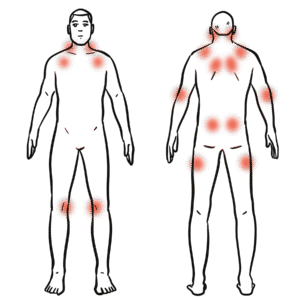
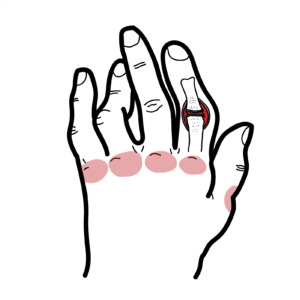
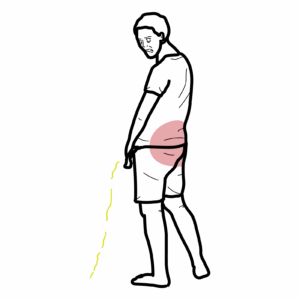
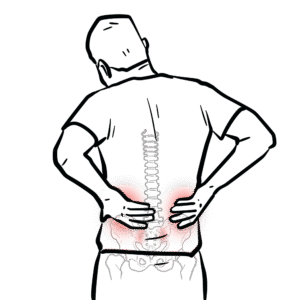
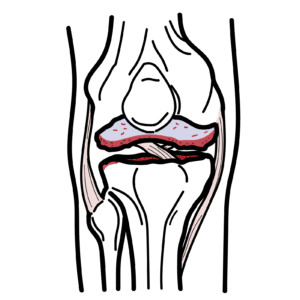
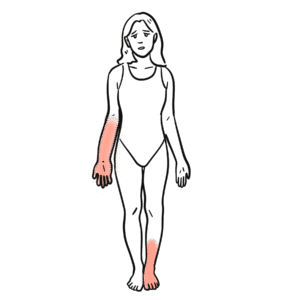
0:00 The sacraliac joints are synovial joints formed by the irregularly shaped j 0:18 agged 0:18 articulate surfaces of the sacrum and the isleum of the pelvis. 0:23 The sacraliac joint are surrounded by a fibrous joint capsule, which is 0:27 relatively thin and 0:28 weak, providing limited mobility. 0:32 The fibrous capsule is lined by a synovial membrane. 0:36 The sacraliac joint is stabilized by strong ligaments, particularly the interos 0:42 ceus sacral 0:43 ileic ligament, the key stabilizer that limits movement. 0:48 The sacraliac joint allows only minimal motion, mainly small degrees of gliding 0:53 and rotation, 0:54 including mutation and counter-utation as shown. 1:03 In this video, we're going to focus on sacral ileitis and its mimicas. 1:10 Sacralitis is defined as inflammation of one or both sacraliac joints. 1:15 It is an important cause of sacraliac joint or buttock pain, often with 1:21 inflammatory 1:22 back pain features such as insidious onset, night pain, morning stiffness, 1:26 improves with 1:27 exercise, not with rest. 1:30 Common causes of sacralitis include axial spondyloarthritis, including ankyl 1:36 osing spondylitis. 1:39 There is also psoriatic arthritis that can cause it, inflammatory bowel disease 1:45 -related 1:46 spondyloarthritis and reactive arthritis. 1:49 They all can cause sacraliitis. 1:55 Now, diagnosis of sacraliitis typically relies on imaging. 2:01 Characteristically, sacraliitis is identified by radiographic changes that are 2:05 graded from 2:06 0 to 4 using the New York criteria, although these changes tend to be late 2:12 findings. 2:13 So let's look at the New York sacraliitis grading criteria. 2:19 So grade 0, as you can see, the sacraliac joints appear completely normal. 2:24 Grade 1, there is some suspicion, there is minimal blurring sclerosis but not 2:29 definitive. 2:31 Grade 2, there is minimal abnormality. 2:35 There are small localized sclerosis, erosions, really, and mild joint space 2:47 change. 2:48 In 3, there is unequivocal abnormality, there is marked sclerosis, there is er 2:53 osions with 2:54 definite joint space narrowing or widening. 2:57 Partial ankylosis may be present. 3:00 Now grade 4 is complete ankylosis of the sacraliac joint. 3:10 The radiographic criterion, which is mandatory for diagnosing ankylosing spond 3:15 ylitis, which 3:15 is axial spondyloarthritis, is having bilateral, so both sides, grade 2 or more 3:24 , or unilateral 3:26 grade 3 sacraliitis, at least on a pelvic x-ray. 3:33 So this x-ray, if you can trust me, the sacraliac joints look abnormal, 3:37 suggesting bilateral 3:39 grade 3. 3:41 MRI with stir or fat-suppressed T2 sequences is preferred for detecting early 3:50 features 3:51 of sacraliitis, such as here you can see bone marrow edema and early erosions. 3:57 You can see whitening along the sacraliac and sacral side of the sacraliac 4:01 joint, and 4:02 this is the bone marrow edema I'm talking about, suggesting inflammation. 4:06 CT is sensitive for identifying structural damage, but does not demonstrate 4:10 active inflammation. 4:12 A bone scan cannot distinguish between mechanical or inflammatory sacraliac 4:16 joint pathology, 4:17 and is not ideal for structural assessment, such as looking at erosions or 4:27 sclerosis. 4:29 Now some important clinical insights with sacraliitis on imaging. 4:34 A normal radiograph, normal x-ray, does not exclude early sacraliitis. 4:40 Remember, x-rays show late changes. 4:42 It takes years to see damage to the sacraliac joint from sacraliitis. 4:46 So you always have to consider referral to a specialist or MRI if suspicion is 4:53 high. 4:54 Bilateral symmetrical involvement is typical in ankylosing spondylitis. 4:59 A symmetrical involvement of the sacraliac joint may point to psoriatic 5:03 arthritis or reactive 5:04 arthritis. 5:07 Non radiographic sacraliitis refers to inflammation or damage of the sacraliac 5:13 joints that is not 5:14 visible on standard x-rays, but may be detected on MRI. 5:19 So this detection on MRI, but not on x-ray, is the hallmark of non radiographic 5:26 axial 5:27 spondyloarthritis. 5:29 Importantly, the presence of sacraliitis on imaging, x-ray or MRI, does not 5:36 always indicate 5:37 an underlying inflammatory arthritis, like an autoimmune arthritis. 