Hodgkins Lymphoma
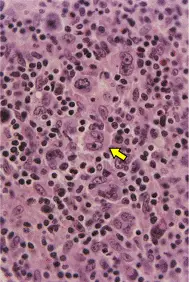
Hodgkin lymphoma (HL) arises from germinal center or post-germinal center B cells. HL has a unique cellular composition, containing a minority of neoplastic cells (Reed-Sternberg cells and their variants) in an inflammatory background.
| Remember Reed-Sternberg cell is a characteristic feature of HL. |
Classical HL – (90-95% of cases). The tumor cells in this group are derived from germinal center B cells, but typically fail to express many of the genes and gene products that define normal germinal center B cells. Classical HL is further divided into the following subtypes:
Nodular lymphocyte predominant HL – The tumor cells in this subtype retain the immunophenotypic features of germinal center B cells.
Classic Hodgkins Lymphoma is characterised by the presence of diagnostic Reed-Sternberg cells in an inflammatory back ground.
Ann Arbor staging system
Classical HL is characterised by the the presence of Reed-Sternberg cells in an inflammatory background containing other immune and non-immune cells.
Reed Sternberg cells are large cells with abundant, slightly basophilic cytoplasm, bilobed, double, or multiple nuclei, and two or more prominent, eosinophilic, inclusion-like nucleoli.
| Watch video Immunology – B cell maturation |
Most patients with HL
Chemotherapy (ABVD – doxorubicin, bleomycin, vinblastine, dacarbazine) +/- Radiotherapy
Refractory and relapsing
Chemotherapy +/- radiotherapy + autologous stem cell transplantation is preferred.
Prognosis
Patients with early stage (stage I-II) HL have a high likelihood of achieving long-term complete remission. A variety of prognostic factors allow for the discrimination of patients with “favourable prognosis” early stage HL and those with “unfavorable prognosis” early stage HL.
Among patients with advanced stage (stage III/IV) HL, prognosis is largely determined by the International Prognostic Score

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion