioxide. 1:00 The functional units of the lungs are these individual alveoli, which contain 1:04 and are 1:05 surrounded by many important cells including alveolar epithelium, macrophages, 1:11 and fibroblasts. 1:13 Capillaries contain red blood cells. 1:14 Oxygen is inhaled and intercirculation by binding to hemoglobin within red 1:21 blood cells. 1:22 The exact cause of idiopathic pulmonary fibrosis is unknown, but certain risk 1:26 factors have 1:27 been identified, including genetic factors such as issues with surfactant 1:34 proteins, gel 1:36 forming mucin, and telomerase things. 1:39 Other risk factors, older age, male sex, cigarette smoking, gastroesophageal 1:45 reflux disease, 1:47 disposable micro aspirations from this can trigger formation of idiopathic 1:52 pulmonary fibrosis. 1:54 Another risk factor is obstructive sleep apnea, air pollution, and herpes 1:59 infection. 2:00 Whatever the trigger, risk, or cause of idiopathic pulmonary fibrosis is, it 2:05 develops slowly, 2:07 thought to be a result of recurrent micro-injuries. 2:11 These injuries are specifically recurrent alveolar epithelial and basement 2:16 membrane injuries, 2:17 which activate cells within the alveoli to release pro-inflammatory cytokines 2:23 and chemokines, 2:24 such as TNF-alpha, interleukin-1, and MCP-1. 2:29 These mediators will activate resident fibrocytes and recruit circulating fibro 2:36 cytes. 2:42 On top of this, pro-fibrotic chemicals such as platelet-derived growth factor 2:46 and transforming 2:47 growth factor beta are also secreted by alveolar cells, which stimulate fibrobl 2:53 asts to activate 2:54 and proliferate, differentiate into myofibroblasts and stimulate collagen 3:01 synthesis, and these 3:03 fibroblasts will undergo further differentiation, expressing unique surface 3:03 proteins. 3:12 Following the induction of fibroblasts activation, proliferation, and 3:16 differentiation by epithelial 3:18 injury, the fibroblasts and myofibroblasts will organize into fibrotic foci. 3:26 Growth factors targeting tyrosine kinase pathways are released continuously, 3:32 which 3:32 will promote fibrotic foci formation and evolution into a fibrozed lung. 3:42 Collagen Type 3 is the predominant form of collagen in the areas of early fib 3:46 rosis, 3:47 while collagen Type 1 predominates in areas of mature fibrosis. 3:51 Fibroblasts proliferation and collagen deposition is a normal repair mechanism 3:58 with acute injury to the lungs, however, repeated insults leads to a pro-fibrot 4:04 ic event, 4:05 where there is increased synthesis of connective tissue and reduced degradation 4:10 leading to fibrosis. 4:12 Fibrosis causes abnormal architecture of the lung parenchyma, resulting in loss 4:18 of capillary 4:19 surface areas and gas exchange units. Because of this, you expect to see poor 4:24 gas exchange and 4:25 transfer on a test called the DLCO. You also see hypoxemia, low oxygen levels 4:31 in the blood. 4:36 And so the investigations to order is a pulmonary function test, and this will 4:40 show a reduced 4:42 viral capacity and reduced total lung capacity. The diffusing capacity of the 4:48 lung for carbon 4:50 monoxide often shows a reduced amount, and this is the DLCO, a reduced DLCO. 4:56 However, remember 4:58 that results may be normal early in the disease. The reduced DLCO is a result 4:58 of fibrosis in 5:05 the interstitium, and so carbon monoxide does not enter circulation properly. 5:10 There is a reduced 5:11 gas exchange, a reduced DLCO. Here is a chest x-ray of someone with idiopathic 5:17 pulmonary fibrosis. 5:19 Important clinical pearl is that typically idiopathic pulmonary fibrosis has 5:24 lower lobe 5:25 predominance. A chest x-ray may be normal early in the disease, and this can 5:32 evolve to bilateral 5:33 reticular infiltrates, hazyopacities reduced in-spiritory lung volumes in 5:38 established disease. 5:40 A high-resolution CT chest is gold-standard, and there's a pathological pattern 5:49 of what's called 5:50 usual interstitial pneumonia. Now, the usual interstitial pneumonia pattern 5:57 includes bilateral 5:59 reticulation and honeycombing that is predominantly in the peripheral and in 6:06 the lower lobes 6:07 with or without traction bronchiectasis. When the combination of clinical and 6:14 imaging is not 6:15 diagnostic, rarely a lung biopsy can be considered. Biopsies from multiple lung 6:21 lobes are taken. 