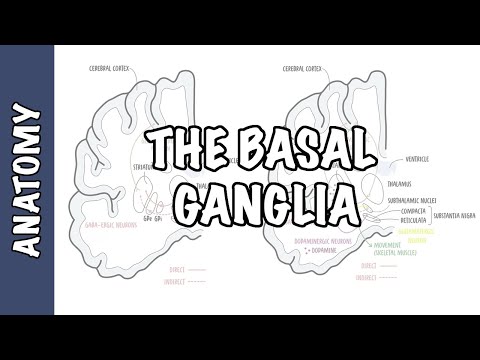
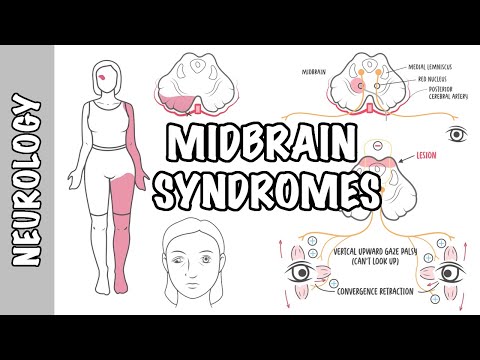
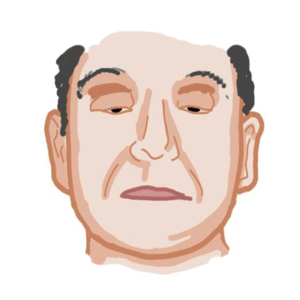
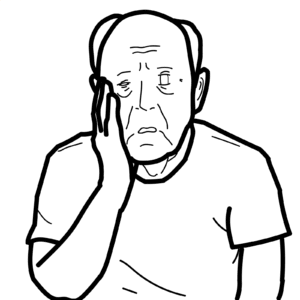
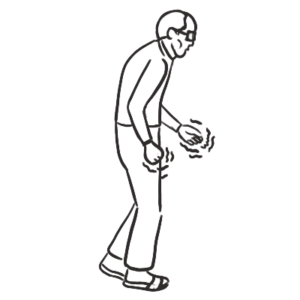
0:00 Hello, in this video, we're going to talk about Parkinson's disease, which is a 0:09 neurodegenerative 0:10 disease. 0:11 About 0.3% of the population over the age of 40 has this disease. 0:18 It's about 7.5 million people worldwide. 0:22 So let's look at the firstly signs and symptoms of Parkinson's, and here I'm 0:27 drawing a patient 0:28 who shows, who presents with tremors, shaking. 0:34 And he presents like this due to a condition called Parkinson's disease that 0:38 affects the 0:38 brain. 0:39 The cardinal features of Parkinson's disease, therefore, these include tremors, 0:45 rigidity, 0:45 bradykinesia, postural instability. 0:49 There are other features which affect the craniofacial areas, which include hyp 0:54 omimia, 0:54 which is basically a decrease in facial expression. 0:57 Thisphasia, hypophonia, reduction in basically the tone of the voice, volume. 1:06 Other features include visual problems, such as blurred vision and eyelid 1:11 opening apraxia. 1:13 Other features also include gait. 1:14 You can have shuffling, fascinations and freezing. 1:18 So all these signs and symptoms are a result of problems that occur within the 1:24 brain, particularly 1:25 in an area of the brain known as the basal ganglia. 1:28 So let's just quickly revise some important anatomical structures of the brain. 1:34 So here we have the phonics, which is an important part of the limbic system. 1:37 We have the hippocampus, which is for memory, the amygdala, for emotions. 1:41 But we will mainly concentrate on this yellow structure here, which is known as 1:46 the basal 1:47 ganglia or the basal nucleus. 1:49 Medially to the basal ganglia is the thalamus, which essentially is a 1:53 connection between the 1:54 cortex and the brainstem spinal cord. 2:01 So again Parkinson's disease is a result of problems that occur within the 2:05 basal ganglia 2:06 or the basal nucleus, because this area is responsible for muscle tone, as well 2:13 as the 2:13 ease of movement. 2:17 It helps in a smooth movement and learned movement patterns. 2:22 So let's just take a cross section, a coronal section of the brain here, and 2:26 look at the 2:26 basal ganglia in a bit more details and its components. 2:30 So here we are looking at a section of the brain. 2:33 Here in green is the thalamus, just to orientate where we are. 2:36 All these structures in yellow here, they are part of the basal ganglia. 2:45 So basal ganglia is made up of the cori nucleus, cori putamen, putamen. 2:50 The globus palitis, of which we have an external and internal part. 2:58 We also is made up of the nucleus accumbens, which I have not drawn here. 3:03 And we also have the subthalamic, subthalamic nucleus and the substantia nigra, 3:08 which consists 3:09 of two parts. 3:10 And just to complete this image, we have the amygdala here as well as the 3:16 hippocampus. 3:17 So we will mainly focus again on the basal ganglia, which is disrupted in 3:22 Parkinson's 3:22 disease. 3:23 So what does the basal ganglia do? 3:26 So let's just have a quick general overview of what it does. 3:34 So here again we have the brain and this yellow structure is a basal ganglia. 3:39 Essentially what happens is the cortex, when it wants to initiate a movement, 3:46 it will 3:47 send signals first to the basal ganglia. 3:50 And the basal ganglia will send signals back to the cortex, particularly the 3:56 motor cortex. 3:56 And then when the signals are sent back to the motor cortex, the motor cortex 4:01 can then 4:02 initiate these signals, send the signals down the spinal cord and then out 4:08 through the ventral 4:09 horn of the spinal cord to that skeletal muscle to initiate a smooth controlled 4:16 movement. 4:17 Okay, now let's look at that in a bit more detail. 4:21 So again, the cerebral cortex wants to initiate a voluntary movement, it will 4:27 first send signals 4:29 to the basal ganglia. 