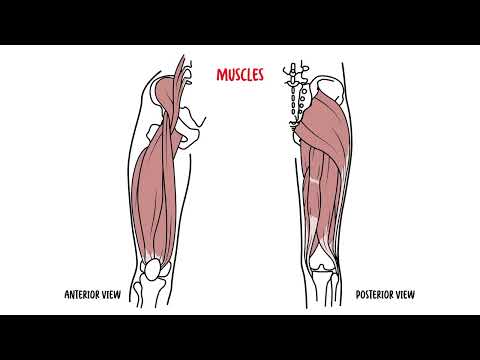
0:00 Hello, in this video we're going to look at the lower limb anatomy and this is 0:11 an overview 0:11 and we'll primarily look at the bones and also some common clinical pathologies 0:17 . 0:17 So here I'm drawing the lower limbs from the pelvis down. 0:22 I am drawing the hip bone, the bony pelvis, which is made up of three parts, 0:27 the ilium, 0:28 thoracium, and pubis. 0:31 The sacrum at the back here joins with the ilium, or the pelvic bone, at the 0:38 sacroiliac 0:39 joint. 0:40 This structure here is the iliac crest, which can be felt when you feel the 0:45 sides of your 0:46 hips. 0:47 And this whole region of the pelvis is actually the ilium. 0:51 The opening of the bony pelvis here is the pelvic brim. 0:56 The pelvic brim differs to the pelvic inlet, which is situated more inferior. 1:04 Now the pubic symphysis is here connecting the pubis area of the hip bone 1:09 together. 1:10 The symphysis is an important landmark, keep note of this. 1:15 Another important structure is the pubic tubercle and I will get back to this 1:21 later. 1:22 Here is the ischioropubic remis, which is essentially the ischium part of the 1:28 hip bone. 1:29 An important surface landmark, which can be felt at the tip of the iliac crest 1:33 anteriorly, 1:34 is the anterior superior iliac spine, or ASIS. 1:41 And somewhat below the ASIS is the anterior inferior iliac spine, or AIS. 1:49 Now the ASIS and pubic tubercle is important, because the inguinal ligament 1:56 runs along here 1:57 and attaches to these two points. 2:00 The middle of the inguinal ligament is called the midpoint of the inguinal lig 2:05 ament, and 2:05 this is an important landmark to remember. 2:09 This should not be confused for the mid inguinal point, which is an imaginary, 2:15 which is a point 2:17 along an imaginary line running from the pubic symphysis to the ASIS. 2:24 The middle of this imaginary line is the mid inguinal point. 2:29 And this is also important landmark, and we will discuss it later. 2:36 So that was for the hip, now for the femur. 2:39 Now the femoral head articulates with the acetabulum, which is a socket formed 2:43 by the 2:43 hip bone. 2:45 The hip joint is a ball and socket joint. 2:48 Important part of the femur to know are the greater trochanter, lesser trochan 2:53 ter, and 2:55 at the distal part of the femur, we have the lateral and medial pondiles. 2:59 There is, of course, the acesumoid bone in the infamous patella. 3:05 Now the patella essentially works by protecting the knee joint, but its primary 3:10 functional 3:11 role is in knee extension. 3:13 The patella actually increases the leverage that the tendon can exert on the 3:18 femur by increasing 3:19 the angle at which it acts. 3:22 Then there is a tibia and the fibula, the bones of the legs. 3:26 As you can see, the fibula doesn't actually articulate with the femur, it's 3:31 really only 3:31 the tibia. 3:33 Now the distal part of the tibia forms the medial malleolus, and the distal 3:38 part of the 3:39 fibula forms the lateral malleolus. 3:45 Now let's go to the bones of the foot. 3:48 The tarsus are a group of bones in the foot, which include the calcaneus, talus 3:56 , and cuboid. 3:57 Medially there is the navicular and cuneiforms, which are made up of three 4:02 bones, the medial, 4:04 intermediate, and lateral cuneiforms. 4:08 Next to the tassels, there are the metatarsals. 4:11 And finally, at the most distal part of the foot, the phalanges. 4:17 So I hope that made all sense, let's just go back to the hip bone again. 4:22 So here again I am drawing the left side of the hip. 4:27 Here is the pubic syphysis, and here the pubic tubercle. 4:32 And this is the anterior superior iliac spine, the ASIS. 4:37 And remember, the inguinal ligament runs between the ASIS and the pubic tuber 4:43 cle. 4:44 The midpoint of the inguinal ligament is an important landmark, because right 4:51 above it 4:52 surgeons know whether the deep inguinal ring is situated. 4:57 So remember, at the midpoint of the inguinal ligament, right above it is the 5:02 deep inguinal 5:03 ring, and the deep inguinal ring is a site where hernias can occur, 5:08 specifically indirect 5:10 hernias. 5:12 This is where in test dimes, the test dimes can go through essentially the deep 5:17 ring, 5:17 and then through the superficial ring and into the scrotum. 5:23 This is one of the reasons why the midpoint of the inguinal ligament is an 5:27 important landmark 5:28 to identify where the deep inguinal ring is. 5:33 So we are right now focusing on clinical anatomy, the surface anatomy. 