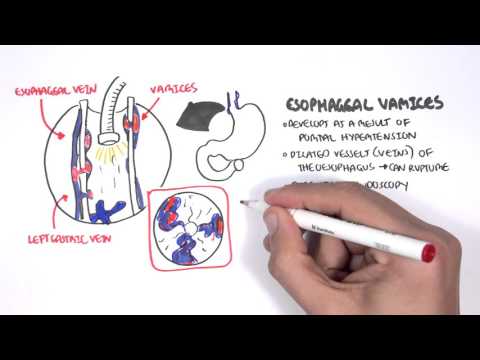
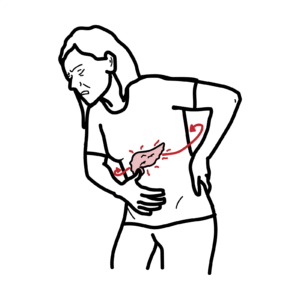
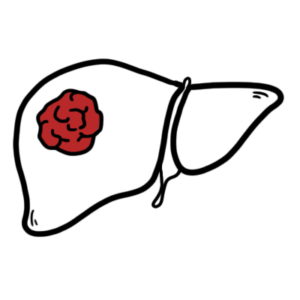
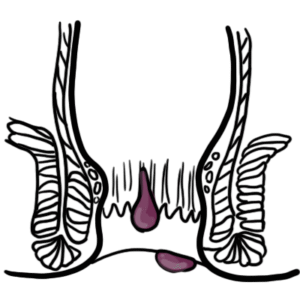
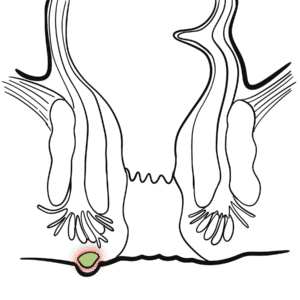
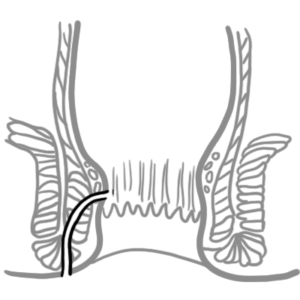
0:00 In this video we're going to look at acute pancreatitis. 0:08 This is an overview and introduction. 0:10 Acute pancreatitis is inflammation of the pancreas by enzyme-mediated oto 0:16 digestion. 0:18 Pancreatitis is mild in 80% of cases, but 20% develop serious complicated life- 0:23 threatening 0:24 diseases. 0:25 The inflammation ranges from mild edema to peri-pancreatic necrosis. 0:33 Goldstones and ethanol are the major causes of acute pancreatitis. 0:43 Here is a patient with epigastric pain, hunched over, and has been nauseous and 0:49 has vomited. 0:50 He is suspected of having pancreatitis. 0:53 What is the pancreas? 0:56 Well the pancreas is an organ that sits behind the stomach, situated partly 1:02 retroperitoneal. 1:03 Here is the liver, gallbladder, stomach, and the small intestine, and here is 1:12 the pancreas. 1:13 This is a close-up image of the pancreas. 1:17 The pancreas makes contact with the duodenum, which is the first part of the 1:22 small intestine. 1:24 The bile duct from the gallbladder and liver connect with the pancreatic ducts, 1:29 which then 1:30 makes its way to the duodenum. 1:33 The pancreas has two main functions. 1:36 It works as an exocrine gland, where it secretes digestive enzymes through the 1:41 pancreatic duct 1:42 into the small intestine. 1:46 And the pancreas also works as an endocrine organ by secreting hormones in the 1:51 blood, 1:52 such as insulin and glucagon. 1:56 The normal pancreas have a cluster of cells called the pancreatic asinum. 2:03 These work as the exocrine glands. 2:07 Here are cells that produce the digestive enzymes, which then travel through 2:12 the pancreatic duct 2:13 into the small intestine. 2:17 Inacute pancreatitis, there is inflammation of part of the pancreas due to a 2:22 number of 2:23 causes. 2:25 Because of the inflammation, the pancreas becomes damaged. 2:30 The asinum get damaged and release its digestive enzymes around them, resulting 2:35 in further damage 2:36 of surrounding structures. 2:39 The pancreas secretes three important enzymes. 2:43 These are proteases, amylase and lipase. 2:48 Because the enzymes are released not into the duct, but to the surrounding 2:52 pancreatic 2:53 tissue, the proteases causes damage to cell and vasculature through protein- 3:00 mediated damage. 3:02 The amylase levels increase in the blood, which is useful for diagnosing 3:08 pancreatitis, 3:10 but it is not specific. 3:13 The lipases also increase in the blood and can result in a serious complication 3:18 of fatty 3:19 necrosis of the pancreas. 3:24 The etiology of acute pancreatitis, the cause of pancreatic inflammation 3:29 mediated by enzyme 3:30 otodigestion, can be remembered by a useful acronym, GET SMASHED. 3:36 G stands for Goldstones, which can plug at the ampullovata, resulting in back 3:42 flow of 3:42 bile and pancreatic juices into the pancreas. 3:46 E is for ethanol. 3:49 Goldstones and ethanol are the two most common causes of acute pancreatitis. 3:54 T is for trauma, S for anabolic steroids, M for mumps virus, A for O2 immune 4:02 diseases, 4:04 S for scorpion venom, H is for hypercalcemia and hyperlipidemia, E is for ERCP, 4:13 which is 4:14 an investigation method and treatment method used for pancreatitis, and D is 4:22 for drugs, 4:23 as certain medications can trigger acute pancreatitis. 4:28 Acute pancreatitis typically presents with the following signs and symptoms, 4:33 including 4:33 vomiting, gradual or sudden severe epigastric central pain, the pain can rad 4:42 iate to the 4:43 back in 50% of cases, tripotting position relieves some pain, tachycardia, j 4:50 aundice 4:51 and fever may also occur. 4:55 Investigations to be performed in suspected acute pancreatitis include serum am 4:59 ylase 4:59 and lipase, which as mentioned, increase in the blood, serum lipase is more 5:06 specific 5:06 for the pancreas. 5:09 An ultrasound of the pancreas can also be performed and an arterial blood gas. 5:18 The management of acute pancreatitis. 5:21 Firstly, do not feed the patient by mouth, nasogastric tube can be used. 5:29 Information for administration of fluids as well as anti-emetic agents and pain 5:35 relief 5:36 with analgesia such as morphine. 5:40 Urinary catheterization is important in monitoring urine output. 5:45 Further, monitoring include daily serology of full blood count, amylase levels 5:51 and EUC. 5:54 Poorly blood pressure, heart rate and urinary output is also advised. 6:01 Complications of acute pancreatitis include chronic pancreatitis, pancreatic 6:08 ascites. 6:09 Another important complication of pancreatitis involves the lungs. 6:14 Because the pancreas sits below the diaphragm under the lung, inflammation that 6:18 occurs can 6:19 spread locally and cause acute lung injury. 6:24 These pancreatitis can result in fistula forming between the pancreas and the 6:28 parietal pleura 6:30 of the lungs. 6:32 This results in effusion in the pleural cavity. 6:35 This is called pancreatic effusion. 6:38 Other complications include acute renal failure and infected pancreatic nec 6:44 rosis, which is 6:45 related to 80% of deaths. 6:50 And also, there was fatty necrosis, which I mentioned earlier.