6:27 Again, changes seen in idiopathic pulmonary fibrosis have lower lobe predomin 6:32 ance, 6:32 and so the differential diagnosis for lower lobe predominant disease, you can 6:37 remember 6:37 what the acronym aids, A, for asbestosis, I is for idiopathic pulmonary fib 6:43 rosis, 6:44 D is for drugin juice, so any drug such as amiodarone, nitrofluidin, and methot 6:49 rexate, 6:49 and S is for scleroderma and other connective disease, except for ankylosing sp 6:57 ondylitis, 6:58 which is the only one with upper lobe predominance. 7:00 The treatment for idiopathic pulmonary fibrosis could be divided into non-ph 7:08 armacological and 7:11 pharmacological treatment. So, non-pharmacological treatment, very important, 7:16 smoking cessation, 7:17 you know, yearly influenza as a vaccination as well as the pneumococcal 7:22 vaccines, 7:24 supplemental oxygen, pulmonary rehabilitation, and consideration of a lung 7:29 transplant. 7:29 Pharmacological therapy, interestingly, since several pathways are likely to 7:35 contribute to the 7:36 pathogenesis and pathophysiology of pulmonary fibrosis, there are two main 7:42 agents that have 7:43 been approved. These are Nintendenib and perfinididone. 7:50 Normally fibroblasts and fibrocytes contain specific tyrosine kinase receptors, 7:54 which respond to growth factors, including platelet-derived growth factors, 7:59 fibroblasts growth factors, and vascular endothelial growth factors, and 8:05 stimulation of this 8:07 causes the fibroblasts to activate proliferate differentiate, which will cause 8:11 the interstitial 8:12 changes in idiopathic pulmonary fibrosis. Nintendenib is a tyrosine kinase 8:18 inhibitor, 8:20 and so it inhibits the pathways VEGF, FGF and PDGF. Perphenidone inhibits 8:27 transforming 8:29 growth factor beta, which normally stimulates collagen production. 8:33 The side effects of this include anorexia, vomiting, photosensitive rash, and 8:40 liver 8:41 derangement. Side effects of Nintendenib include diarrhea, liver function, test 8:45 abnormality, 8:47 increased risk of bleeding, and myocardial infarction has been reported. 8:51 Other medications used in idiopathic pulmonary fibrosis is antacids because of 8:57 the risk of 8:58 gastro-sophageal reflux disease and the micro aspiration in causing idiopathic 9:03 pulmonary fibrosis. 9:05 Steroids are typically not recommended. Clinical presentation of someone with 9:11 idiopathic 9:12 pulmonary fibrosis. Again, chronic exertional dysnia is universal. A dry 9:17 chronic cough 9:19 without pearlency because if they have mucoperulent coughs, this would sway you 9:25 to 9:26 diagnosed bronchiectasis, for example, and there can be clubbing, evidence of 9:31 clubbing, 9:31 acrocynosis, just a cyanosis, bilateral velcro crackles, and spiritually crack 9:38 les, 9:38 specifically, as well as fatigue and lethargy. 9:43 Complications and mortality. So, idiopathic pulmonary fibrosis is progressive 9:52 with a median 9:53 survival of three to five years after diagnosis. The progression of disease, 9:58 however, is 9:59 variable and may be associated with periods of stability with intermittent 10:02 periods of acute decline. 10:05 Up to 20% have acute exacerbations characterized by worsening hypoxic 10:09 respiratory failure. 10:11 Exasabations are often idiopathic but can be triggered by events such as 10:15 infection, 10:15 aspiration, or some drug toxicity. Now, interestingly, there's an increased 10:21 risk of 10:22 venothermbal embolism, lung cancer, and pulmonary hypertension. 10:25 Thank you for watching. I hope you enjoyed this video on idiopathic pulmonary 10:30 fibrosis, 10:31 a chronic and progressive lung disease characterized by inspiratory velcro like 10:38 crackles clubbing. 10:39 With a median survival of up to five years, it has lower lobe predominance and 10:46 is typically 10:47 diagnosed, gold standard, with a high-resolution CT chest, which shows 10:52 particular changes, 10:53 honeycombing, as well as traction bronchiectasis. Thank you for watching. I 10:58 hope you enjoyed this video. 11:01 You