5:39 The other important landmark is where we draw an imaginary line between the pub 5:44 ic symphysis 5:46 and the ASIS. 5:47 The middle here is the mid inguinal point. 5:51 Now the mid inguinal point is slightly medial to the midpoint of the inguinal 5:56 ligament. 5:57 The mid inguinal point is important because below it runs the femoral artery 6:02 which can 6:03 be palpated. 6:05 And here is the femoral artery. 6:09 Once the femoral artery is identified, you just have to move medially towards 6:14 the groin 6:15 and you will find the femoral vein and then the femoral canal where lymphatics 6:22 run. 6:23 There is an acronym navy to help you remember the sequence of the structures 6:30 and navy involves 6:31 also the femoral nerve which is the most lateral part and runs down the ileoso 6:41 is muscle. 6:42 So lateral to medial, the structures can be remembered as navy. 6:47 Then for femoral nerve, A for artery, V for vein, and Y for lymph. 6:56 The femoral artery is important because this can be an access for stenting of 7:02 the heart 7:03 and the aorta. 7:04 Similarly, the femoral vein is important because it is an access for central 7:10 lining. 7:11 And to find all these structures, you just need to remember the mid inguinal 7:15 point which 7:15 is where the femoral artery is located and then you can work medially. 7:19 During the same diagram again, I am adding the femoral head and part of the fem 7:26 ur here. 7:27 Again here is your femoral artery, vein, and lymph remember. 7:33 There is a fascia type thing that runs over these structures which it makes 7:38 actually an 7:39 opening here and this opening right below the inguinal ligament is called the 7:45 saphenous 7:45 opening. 7:46 And as you expect, this is where the great saphenous vein goes through. 7:52 Now the great saphenous vein drains into the femoral vein which if you remember 8:00 is medial 8:01 to the femoral artery. 8:04 The great saphenous vein actually originates or attaches from or comes from the 8:11 medial 8:11 malleolus and drains, just comes right up and drains into the femoral vein here 8:19 . 8:20 Clinical anatomy. 8:22 Femoral hernia is where there is weakening of the femoral canal. 8:27 The femoral canal if you remember is where the lymphatics run and the femoral 8:34 canal is 8:35 situated medial to the femoral vein. 8:38 The femoral canal can allow intestines to go to enter the canal and go down and 8:45 out through 8:45 the saphenous opening causing a femoral hernia. 8:51 The hernia is more common in women than men and have an increased risk of 8:55 strangulation 8:57 because of the rigid and narrow femoral canal. 9:01 To finish this diagram off, there is a muscle here called the psoas major which 9:06 originates 9:06 from the vertebrae, the spine, actually specifically the lumbra vertebrae. 9:11 And so it goes from the lumbra vertebrae and it goes down into the pelvic area 9:16 and joins 9:17 with another muscle called the iliacus, and these two will form partly the 9:23 muscle known 9:24 as iliosaurus. 9:26 And if you remember iliosaurus is the muscle where the femoral nerve runs along 9:32 . 9:33 And essentially these muscles will then all join to the lesser trochanter of 9:40 the femur. 9:41 Why am I telling you this? 9:42 Well the psoas muscles are important because a condition can arise called psoas 9:47 absis. 9:48 So why am I talking about psoas absis? 9:50 Well psoas absis can present with a small lumb potentially but mainly pain, 9:56 pain around 9:57 the hips with or without fever. 10:02 And the major cause of psoas absis is tuberculosis or by enteric bacteria. 10:10 Also bacteria from the GIT can cause psoas absis. 10:15 And an example can be if a patient has diverticulitis and ruptures and so 10:22 creates a sort of tunnel 10:24 where the bacteria can enter the absis, the psoas muscles. 10:32 So next I want to talk about the hip joint and I want to introduce the lig 10:36 aments. 10:37 The hip joint is very stable. 10:39 Here are the three parts of the bony pelvis, the ilium, hubis and ischium which 10:45 I described 10:46 at the beginning of the video. 10:47 And this is the femur. 10:49 The head of the femur is within the acetabulum. 10:53 The hip joint is a ball and socket joint. 10:56 There are ligaments that support the ball and socket joint. 10:59 And there are three main ligaments and are named by where they connect to and 11:05 from. 11:06 So the first ligament is from the femur to the ilium. 11:09 And this is called the ileophimoral ligament. 11:13 The next ligament is from the pubis to the femur. 11:15 This is called the pubofimoral ligament. 11:17 And the third ligament which cannot be seen here is actually at the back and is 11:23 the ligament 11:24 from the ischium to the femur. 