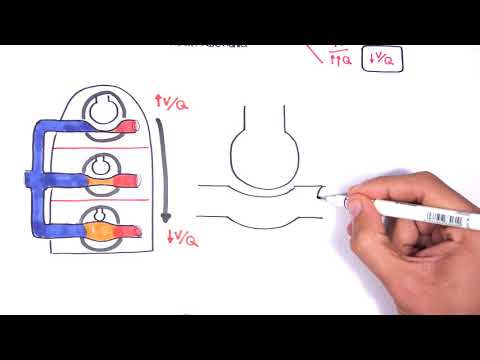
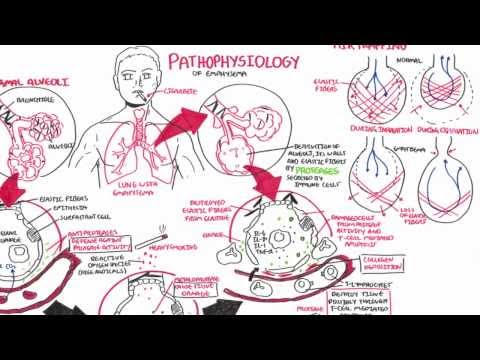
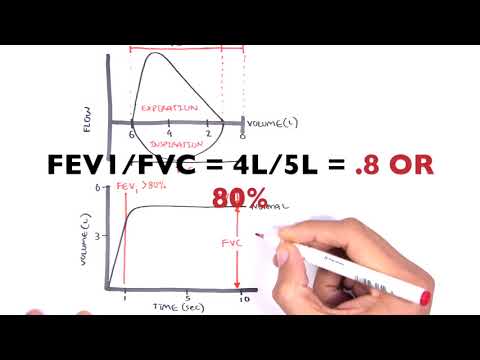
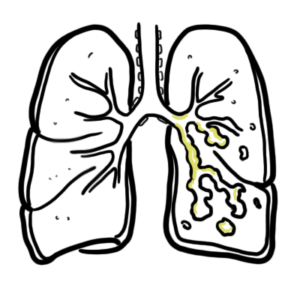
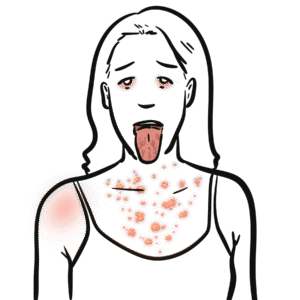
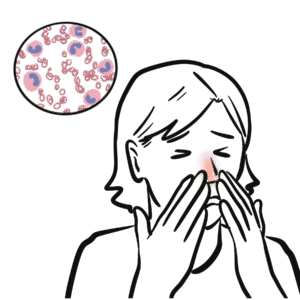
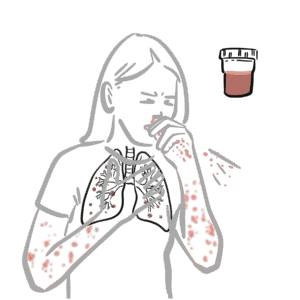
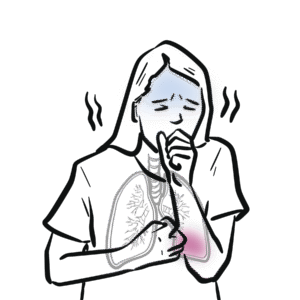
0:00 COPD, or chronic obstructive pulmonary disease, is a common respiratory 0:09 condition involving 0:10 the airways and is characterized by airflow limitation. 0:15 Exacerbations and comorbidities contributes to the overall severity in 0:20 individual patients. 0:22 Let's look at the signs and symptoms of COPD. 0:25 So patients with COPD present usually with three cardinal symptoms. 0:31 And these are dyspnea, chronic cough, and sputum production. 0:35 Less common symptoms include wheezing and chest tightness. 0:40 Risk factors for COPD include smoking in 95% of cases. 0:45 So it's a big risk factor. 0:47 There's also air pollution, low birth weight, recurrent lung infections, and 0:52 cannabis smoking. 0:54 Low socioeconomic status and alpha-1 anti-trips and deficiency are also risk 1:00 factors for COPD. 1:02 COPD, again, stands for chronic obstructive pulmonary disease and encompasses a 1:06 variety 1:07 of diseases. 1:09 The big three COPD chronic obstructive pulmonary diseases are chronic asthma. 1:16 The blue bloaters, which is the chronic bronchitis and the pink puffers, which 1:21 is emphysema. 1:23 In this video, we will mainly focus on the blue bloaters and pink puffers. 1:28 But before looking at these two, let us quickly revise asthma, and I have a 1:33 video that actually 1:34 looks into more detail on asthma, if you're interested. 1:38 So asthma, it's a chronic inflammatory disorder of the airway in which many 1:43 cells and cellular 1:43 elements play a role. 1:46 Recurrent episodes of wheezing, breathlessness, chest tightness, and coughing 1:51 are only signs 1:52 and symptoms of asthma. 1:54 So now we will talk about the blue bloaters and the pink puffers. 2:00 And here I am drawing a diagrammatical, yes, representation, a stereotypical 2:06 representation 2:07 of patients that present with chronic bronchitis, as well as emphysema side-by- 2:13 side blue bloaters 2:15 and pink puffers. 2:16 We will use this to compare the difference between the two chronic obstructive 2:23 pulmonary 2:24 diseases, beginning by looking first at the blue bloaters. 2:30 So the blue bloaters, these are patients that look very sinosed blue, bloaters, 2:37 possibly 2:38 potentially due to the dyspnea, severe dyspnea, and lack of exercise. 2:43 So in chronic bronchitis, you have inflammatory change leading to mucocillary 2:49 dysfunction 2:49 and increased goblet cell secretion and numbers, which leads to excessive mucus 2:56 production. 2:58 So if we look at a normal alveoli, it has oxygen coming in and carbon dioxide 3:04 going out, 3:05 normal ventilation and perfusion. 3:09 These are alveoli and it has elastic fibers surrounding the alveoli, which is 3:14 important 3:15 for basically the air recoiling during expiration. 3:20 So in the exhale, it recalls back pushing the air out and we breathe this 3:25 carbon dioxide 3:26 out. 3:28 Now if we look at an alveoli and the bronchioles of a chronic bronchitis 3:32 patient, we can see 3:33 big differences. 3:36 In the bronchioles and bronchioles, we see bronchoconstriction and mucus hyper 3:42 secretion. 3:43 The mucus hypersecretion leads to the productive cough in chronic bronchitis. 