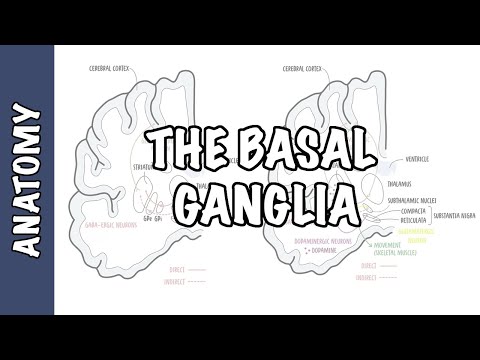
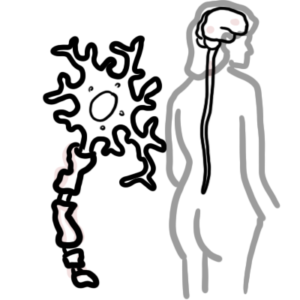
0:00 Hello. In this video, we're going to look at the pharmacology of Parkinson's, 0:08 so the 0:08 main drugs involved in the treatment of Parkinson's disease. If you haven't 0:13 watched my video 0:14 on Parkinson's pathophysiology, I recommend you watch that to get a better 0:19 understanding 0:20 of the disease. So hopefully that will make this video a lot easier. So 0:26 Parkinson's disease 0:27 is a neurodegenerative disease that affects an area of the brain known as a 0:32 substantia 0:32 nigra, mainly this area. And in the substantia nigra, you have important 0:40 neurons arising from 0:41 there known as a dopaminergic neurons. And these guys, they secrete dopamine, 0:45 which 0:45 is important in essentially contributing to a controlled movement pattern. So 0:51 let us 0:51 look at a normal neuron in this area and compare it to the one in Parkinson's 0:57 disease. 0:58 So let's look at the normal one first. So here we have a dopaminergic neuron. D 1:03 opaminergic 1:04 neurons contain dopamine vesicles in the terminal here. And these guys, they 1:11 are able to secrete 1:13 dopamine. And when they secrete dopamine, it will essentially either stimulate 1:21 or it 1:21 will inhibit these GABA-nergic neurons here. These GABA-nergic neurons are 1:28 found in an 1:29 area of the brain known as a coredate striatum. The coredate striatum is made 1:35 up of the coredate 1:36 nucleus and coredate putamen. Again, this area contains GABA-nergic neurons, 1:43 which receives 1:44 information from the dopaminergic neurons from the substantia nigra. So these 1:49 guys have 1:50 dopamine receptors. When dopamine is released, it binds onto these dopamine 1:57 receptors and 1:58 either stimulates or inhibits the GABA-nergic neurons. Within the dopaminergic 2:03 neurons 2:04 here, we have an enzyme monomer amine oxidase. And these guys essentially break 2:10 down the 2:11 dopamine after it's being used. So it sort of helps in the recycling process. 2:18 So Parkinson's 2:18 disease is where we have degeneration of dopaminergic neurons. This means that 2:24 we have not 2:26 much dopamine or no dopamine being produced by the cells in this area. Now, 2:34 these neurons 2:35 in the central nervous system in the substantia nigra, they're surrounded by -- 2:40 they're protected 2:42 by the blood-brain barrier, just an important side note. Okay, so again, in 2:48 Parkinson's 2:49 disease patient, we have decrease in dopamine in the synaptic cleft because no 2:53 dopamine 2:54 is being produced because the neurons are dying. Similarly, we have, again, the 3:03 enzyme, 3:03 of course, monomer amine oxidase, which will still break down the dopamine if 3:08 it were 3:08 being produced. So essentially, the treatment for Parkinson's disease is to 3:19 provide more 3:21 dopamine. That is one logical reason. So a drug that could be given is known as 3:28 levodopa. 3:30 So levodopa is a precursor to dopamine. And it's given because it is able to 3:38 pass the 3:39 blood-brain barrier. So it can go into the neuron, whereas dopamine cannot pass 3:47 the blood-brain 3:48 barrier. That is why we give levodopa. Unfortunately, in the peripheral system 3:54 or in just the blood 3:55 vessels, levodopa can be broken down by dopamine carboxylase to dopamine. And 4:04 so if 4:04 it gets converted to dopamine, before it reaches the brain, that's really not 4:10 helpful. 4:11 So usually, there's another drug which is given in combination with levodopa. 4:19 These 4:19 guys are known as decarboxylase inhibitors. Decarboxylase inhibitor, our main 4:24 example, 4:25 is carvidopa. And these guys, again, they prevent the peripheral breakdown of 4:29 levodopa 4:29 to dopamine, allowing levodopa to essentially move into the dopaminergic 4:34 neurons that are 4:35 left over to produce more dopamine. However, levodopa in the periphery can also 4:40 be broken 4:40 down to 3 OMD by comped. And so you also can administer a comped inhibitor. 4:46 Again, comped 4:47 inhibitors prevents the peripheral breakdown of levodopa. So levodopa is an 4:55 able to pass 4:56 the blood-brain barrier into the dopaminergic neurons. In the neurons, levodopa 5:01 can be converted 5:02 to dopamine by carboxylase. And so this neuron is able to produce and release 5:08 more dopamine, 5:10 lessening the signs and symptoms of Parkinson's disease. So those were these 5:18 drugs, the levodopa 5:19 is first-line for Parkinson's disease. However, there's other drugs that could 5:25 also be given. 5:26 And they target different things. So for example, you can actually have 5:31 dopamine agonists. And 5:32 these guys essentially bind and activate dopamine receptors. So they mimic the 5:36 effects of dopamine. 5:39 You can also administer mono amine oxidase inhibitors. So these guys inhibit 5:45 the enzyme 5:45 within the neuron that would otherwise break down dopamine. So they prevent 5:51 these guys 5:51 prevents the breakdown of dopamine, allowing more dopamine to be used for 5:56 longer periods 5:57 of time. So I hope that made sense. Again, the drugs used, main drugs used are 6:03 levodopa, 6:04 which has to be administered with the peripheral dopamine carboxylase 6:08 inhibitors such as carbidopa. 6:10 And then you can also have the dopamine agonists or the mono amine oxidase 6:14 inhibitors. 6:16 I hope you enjoyed this video on the pharmacology of Parkinson's disease. It 6:19 was just an overview. 6:20 Thank you very much for watching. Bye.