4:31 And the basal ganglia will help in the subconscious control of the skeletal 4:35 muscle tone, as well 4:36 as the coordination of learned movement patterns. 4:41 This information will then be sent back to the cerebral cortex through a loop. 4:46 It will be sent to the thalamus first and then thalamus will send this info to 4:49 the 4:50 cerebral cortex. 4:52 The cerebral cortex will then send the movement signals, the smooth controlled 4:57 movement signals 4:58 down the spinal cord to the skeletal muscle and thus we have a normal movement 5:05 pattern. 5:07 Two important parts in this diagram, the input from the cerebral cortex to the 5:11 basal ganglia 5:12 and the output from the basal ganglia to the thalamus back to the cortex. 5:18 In Parkinson's disease, the output number two, there's a problem in the output 5:23 and thus 5:23 we do not have a normal controlled movement pattern, it is not smooth. 5:29 So now let us go back to the big diagram and learn about the interconnection 5:34 that occur 5:35 within the basal ganglia and how and the disruption that occurs and how this 5:39 results in Parkinson's 5:40 disease. 5:42 So in this diagram, we're going to look at all the components of the basal gang 5:47 lia. 5:48 So to start, the cortenucleus and cordic putamen is also known as the cordic 5:53 striatum. 5:54 So here, the rectangular structure I'm drawing is the cordic striatum. 5:59 This is the cortex and all these other structures here are part of the basal 6:03 ganglia. 6:04 We have the substantia nigrapods compactor, the globus palitis interna, the 6:08 substantia 6:09 nigrapods reticular, the globus palitis externa, the subthalamic nucleus and 6:15 the thalamus. 6:16 Now, I'm going to start drawing the interconnections that occur within this 6:22 region. 6:23 But firstly, I want you to learn three main points. 6:29 The input from the cortex to the basal ganglia is to the striatum, to the cord 6:35 ic striatum 6:36 first. 6:37 So the input is to the cordic striatum. 6:39 The output from the basal ganglia occurs in the globus palitis interna, that's 6:43 the point 6:44 two. 6:45 So the globus palitis interna is the output from the basal ganglia to the thal 6:50 amus. 6:51 And then the thalamus will then send this information to the cortex, back to 6:54 the cortex 6:55 in that loop. 6:57 And this is point three. 6:58 The cortex will then send this information to the skeletal muscle down the 7:03 spinal cord 7:03 to cause a smooth movement pattern, coordinated movement pattern. 7:11 So those are the three main points. 7:12 The input to the basal ganglia, the output from the basal ganglia, and then the 7:17 output 7:17 from the cortex again to the muscle. 7:22 Now within the basal ganglia, there's a lot of interconnections happening 7:26 between the 7:26 glutaminergic neurons, which are the excitatory neurons, as well as the GABA-n 7:31 ergic neurons, 7:32 which are your inhibitory neurons. 7:36 But the most important thing in this diagram is within the Substantia nigra 7:42 postcompacta, 7:43 because here we have dopaminergic neurons that arise. 7:49 And these dopaminergic neurons, they release dopamine in two, the cordate stri 7:56 atum. 7:57 So dopamine can bind onto two types of receptor, D1, dopamine 1, or dopamine 2. 8:02 And depending on which receptor binds to it is either excitatory or inhibitory. 8:07 So if dopamine binds onto D1 receptor, it is excitatory. 8:12 So it will stimulate that neuron. 8:14 If dopamine binds onto D2 receptors, dopamine will inhibit that neuron. 8:23 So if we were to follow it step by step, the dopaminergic neurons release is 8:30 dopamine. 8:31 It binds onto the D1 receptor, which is excitatory. 8:35 So it will stimulate the GABA-nergic neuron here. 8:39 And it will directly inhibit this GABA-nergic neuron, allowing the thalamus to 8:47 send signals 8:49 to the cortex. 8:50 So thus the cortex can send signals to a skeletal muscle for a controlled 8:58 movement pattern. 9:00 So that is what occurs normally, but unfortunately in Parkinson's disease, 9:04 there's not much dopamine. 