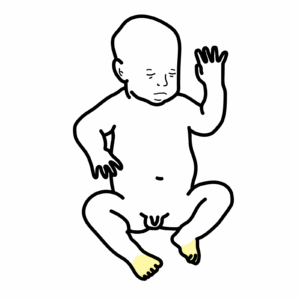
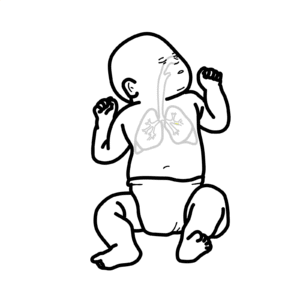
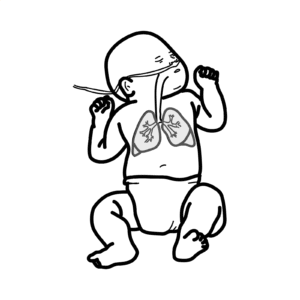
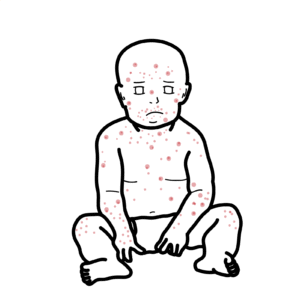
0:00 Hello, in this video, we're going to look at cute gastroenteritis. 0:10 This is an overview and introduction. 0:13 Let's begin by looking at a scenario. 0:18 So a mother brings in her child who has been recently sick. 0:24 The child's been vomiting for the past 24 hours. 0:29 She's also been having some diarrhea and also having a fever. 0:32 Upon examination, you see that the child has sunken eyes, dry mucosa, reduced 0:38 skin 0:38 turgor and has tachycardia. 0:43 And so your provisional diagnosis, best based on these findings, is acute 0:48 gastroenteritis. 0:50 Gastroenteritis is defined as having three or more loose or watery stools in a 0:54 24-hour 0:54 period with or without vomiting and typically with a fever. 1:00 Gastroenteritis lasts around one week but not longer than two weeks. 1:06 Gastroenteritis is a common pediatric condition and the main thing to remember 1:12 about gastroenteritis 1:14 is that we want to avoid dehydration and to avoid dehydration you have to give 1:20 fluids. 1:21 Interrel feeding is preferred but of course if the child has more moderate or 1:27 severe signs 1:28 of dehydration, a nasogastric tube or IV fluids are used. 1:35 So for gastroenteritis, avoiding dehydration is critical and so it is important 1:41 to look 1:41 for signs of dehydration. 1:45 A child can have no clinical signs of dehydration. 1:49 Maybe the child has some increased thirst and maybe decreasing your own output. 1:54 A child with mild dehydration will have dry mucosa membranes, feeling thirsty, 2:01 have mild 2:02 tachycardia and decreased your own output. 2:07 And then you have moderate dehydration. 2:10 In moderate dehydration you have dry mucosal membranes, sunken eyes, some 2:16 respiratory signs, 2:17 cachycardia, reduced skin turgor and lethargy. 2:22 A child who is severely dehydrated can be said is in a sign of shock. 2:27 They'll have all the signs above mentioned, mottled cool limbs, altered 2:32 consciousness 2:32 and signs of shock. 2:36 The main complications in gastroenteritis is to do with underhydration or 2:41 dehydration 2:42 and overhydration. 2:45 The most severe case would be shock. 2:51 For overhydration, the more severe cases would be cerebral edema and even death 2:59 . 2:59 Now let us look at an algorithm of acute gastroenteritis. 3:03 So again just recapping. 3:06 We have a child who has fever, has been vomiting, non-bilis and with abdominal 3:11 pain and with 3:12 some diarrhea. 3:14 This is the triad for acute gastroenteritis. 3:18 The etiology, the cause of gastroenteritis is mainly viral in more than 70% of 3:23 cases. 3:24 It's usually rotavirus, norovirus or adenovirus. 3:28 There are also some bacterial causes which make up less than 20% such as campyl 3:32 obacter, 3:33 E. coli, shigella and salmonella. 3:37 There are also protozoan, protozoan and helmets that can cause acute gastro 3:41 enteritis 3:42 but these are less common. 3:46 While examining a child with suspected acute gastroenteritis, it's also 3:51 important to look 3:52 for red flags. 3:54 Red flags indicate a more severe cause. 3:58 Red flags include severe abdominal pain, persistent diarrhea for more than 10 4:04 days, blood in 4:04 the stools, vomiting without diarrhea and just being very unwell, having a very 4:12 unwell 4:12 appearance. 4:14 So a child comes into the hospital. 4:17 What would you first do? 4:18 Well, you would take a history and examination and based on this, your 4:23 provisional diagnosis 4:24 is gastroenteritis. 4:26 You then go on to assess degree of dehydration but it's important that you have 4:32 differentials 4:33 in mind and some good differentials for acute gastroenteritis include causes of 4:39 increased 4:39 intracranial pressure, diabetic ketoacidosis, sepsis, urinary tract infections, 4:47 appendicitis 4:49 and other surgical causes of acute abdomen. 4:56 So your provisional diagnosis is gastroenteritis and you want to assess the 5:01 degree of dehydration. 5:02 It can either be mild dehydration, moderate dehydration or they can have severe 5:08 dehydration. 5:09 During this time, investigations can also be performed but investigations are 5:14 not required 5:15 usually only in cases of moderate to more severe dehydration. 5:21 Some investigations include full blood count, EUC, glucose, stool sample and 5:29 culture, urine 5:30 analysis and you can also consider blood cultures for children or babies that 5:36 have a high fever 5:38 and have severe signs of dehydration. 5:43 Now let's look at each of these categories of dehydration and see what the 5:48 common procedure 5:48 is. 5:50 So for mild dehydration, remember fluids is important. 5:54 So if the child is tolerating oral fluids, you can monitor them and then just 6:00 discharge 6:01 them. 6:02 However, if they are not tolerating oral fluids, you want to encourage oral 6:07 fluid intake and 6:08 admit if they are worsening. 6:12 For moderate dehydration, it's the same principle. 6:15 You want to encourage oral rehydration but if this is not possible, there are 6:19 other options 6:21 including nasogastric rehydration and IV rehydration. 6:26 Again, if they are not tolerating oral fluids and they are not improving, it's 6:31 important 6:32 to admit and monitor them. 6:35 So for the scenarios where oral fluid intake is not possible, it's important to 6:41 admit and 6:41 monitor the child, to check for vitals regularly and once they are improving, 6:47 you can discharge 6:49 and then follow up later on. 6:52 For severe dehydration, this is admitting the child straight away. 6:56 The child is in a state of shock and it's important to reassess them frequently 7:02 . 7:03 Airway, breathing and circulation are very important in children who have 7:10 severe dehydration. 7:12 Circulation includes getting an IV access, taking bloods for investigation and 7:17 rehydration 7:18 with IV fluids. 7:19 And of course, this child will be admitted, monitored and once improved, once 7:25 improving, 7:25 you want to encourage oral intake, oral fluid intake and then discharge and 7:30 follow up.