Overview
Birth defects are the leading cause of perinatal and post- neonatal deaths, and result in substantial morbidity and disability in developed countries. There is a wide variety of mechanisms including genetic, environmental and multifactorial. Major birth defects affect 2–3% of live-borns, and minor birth defects affect 15%. Preventative strategies remain limited, but include maternal folic acid supplementation, reduction in teratogen exposure, alternative reproductive options, prenatal detection and neonatal screening.
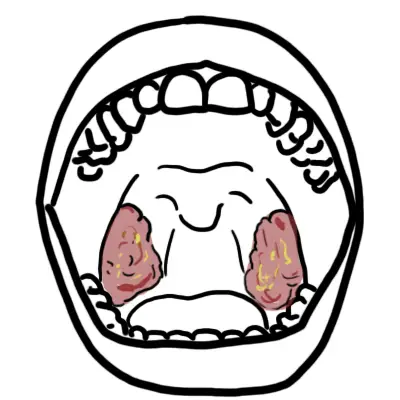
| Definition Types of structural birth defects Malformation arise during the initial formation of the embryo and fetus as a result of genetic and/ or environmental factors during organogenesis (2–8 weeks post-conception). Malformations may include failure of formation, incomplete formation or abnormal configuration. Examples include spina bifida, cleft palate and hypospadias. Disruption result from a destructive process that alters structures after formation. Examples include early amnion rupture causing amputation defects of digits, and vasoconstriction defects caused by cocaine. Deformations result from moulding of a part by mechanical forces, usually acting over a prolonged period. Examples include talipes, congenital hip dislocations and plagiocephaly associated with oligohydramnios. |
Aetiology and Risk Factors
| AETIOLOY OF BIRTH DEFECTS | |
| Mechanism | Examples |
| Whole chromosome duplication | Downsyndrome (Trisomy 21) |
| Whole chromosome missing | Turner (monosomy XO) |
| Section of a chromosome duplicated | Cat eye syndrome (Duplication 22q) |
| Section of a chromosome missing | Cri du chat syndrome (Deletion 5p) |
| Mutation of single gene | Smith-Lemli-Opitz syndrome (7-Dehydrocholesterol reductase) |
| Multifactorial/polygenic (Genes and envinroment) | Congenital Heart defect, Neural tube defect and facial cleft |
| Uterine environment | Hip dysplasia, talipes (Oligohyrdomnios) |
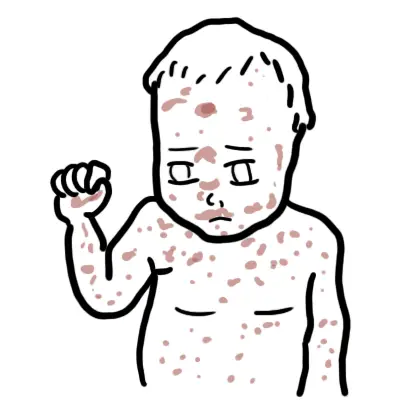
| Wider environment | Fetal rubella syndrome (Rubella infection in pregnancy) Fetal Alcohol syndrome (maternal alcohol ingestion) Microcephaly (high dose irradiation) Limb deficiency (thalidomide) |
Noonan Syndrome
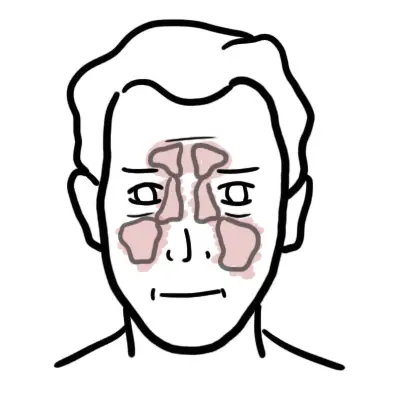
Noonan Syndrome is an autosomal dominany disorder with mutation of chromosome 11. Clinical features include characterisic facies (down slatning, palpebral fissures, widespread eyes, low set ears +/- ptosis), Short stature, pulmonary valve stenosis, webbed neck, failure to thrive, abnormalities of cardiac conduction and rhythm.
Common Birth Defects
| Common Birth Defects | Descrption |
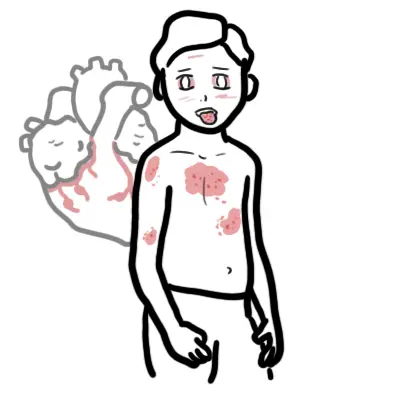
| Congenital Heart defect | |
| Development hip dysplasia | |
| Hypospadias | |
| Talipes equinovarus | |
| Hypertrophic pyloric stenosis | |
| Down syndrome | |
| Cleft lip/palate | |
| Spina bifida | |
| Tracheo-eosphageal fistula | |
| Abdominal wall defect (Exomphalos and gastroschisis) |
Approach
Approach
- History
- Antenatal History
- Perinatal History
- Postnatal History
- Social History – smoking, alcohol
- Family History – miscarriage, stillbirths, genetic diseases
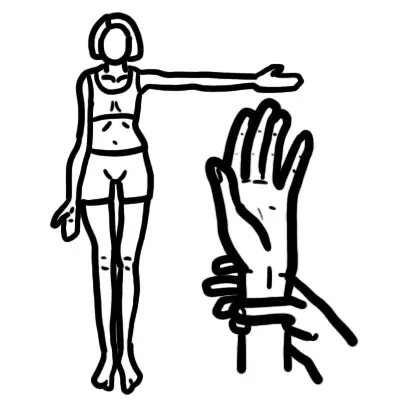
- Examination
- Head to Toe
- Mesurements
- Investigaitons
| Remember Features of Down syndrome Hypotonia, Protruding tongue, Intellectual delay, Brachycephaly, Inner epicanthal folds, Hearing loss, Short neck, Single palmar crease, 40% have cardiac anomaly. |
Prenatal Diagnosis aims at detection of birth defects prior to birth to allow options for parents. Tests fall into two main categories:
- Screening tests
- Ultrasound
- Nuchal translucency screening
- Diagnostic tests.
- Aminocentesis
- Chorionic villus sampling
- Fetal blood samples
- Organ biopsies
- MRI
- Ultrasound
Teratogens
Overview Teratogens is an environmental agent that can cause abnormalities of form or function in an exposed embryo or fetus (examples: sodium valproate and alcohol). Estimated ~ 1% and 3% of birth defects may be related to teratogenic exposure.
- <2weeks after contraception – exposure of teratogen is likely to cause embronynic death rather than malformation (all or nothing effect)
- 2-8 weeks after contraception – During organogenesis exposure to teratogens may cause malformation
- >8 weeks after contraception – slowly forming organs such as brain and kidney can be effected by teratogen exposure resulting in cognitive impairment, or behavioral effects
| Indications for genetic couselling |
| Parents with genetic disorders |
| Couples who have had a still birth |
| Couples who have had a child with birth defect or intellectual disability |
| Family history of known genetic disorders |
| Recurrent miscarriage |
| Advanced maternal age |
| Consaguinity |
| Exposure to radiation or drugs during pregnancy |
















Discussion