9:06 The dopaminergic neurons die. 9:09 So in Parkinson's disease, you have a reduced dopamine in the substantia nigra. 9:19 And the pathogenesis probably involves apoptosis or necrosis of dopaminergic 9:25 neurons. 9:26 But it is a result of the death of these neurons can be due to protein misfold 9:33 ing, aggregation 9:34 and toxicity. 9:36 It can be due to defective proteolysis. 9:38 It can be due to mitochondrial dysfunction or oxidative stress. 9:44 These are all theories. 9:46 Regardless of the cause, the result is that we have reduced dopamine in this 9:52 area, in 9:52 the basal ganglia. 9:54 Okay, now let's go back to the diagram and look at what happens if we have 10:00 reduced dopamine. 10:01 If we have reduced dopamine, dopamine does not bind on to the D2 receptor, 10:05 which normally 10:06 inhibits this GABA-nergic neuron. 10:10 Thus the GABA-nergic neuron here is now overactive and secretes GABA, which 10:15 inhibits the second 10:17 GABA-nergic neuron. 10:19 Because this GABA-nergic neuron is now inhibited, it cannot inhibit the glut 10:23 aminergic neuron in 10:24 the subthalamic nucleus. 10:26 And so the subthalamic nucleus glutaminergic neuron will secrete glutamate, 10:32 which will 10:33 stimulate this GABA-nergic neuron in the globus palitis interna. 10:39 Similarly, because we have no dopamine, the dopamine does not bind on to the D1 10:46 receptor. 10:47 And so the GABA-nergic neuron that normally inhibits the globus palitis interna 10:55 neuron 10:56 is not stimulated. 10:58 And as a result, we have an overactive GABA-nergic neuron from the globus pal 11:05 itis interna to the 11:06 thalamus. 11:09 So we have excessive inhibitory input to the thalamus. 11:14 Thus inhibition causes suppression of the thalamo corticose spinal pathway. 11:22 And because of this, the signals that the basal ganglia should have sent back 11:27 to the 11:27 cortex doesn't really happen. 11:31 And so as a result, when you want to initiate a movement, it's not smooth, 11:36 coordinated, controlled. 11:38 And thus it results in the clinical manifestations of Parkinson's disease. 11:46 I hope that all made sense. 11:48 Now let's look at the pathology of Parkinson's disease. 11:52 So let's zoom into the substantia nigra area here, which can be, which is 11:56 basically located 11:57 on the midbrain. 11:58 Here's a cross-section of the midbrain. 12:00 And let's compare Parkinson's disease, substantia nigra, to the one of a normal 12:06 patient. 12:07 What we see in Parkinson's disease is we see demyelination, neuronal loss, and 12:13 gliosis 12:14 within the substantia nigra. 12:17 Another pathological hallmark is the presence of Lewy bodies within the soma of 12:22 the neuron. 12:23 So here we have the soma of the neuron. 12:25 And this blue structure here are Lewy bodies. 12:28 And Lewy bodies are around Esonophilic intraceidoplasmic occlusions in the 12:34 nucleus, in the nucleus 12:34 of the neuron. 12:37 The Lewy bodies are made up of mainly alpha, cyanuclein proteins, ubiquinin, as 12:42 well as 12:43 those other proteins, but mainly alpha, cyanuclein. 12:48 Now let's talk about the risk factors as well as the protective factors of 12:52 Parkinson's disease. 12:54 So the risk factors of Parkinson's disease include family risk factors. 13:00 There are genetic risk factors which include GBA, CNCA, LIRK2, PARC2, and PINK1 13:07 , as well 13:09 as those shown that pesticides can cause Parkinson's disease. 13:13 Protective factors include smoking, coffee, vigorous exercising, as well as the 13:19 use of 13:19 nonsteroidal anti-inflammatory drugs. 13:24 So that concludes this video on Parkinson's disease. 13:27 We looked at the signs and symptoms. 13:29 We looked at some neuroanatomy of the basal ganglia. 13:32 We looked at the function of the basal ganglia, as well as what occurs in 13:38 Parkinson's disease. 13:39 And then we looked at the pathophys as well as the pathology and the risk 13:43 factors and 13:44 protective factors. 13:45 Thank you for watching. 13:46 I hope you enjoy this video.