11:25 And this is called the ischofimoral ligament. 11:30 So again there are three major ligaments that support the hip joint. 11:35 The clinical anatomy of the hip joint will be discussed in a separate future 11:38 video hopefully. 11:40 Let's look more closely at the knee joint now. 11:43 So here is the right fibula, the right tibia, the tibial tuberosity and the p 11:50 atellar. 11:51 There is a patellar ligament which is a continuation from the quadriceps tendon 11:57 . 11:57 The patellar ligament attaches and continues with the tibial tuberosity. 12:02 And as mentioned the patellar ligament is actually a continuation of the quad 12:06 riceps tendon. 12:07 Which is formed from muscles of the anterior thigh which includes the quadrice 12:14 ps femoris 12:15 and the vastus muscles. 12:18 Now between the femur and the tibial bones there is a cushiony type substance 12:22 called the 12:22 meniscae. 12:23 And these are essentially college. 12:25 There is a medial meniscus and a lateral meniscus. 12:30 And here we have the medial condyle and lateral condyle. 12:35 Here is the lateral collateral ligament and here is the medial collateral lig 12:40 ament. 12:40 There is also another two collateral ligaments which is under the patellar, the 12:45 anterior collateral 12:45 ligament and the posterior collateral ligament. 12:48 It is important to know these ligaments and the meniscus because they can be 12:54 injured during 12:55 sporting activities or with certain maneuvers. 12:59 It is important to note that some branches of the medial collateral ligament 13:06 joins and 13:07 continues with the medial meniscus. 13:10 And so when the medial collateral ligaments are damaged, part of the medial men 13:15 iscus can 13:16 also be damaged. 13:19 So now I am just going to draw the same knee joint again. 13:22 Here again is the patellar ligament and here is the quadriceps tendon which is 13:27 formed by 13:30 the anterior muscle compartments of the thigh. 13:34 Under the rectus femoris there are a group of muscles, the vastus muscles and 13:41 we have 13:42 the vastus lateralis, vastus intermedius and vastus medialis which forms the 13:47 quadriceps 13:47 tendon, part of it. 13:49 And then this will then continue to the patellar ligament that runs through and 13:54 joins with the 13:55 tubule tuberosity. 13:57 It is important to point out that the vastus medialis is one of the strongest 14:02 muscles for 14:02 stabilizing the knee joint. 14:05 Clinical anatomy, weakness of the vastus medialis can cause the patellar to 14:12 track laterally. 14:14 The second clinical anatomy regarding the knee joint is a condition called Osk 14:18 ud Schlatter 14:19 syndrome which occurs in young children in particular. 14:23 It is where there is inflammation of the tibial ligament at the tibial tuber 14:28 osity. 14:29 This usually is self resolving and leads to a lump forming where the tibial 14:33 tuberosity 14:34 is quite a prominent lump. 14:37 Finally, let's talk about the ankle joint. 14:40 Here we are looking at the posterior view of the ankle joint. 14:44 So from the back, here is the tibia, the fibula, the talus calcaneus, the 14:51 medial malleolus. 14:53 The ligaments visible here are the deltoid ligaments medially. 14:58 A ligament that runs from the fibula and tibia is at the back here is the 15:03 posterior tibio 15:05 fibula ligament. 15:07 There is also an anterior one which is not visible of course. 15:11 Another ligament from the fibula to the talus is the posterior talofibular lig 15:17 ament. 15:18 There is an anterior talofibular ligament as well but it is not visible of 15:24 course. 15:25 And here is the ligament from the calcaneus to the fibula called the calcaneof 15:29 ibular ligament. 15:32 As mentioned, there is also the anterior talofibular ligament and it is very 15:36 important 15:36 to know this one remember. 15:39 And the reason being is when you have a rolling of your ankle to the inside, so 15:45 inversion, 15:46 the ligament most commonly injured is the anterior talofibular ligament. 15:53 And that's a good exam question. 15:55 So through inversion, you can get an anterior talofibular ligament here. 16:00 The ligament, remember, is located on the lateral side. 16:06 And again this is the most common injury through foot inversion. 16:11 But then you can have a traumatic inversion. 16:15 And this can cause distal fibula fracture together with ligament tears mainly 16:21 involving 16:21 the anterior talofibular ligament. 16:26 I hope you enjoyed this video on the overview of the lower limb, thank you for 16:30 watching.