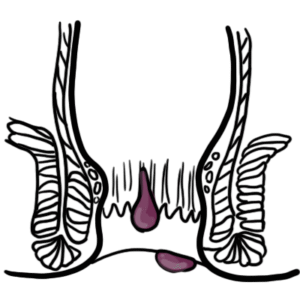
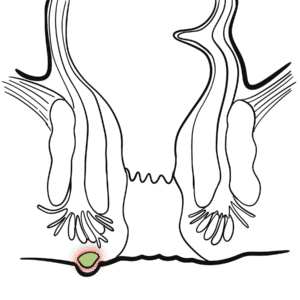
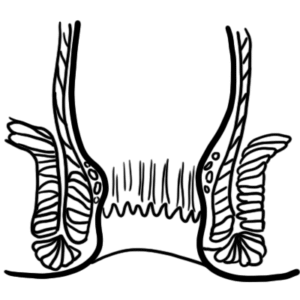
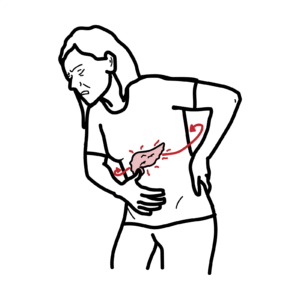
0:00 Diverticular disease is where you have outpouchings of the colonic mucosa and 0:09 underlying connective 0:10 tissue through the colon wall. 0:13 Diverticular disease are acquired outpouchings which make them a false divert 0:19 icular and we 0:20 will compare between true and false in this video. 0:24 Let's begin by first recapping the anatomy of the colon. 0:29 Here we have the cecum, the beginning of the colon, ascending transverse, 0:33 descending sigmoid 0:35 and the rectum. 0:36 It's important to note that the sigmoid is where most diverticular occur in the 0:42 western 0:43 country. 0:44 However, in Asian populations it occurs more predominantly on the right side, 0:48 so around 0:49 the ascending and the hepatic fluctuations/transverse colon. 0:54 Before I continue it is important to know the terminology. 0:58 So a diverticulum is one outpouching, diverticula is plural, multiple outpouch 1:07 ings, diverticulosis 1:09 is the presence of diverticula which is usually asymptomatic, so no symptoms. 1:16 And diverticula disease is an umbrella term which can present as either sympt 1:22 omatic or 1:22 asymptomatic and it's an umbrella term for a variety of conditions involving 1:28 the diverticula. 1:30 So let's cut a cross-section of the colon and just recap some important 1:35 structures. 1:36 The colon is made up of many layers. 1:38 Here we have the lumen and here a longitudinal muscle fiber known as a tine col 1:44 i and we have 1:45 three of these surrounding the colon and then we have blood vessels which 1:50 supply the colon 1:51 wall and these blood vessels originate from the inferior mesenteric arteries 1:56 and these 1:57 blood vessels then penetrate through part of the colon wall to supply the 2:02 surrounding 2:02 tissue. 2:05 In diverticula disease you have diverticulosis, the presence of a lot of these 2:09 outpouchings 2:10 within the colon. 2:14 These outpouchings can be divided into either true or false diverticula and 2:20 there's a difference. 2:22 The difference is that when you have a true diverticula all the layers are 2:28 involved in 2:29 the outpouching, so all the layers of the colon wall is involved in the outp 2:34 ouching. 2:35 However, in a false diverticula it's only the mucosa and the submucosa that is 2:41 involved 2:41 in the outpouching, the muscle layer remains the same and it is the false diver 2:47 ticulum 2:48 which is the acquired diverticulum and this is what we see in the adult 2:54 population whereas 2:55 a true diverticulum is what we see in infants, this is a congenital problem. 3:04 This is essentially the presence of a lot of diverticula and so this is usually 3:10 asymptomatic, 3:12 however in diverticula disease there is usually symptoms. 3:19 One of the causes of these symptoms is diverticulitis which is inflammation of 3:25 a diverticulum or 3:26 diverticula and this inflammation causes pain and some bowel problems. 3:34 If we zoom into what happens during inflammation we see the presence of neut 3:39 rophils infiltrating 3:41 the area and this leads to the signs and symptoms we see in diverticula disease 3:48 . 3:49 In diverticula disease a majority of people are asymptomatic, they have a lot 3:54 of these 3:55 outpouchings and it doesn't cause any problems, however there can be painful 4:00 diverticula disease 4:01 and this is usually pain at the lower iliac fossa on the left and this is 4:07 remember the 4:08 sigmoid area where in western countries diverticula disease predominates, 4:16 however painful diverticula 4:17 disease often coexists with irritable bowel disease and so there is some 4:24 confusion. 4:25 The third way of presentation is when there is bleeding diverticula disease and 4:30 this is 4:31 usually large volume of dark red blood. 4:35 What is the cause of this? 4:37 Well if we have many outpouchings here the blood vessels that supply the area 4:41 can rupture 4:42 so we have rupture of a peri diverticula submucosal blood vessel resulting in 4:48 the blood entering 4:50 the lumen and then going out as stool forming the large volume of dark red 4:55 blood. 4:56 The fourth way diverticula disease can present is with diverticulitis which is 5:01 in from inflammation 5:02 of a diverticula and this presents with usually nausea, fever, tachycardia, 5:10 acute left iliac 5:12 fossa pain in western countries and also loose stools. 5:18 So again those are the four ways diverticula disease can present. 