5:47 There are differential diagnosis of sacraliitis on imaging. 5:53 So keep in mind, sacraliitis on imaging does not always signify an underlying 5:57 autoimmune 5:58 arthritis. 6:00 Clinical context is essential, and here are some important differentials to 6:04 consider. 6:05 There is this thing called secondary hyperparathyroidism, typically a 6:09 consequence of chronic kidney 6:10 disease, and it can produce sacraliac joint changes that mimic sacraliitis. 6:16 On imaging, it is characterized by erosions, particularly on the ventral iliac 6:22 side, and 6:22 a strikingly widened joint space, as you can see clearly on panel B, which 6:28 contrasts 6:29 with joint space narrowing or fusion, usually seen in chronic inflammatory 6:38 arthritis. 6:40 Mechanical stress is another common cause of sacraliac joint changes that can 6:45 be misinterpreted 6:46 as sacraliitis. 6:48 The primary function of the sacraliac joint is to transmit loads between the ax 6:52 ial skeleton 6:53 and the lower limbs. 6:55 As a result, a considerable strain is put on the sacraliac joint, which may 7:00 lead to early 7:01 mechanical and degenerative changes. 7:04 While these changes are often asymptomatic, some may be associated with pain. 7:10 The key diagnostic clue lies in the location of subcondral bone marrow changes. 7:19 Here are cross sections of the sacraliac joint looking at it from a transverse 7:24 plane 7:25 on the left and a sagittal plane on the right. 7:29 Mechanical stress changes are usually found in the anterior part of the mid- 7:34 third of the 7:35 sacraliac joint. 7:37 The region subjected to the greatest mechanical load. 7:41 Here I color it in blue, the area of mechanical stress. 7:45 In contrast, bone marrow edema or sclerosis in the proximal or distal third or 7:51 the posterior 7:52 part of the joint raises stronger suspicion of inflammatory sacraliitis. 8:06 Low insufficiency fractures occur when normal mechanical forces act on weakened 8:11 bones, most 8:12 often due to osteoporosis. 8:14 These fractures are common in elderly women, presenting with low back pain 8:17 without significant 8:19 trauma. 8:20 Imaging typically reveals bilateral ventricle fractures through the sacral LA 8:28 that parallel 8:29 the sacraliac joints. 8:31 A transverse fracture, a component often completes a H-shaped pattern, known as 8:37 the Honda sign 8:38 or H-pattern. 8:45 Osteitis condensense iliae is usually identified and is another very good 8:50 differential for 8:51 sacraliitis. 8:53 It's usually identified incidentally during imaging for unrelated low back pain 8:57 or pelvic 8:58 pain. 8:59 This condition is sometimes mistaken for sacraliitis, and the hallmark, radi 9:04 ographic or x-ray finding 9:05 is dense, well defined, triangular shaped sclerosis on the ileic side of the 9:11 joint, often bilateral 9:13 without erosions or joint fusion. 9:15 While the sclerosis predominate in the anterior mid third, it is more extensive 9:20 than the changes 9:22 seen with mechanical stress. 9:24 Bone maradema may be seen in early stages, or intermittently in later stages. 9:31 In postpartum women, bone maradema is a well documented finding of MRI. 9:36 Prolonged mechanical stress during pregnancy can cause bone maradema in up to 9:42 60 or 65% 9:43 of women in the early postpartum period. 9:47 This tends to resolve over time, with the prevalence decreasing to about 15% at 9:53 6 months, 9:54 and then 12% at 12 months, and as low as 5% after 16 months. 9:59 However, subcondrel sclerosis can persist well beyond delivery, and therefore, 10:05 it's 10:05 very difficult often to interpret MRI findings with bone maradema in pregnant 10:11 women and even 10:12 postpartum. 10:15 Finally, sacroiliac joint infection can closely mimic autoimmune inflammatory 10:23 sacroiliitis, 10:25 but typically presents as a severe, unilateral process, often accompanied by 10:31 systemic signs 10:32 of infection. 10:35 Diagnosis is usually confirmed by image-guided aspiration and positive 10:39 microbial culture 10:40 on joint fluid. 10:46 So, in summary, we really looked at sacroiliitis, the definition of 10:50 inflammatory sacroiliitis 10:53 based on radiographic findings, and we use a New York criteria, but then we 10:59 also look 11:00 at other things such as non-radiographic actual spondyloarthritis, where there 11:06 is no x-ray 11:07 changes, but there are early MRI changes, and then we also looked at some mimic 11:07 urs of 11:11 sacroiliitis, which is important to be aware of. 11:15 Thank you.