3:50 The airway is obstruction from bronchoconstriction and mucus leads to wheezing. 4:00 And we hear wheezing during expiration typically. 4:04 When we have airway obstruction, this also can mean that we have alveolar hypox 4:10 ia because 4:11 oxygen is not getting through to the alveoli efficiently. 4:15 This leads to a VQ mismatch. 4:19 The VQ mismatch leads to hypoxemia and hypercapnia. 4:27 Hypercapnia means respiratory acidosis. 4:29 A decrease in oxygen in the blood means the body will try to make more red 4:34 blood cells 4:35 to compensate. 4:37 This is known as polycythemia where we get an increase in hemoglobin. 4:42 The respiratory acidosis and polycythemia with the decrease in oxygen 4:48 contributes and 4:49 basically means sinosis, the blue color. 4:53 And this is why these patients with chronic bronchitis are known as the blue 4:58 bloaters. 4:59 So just recapping, chronic obstruction means that during respiration less 5:05 oxygen comes 5:07 in and less carbon dioxide goes out, which leads to decrease in oxygen in the 5:12 blood and 5:12 increase in carbon dioxide in the blood. 5:16 Because in chronic bronchitis, oxygen is not properly getting into the alveoli, 5:20 we get 5:20 alveolar hypoxia. 5:23 When this happens, the pulmonary vessels will constrict so that it can shunt 5:28 the blood flow 5:29 to healthier alveoli. 5:32 But when you get pulmonary vasoconstriction, you can get an increase in 5:37 pulmonary vascular 5:38 pressure, so pulmonary hypertension. 5:42 When you get pulmonary hypertension, this can cause backflow of blood to the 5:47 right side 5:47 of the heart and this can cause right-sided heart failure, which causes your 5:54 core pulmonale, 5:55 leading to the increase in jugular venous pressure. 6:00 If that, I hope that makes sense. 6:02 Now going back to the alveolar hypoxia again, remember that the pulmonary vas 6:09 oconstriction 6:10 of some vessels leads to the pulmonary hypertension. 6:14 So pulmonary hypertension leads to less blood going to the left side of the 6:20 heart, which 6:20 means there can be a decrease in left ventricular cardiac output and this means 6:26 a decrease in 6:27 circulatory volume. 6:29 Now a decrease in circulatory volume results in the activation of the renin ang 6:34 iotensin 6:34 aldosterone system, which causes more fluid retention despite still having 6:40 fluid piling 6:41 up in the lungs. 6:43 And of course this is in more severe cases. 6:48 So I hope that all made sense. 6:50 So that was for the blue bloaters chronic bronchitis and they are sinosed, they 6:57 present 6:58 with wheeze and also productive cough, not productive but very prominent cough. 7:05 Now let us look at emphysema, emphysema are known as the pink puffers, very 7:11 skinny muscle 7:13 wasting, but prominent thoracic cage, barrel chested, and we will see why. 7:22 So emphysema is an inflammatory response, which leads to elastic fiber 7:26 breakdown and 7:27 destruction of the alveolar walls, which means loss of alveolar integrity. 7:33 And so we lose alveolar recoil as well. 7:37 This leads to a phenomenon known as air trapping, which is typical of emphysema 7:42 patients. 7:43 So if that all did not make sense, we will look at it in a diagram. 7:48 So let us draw the same diagram as before with the bronchiol and the alveolus 7:55 here, and 7:55 it is pulmonary supplied. 7:57 Now within the alveolus there are macrophages normally reciting in there, 8:02 helping to keep 8:02 the place clean and sterile. 