5:23 Majority of people are asymptomatic causes no problems, then you have painful 5:27 diverticula 5:28 disease, you have bleeding diverticula disease and then you have diverticulitis 5:34 . 5:35 The risk factors for diverticula disease or forming diverticula include age 5:41 because it's 5:42 majority in an older population, being male, obese, having a low fiber diet, 5:48 certain medications 5:50 such as non-steroidal anti-inflammatory drugs, corticosteroids and exercise as 5:59 well. 6:00 Let us now look at the pathophysiology of diverticula disease or how a false 6:06 diverticulum 6:07 forms. 6:09 In order to do this we must zoom into the layer of the colon here and recap the 6:15 layers 6:15 of the colon itself. 6:17 So here we have the lumen, the first layer which interacts with the lumen is 6:22 the mucosa 6:22 and the submucosa. 6:24 Then we have the muscle layer, the muscularis and then the cirosa. 6:30 Remember the branches of the inferior mesenteric arteries supplies the colon 6:37 and so here we 6:38 have the artery which is a branch of the inferior mesenteric arteries supplying 6:42 the colon and 6:43 it's actually penetrating inside the colon wall to supply the mucosa and submuc 6:50 osa. 6:51 Well it's actually in this area where the artery penetrates the colon wall 6:56 where diverticulum 6:58 can form because this is essentially a weak spot. 7:02 When pressure builds up within the lumen due to various reasons the site where 7:10 the artery 7:11 penetrates the colon wall is a site of weakness and therefore a diverticulum 7:16 can form and 7:17 out pouching can form involving only the mucosa and submucosa layers. 7:24 So again here we have the penetrating artery which is a weak spot and the high 7:28 pressure 7:29 within the lumen also contributes to the formation of the diverticulum, the 7:34 false diverticulum. 7:36 It's also important to note that sigmoid where most of the diverticula occur is 7:41 the narrowest 7:42 part of the colon and so this will mean that there is greater pressure in the 7:49 area. 7:50 The pathogenesis of diverticulitis which is inflammation of a diverticulum is 7:55 thought 7:56 to be due to the microflora or fecal impactment for that matter. 8:01 So if there's an out pouching a fecal can just lodge in there and block the 8:07 site causing 8:08 some form of ischemia type necrosis and this will cause an inflammatory process 8:14 . 8:15 Or another thought is that the gut bacteria that lives within the colon 8:19 actually initiates 8:20 the inflammatory process. 8:23 Now it's important to talk about the complications of diverticula disease and 8:29 there are many 8:30 mainly abscess formation, diverticulitis itself, perforation where a divertic 8:40 ulum can perforate 8:42 and this can then lead to the formation of a fistula. 8:46 A fistula is a tunnel formed by you can say two hollow organs and in the case 8:54 of a perforated 8:56 diverticula it can actually form a fistula with the bladder and so when it 9:02 forms this 9:03 fistula with the bladder here the urinary bladder it can cause some signs and 9:09 symptoms. 9:10 This is known as a colon vesicular fistula and when this happens the bacteria 9:16 which normally 9:17 reside in the colon can go into the bladder causing UTIs and also the gas that 9:24 is being 9:25 produced can lead to bubbling when you urinate so you have bubbles in your 9:33 urine. 9:34 Investigations that are performed for suspected diverticula disease include bar 9:41 ium enema which 9:42 can reveal heaps of diverticula and also possible strictures and complications 9:48 associated with 9:49 diverticula disease. 9:51 Then you have a colonoscopy which essentially is where you have a camera 9:55 inserted into the 9:55 back passage and this is good because you can see visually visualise the colon 10:02 wall 10:02 and go all the way around the colon and you can possibly find coexisting 10:07 complications 10:08 or even malignancy. 10:11 Laboratory tests including full blood can and CRPs also used CT scan is used to 10:15 identify 10:16 complications associated with diverticula disease. 10:22 The management of diverticula disease can be divided into medical and surgical. 10:28 Medical looks at diet promoting high fibre diet and also drinking more water. 10:36 Exacerbations of diverticulaitis there may be a need for IV antibiotics, 10:41 analgesia and 10:42 fluids in hospital. 10:45 Individual management include resection, segmental, collectamy and indications 10:50 for surgery include 10:52 a perforation of a diverticula, inflammation that fails to respond to medical 10:58 treatment, 10:59 undrainable abscess and also a fistula formation. 11:15 [BLANK_AUDIO]