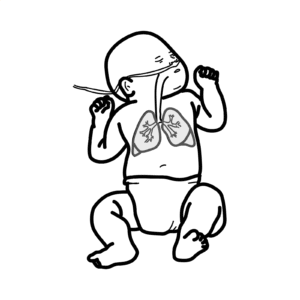
0:00 Bronchiolitis is inflammation of the bronchioles, and is often caused by a 0:10 viral infection, 0:11 notably respiratory syncytial virus, RSV. 0:15 Bronchiolitis is the most common respiratory tract infection of neonates, and 0:18 is usually 0:19 self-limiting. 0:21 A major source of confusion of treatment is differentiating a viral bronchiol 0:24 itis to asthma. 0:27 In summary, bronchiolitis is usually seen in infants less than 2 years old, and 0:31 asthma 0:31 is seen in older children. 0:34 The main causative agents is the respiratory syncytial virus. 0:38 Other causes include rhinovirus and para-influenza virus. 0:43 The respiratory tract begins with the nasal cavity and oral cavity. 0:48 Oxygen inhaled travels through this area, the upper respiratory tract, and then 0:53 down 0:53 the lower respiratory tract. 0:55 The lower respiratory tract begins with the larynx. 0:58 The larynx continues to become the trachea, and then the trachea bifurcates 1:02 into the bronchi, 1:04 and then smaller bronchi, and then bronchioles, before terminating as an alveol 1:11 us. 1:11 A normal bronchiol have smooth muscle cells around it, which help in 1:16 contraction of the 1:17 bronchiol. 1:19 The inside of the bronchioles are lined by mucus, produced by goblet cells. 1:26 Bronchiolitis is inflammation of the bronchioles. 1:30 Something similar called bronchitis is inflammation of the bronchi, and 1:35 typically affects older 1:37 people who smoke and not infants. 1:42 In bronchiolitis, the changes include narrowing of the airways due to mucous 1:47 hyper secretion, 1:48 cell wall thickening, and smooth muscle contraction. 1:53 These findings are also seen in patients who have asthma. 1:58 And in infants around two years old, bronchiolitis can often be mistaken as 2:05 asthma. 2:05 Bronchiolitis also causes air trapping, where oxygen can be inhaled but gets 2:12 trapped in 2:12 the lower respiratory tract in the alveolus, due to surrounding inflammation. 2:19 This causes difficulty breathing for the infant. 2:24 Respiratory syncedial virus is the major cause of bronchiolitis. 2:28 A single stranded RNA virus is spread through airborne droplets or direct 2:33 contact with respiratory 2:35 secretions. 2:36 A respiratory syncedial virus infection begins with replication of the virus in 2:41 the nasopharynx, 2:42 causing caraisal symptoms. 2:45 A lower respiratory tract infection can begin one to three days later. 2:50 The virus spreads to the bronchioles, where small bronchiolar epithelium line 2:56 the small 2:56 airways. 3:00 If a lower respiratory tract infection occurs, the virus causes an inflammatory 3:05 response. 3:08 Immune cells infiltrate the area. 3:12 The inflammatory response causes edema, increased mucus production from goblet 3:17 cells, and eventually 3:19 necrosis and regeneration of these epithelial cells. 3:25 This leads to small airway obstruction, air trapping, and increased airway 3:32 resistance. 3:33 These pathological features lead to the signs in bronchiolitis. 3:41 Bronchiolitis can be mild, moderate, or severe, depending on the clinical 3:45 presentation. 3:46 Infants with mild to moderate bronchiolitis typically are tech-abnique, have a 3:52 fever, 3:52 and have signs of increased work of breathing, such as nasal flaring, tracheal 3:58 tug, intercostal 4:00 recessions, and abdominal breathing. 4:04 On excultation, they can have inspiratory crepitations and a wheeze. 4:12 Severe bronchiolitis is concerning, and the infants appear very unwell. 4:17 They can have a very high respiratory rate, or a low respiratory rate, and even 4:23 apnea, 4:23 which are episodes where they stop breathing altogether. 4:28 There is severe grunting, and may be sinosis and paleness as well. 4:33 The child has difficulty feeding, taking in less than 50% or normal feeds. 4:38 All these features are concerning, and all these features indicate severe bron 4:44 chiolitis. 4:45 Risks fact is for severe bronchiolitis, or those with high risk of illness 4:50 include the 4:50 young, especially less than 6 weeks, old, premature infants, or low weight for 4:58 gestation, immunodeficient 5:00 infants, and those with congenital heart disease, neurological conditions, and 5:05 rachronic respiratory 5:07 illness. 5:09 The differential diagnosis is important, especially if an infant presents with 5:14 recurrent bronchiolitis, 5:15 or has a severe respiratory tract infection. 5:19 Structural diagnosis include acute asthma, viral-induced whees, pneumonia, 5:24 congestive 5:25 heart failure, and pertussis. 5:29 The diagnosis of bronchiolitis is clinical. 5:33 An infant or child less than two years of age presenting with initial symptoms 5:37 and signs 5:38 of upper respiratory tract infections, followed by a cough, tachypnea, and 5:43 spiritual crepitations, 5:45 and wheeze is likely to have bronchiolitis. 5:48 There is usually no role in investigations, unless the infant has a severe bron 5:53 chiolitis 5:54 or something else is expected. 5:58 Management is largely supportive, focusing on maintaining oxygenation and hyd 6:02 ration of 6:03 the patient. 6:04 Evidence suggests no benefit from broncholitis or corticoid use, in infants 6:09 with the first 6:10 episode of bronchiolitis. 6:12 Mild bronchiolitis is easily managed at home, important to encourage oral 6:17 intake. 6:18 Moderate bronchiolitis with increased work of breathing can be monitored in the 6:22 hospital, 6:23 and paracetamol and ibuprofen can be given for temperature and for symptom 6:28 relief. 6:29 Oxygen can be given to maintain oxygen saturation above 92. 6:34 It's important to encourage oral hydration, and if not, consider nasogastric 6:41 feeding. 6:42 Bronco dilators and corticosteroids again are not recommended for infants with 6:47 bronchiolitis. 6:48 For older children, you can consider bronchiolitis for symptom relief. 6:53 If oxygen levels are still low, consider high-flow nasal prongs. 6:59 Severe bronchiolitis will require oxygen via high-flow nasal prongs or even a 7:03 continuous, 7:04 positive, airway pressure CPAP. 7:09 Nasogastric tube or IV cannulation is important to keep up with the fluids. 7:14 Cygen will require admission to hospital and potentially further investigations 7:21 . 7:21 Persistent hypoxemia will require ICU referral. 7:26 Most cases of bronchiolitis resolve without complications, however, some 7:30 complications 7:30 can include dehydration, apnea, particularly in infants born prematurely, and 7:38 then obviously 7:39 secondary bacterial infections.