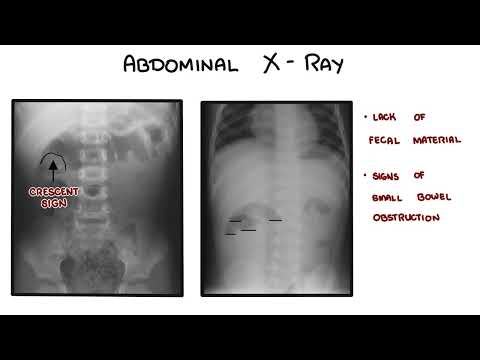
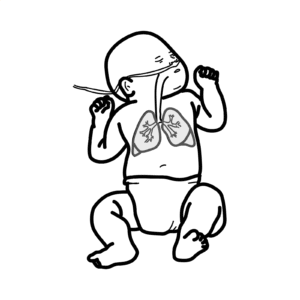
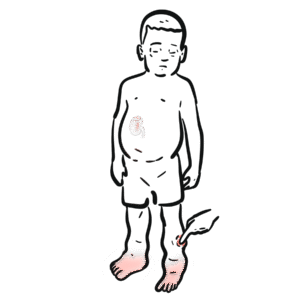
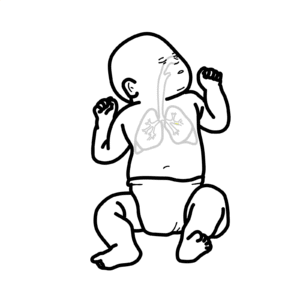
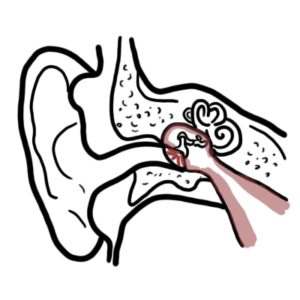
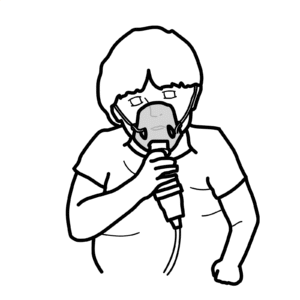
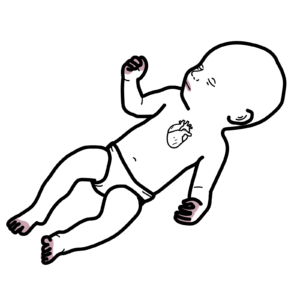
0:00 In this video, we're going to look at pediatric respiratory distress syndrome, 0:10 or RDS. 0:14 Respiratory distress is common immediately after birth, and is typically caused 0:19 by abnormal 0:20 respiratory function during the transition from fetal to neonatal life. 0:26 RDS is deficiency of alveolar surfactant, which is mainly confined to premature 0:34 babies. 0:34 RDS is responsible for most admissions to the ICU in the immediate newborn. 0:42 RDS manifests usually in the first four hours of life. 0:49 Signs include intercostal or subcostal retraction, audible grunting, tachopnea, 0:55 nasal flaring, and sinosis. 0:59 Neonatal respiratory distress may be transient. 1:04 However, persistent distress requires a rational, diagnostic, and therapeutic 1:10 approach 1:11 to optimize outcome and minimize morbidity, minimize the death of the newborn. 1:18 The functional units of the lungs are the alveoli, 1:22 which is where oxygen and carbon dioxide exchange takes place. 1:27 This process is called internal ventilation. 1:31 Certain cells in the alveoli normally produce surfactant, which is an important 1:36 product. 1:37 It's important in keeping the alveoli open by decreasing surface tension. 1:44 In RDS, the alveoli cannot produce surfactant because the lungs have not 1:50 matured yet, 1:52 or because of an abnormal gene that otherwise would contribute to the 1:57 production of surfactant. 1:59 And so during inspiration, air can fill the alveoli, 2:04 but after exhalation, the alveoli slowly collapses because the alveoli cannot 2:12 be maintained open. 2:14 And so after every exhalation, it will become harder and harder to inhale, 2:21 to inflate the alveoli, to open the alveoli. 2:25 This results in the signs and symptoms of respiratory distress syndrome, as we 2:30 mentioned earlier. 2:32 In summary, in RDS, the alveoli will collapse, resulting in respiratory failure 2:38 . 2:38 This will cause hypoxia to tissues, and eventually the heart will not function 2:44 properly, 2:44 and you will get a decrease in cardiac output. 2:47 This will result in eventual decrease in blood pressure, which will eventually 2:53 lead to renal failure. 2:55 Again, this is all a result of surfactant is insufficiency. 3:03 Surfactant is normally produced by type 2 pneumocytes. 3:07 Surfactant is important in keeping the alveoli open during ventilation. 3:12 When there is no surfactant in the newborn, this is RDS. 3:19 The risk factors for developing RDS includes premature birth, maternal diabetes 3:25 , and cesarean section. 3:30 Investigations that can be performed in suspected RDS includes a chest x-ray, 3:38 which will reveal white lungs. 3:40 It will reveal ground glass appearance, which is fluid shifting to the lung par 3:47 acima, as well as air bronchograms, 3:49 where the bronchi, the bronchioles, are visible in the center. 3:56 Differential diagnosis for RDS includes other common respiratory distress 4:01 conditions. 4:01 This includes transient tachypnea of the newborn, and this is where fluid 4:08 remains in the lung tissue 4:10 and does not shift out as it normally should after delivery. 4:14 This is often self-limiting, but infants require CPAP. 4:20 Another differential diagnosis is maconium aspiration, which occurs in the 4:26 uterus when the fetus poos, 4:28 the poo product is known as the maconium. 4:31 The fetus then aspirates the maconium, which often results in respiratory 4:37 distress after delivery. 4:39 Then there is a congenital abnormality, where a hole is present between the tr 4:45 achea and the esophagus. 4:47 This is called a fistula, and this can lead to similar signs to RDS. 4:53 This condition is properly known as tracheo esophageal fistula. 4:59 Another differential diagnosis include group B streptococcus pneumonia, 5:04 where the infant can contract group B streptococcus from a group B streptococ 5:10 cus positive mother, 5:11 following a vaginal delivery. 5:14 There are also other lung abnormalities that can contribute or mimic the signs 5:20 of respiratory distress syndrome. 5:22 The management of RDS includes oxygen therapy. 5:27 This may be all that is needed, and RDS may resolve. 5:31 However, intubation may need to be performed, especially in premature infants, 5:36 less than 26 weeks. 5:39 Prophylactic surfactant may also need to be administered to restore surfactant 5:45 in the body, 5:45 and hopefully stimulate natural surfactant secretion from the lungs. 5:51 Fluids containing 10% dextrose may be administered to restore lost fluid and 5:59 for feeding. 6:01 Finally, monitoring is always important.