8:06 And normally again oxygen comes in and carbon dioxide goes out. 8:12 Now with emphysema, due to smoking or inhalation of pollution or other toxic 8:16 substances, the 8:17 macrophages can become stimulated and begin secreting proteases and cytokines, 8:22 which lead 8:23 to a number of things. 8:26 The cytokines released attract neutrophils from circulation to move into the 8:32 area. 8:32 The neutrophils as a consequence begins secreting a special protease called el 8:37 astase, which 8:38 specifically targets the elastic tissues. 8:42 So elastase secreted by the neutrophil leads to loss of elastic fibers around 8:48 the alveolus, 8:49 which would mean loss of elastic recoil, which means decrease in ventilation. 8:58 The protease is secreted by macrophages and the neutrophils also lead to the 9:03 destruction 9:04 of the alveolar wall and capillary beds. 9:08 The destruction of the capillary beds leads to a decrease in perfusion. 9:14 And so as you might realize, we have a big problem with the ventilation and 9:18 perfusion 9:19 ratio. 9:21 The loss of elasticity and destruction of alveolar wall leads to air trapping. 9:27 Air trapping is basically when you still have a lot of gas trapped in the alve 9:31 olus, after 9:32 you expire, after you exhale. 9:36 So you have oxygen and carbon dioxide trapped there still, after you exhale. 9:41 This means you have an increase in n-expertory volume. 9:48 So because you have an increase in n-expertory volume, this leads to one of the 9:55 clinical 9:56 signs of emphysema, which is barrel chest, because you are not emptying your 10:01 lungs, you 10:02 still have gas trapped, and you're using accessory muscles and a lot of effort 10:08 in breathing. 10:10 All these together lead to the barrel chest. 10:13 Okay, so the decrease in perfusion and the decrease in ventilation, which we 10:18 talked about 10:18 earlier, leads to a matched VQ deficit. 10:23 As a result of this deficit, in the blood, you see similar things to chronic 10:28 bronchitis, 10:29 a decrease in oxygen and an increase in carbon dioxide in the blood. 10:36 So recapping what we just drew on the diagram, the protease is released by mac 10:40 rophages and 10:41 neutrophils, damages the elastic fibers leading to decrease in elastic recoil, 10:46 which means 10:46 a decrease in ventilation. 10:48 The protease is also destroys capillary beds, which means a decrease in perf 10:54 usion. 10:55 decrease in ventilation and perfusion means we have a matched VQ deficit. 11:00 As a result of this VQ matched deficit, we get hypoxemia and hypercaponemia. 11:05 I think that's what you said. 11:07 Hypoxemia and hypercapnia in the blood becomes more severe in late stage. 11:13 The loss of elastic recoil is due to the loss of alveolar integrity and the 11:17 destruction 11:18 of the alveolar walls, and so the person needs to work a lot harder to breathe 11:25 in. 11:25 As a result, we get dysnia and also capaxia. 11:29 Now alpha-1 anti-tripsin deficiency is a hereditary condition, which means that 11:34 if you 11:34 are deficient in anti-tripsin, you cannot defend against proteases. 11:39 And so you have a net too much protease and less anti-protease, which means you 11:45 get a 11:46 net damage to your lungs, essentially. 11:49 So I hope all that makes sense about infasema. 11:52 So infasema are your pink puffers, chronic bronchitis are your blue bloaters. 11:57 Now let's proceed to investigations. 12:01 What sort of investigations would you perform if someone presents with 12:04 difficulty breathing, 12:05 sputant production, as well as a cough? 12:16 [BLANK_AUDIO]