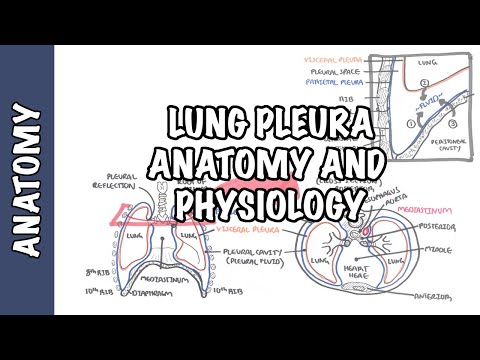
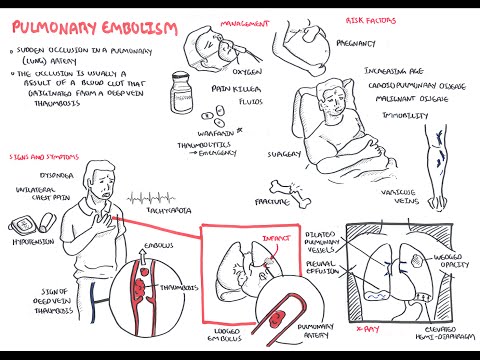
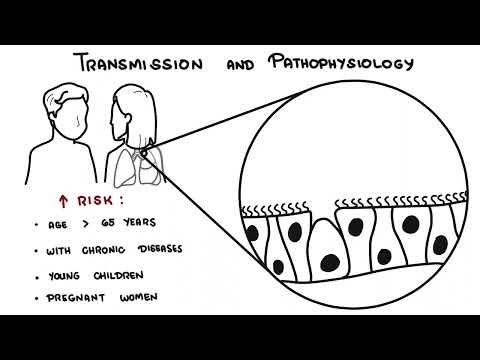
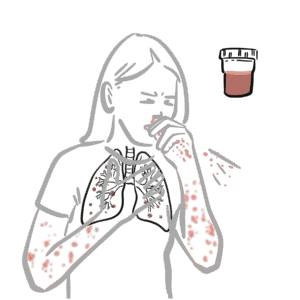
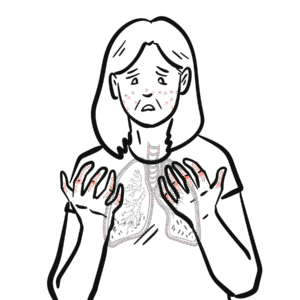
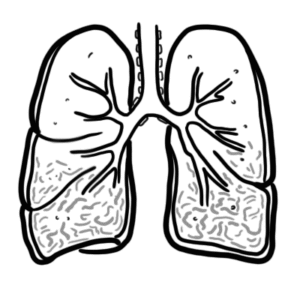
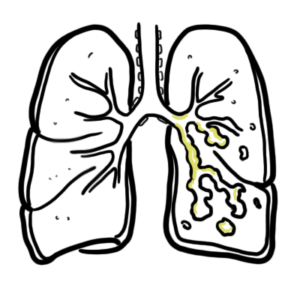
0:00 Hello, in this video, we're going to talk about plural effusions. 0:09 Plural effusions is where you have accumulation of fluid in the plural space. 0:13 Let's recap some basic anatomy and physiology. 0:16 So here are the lungs. 0:18 Surrounding the lungs is the visceral pleura, which continues on and becomes 0:23 the parietal 0:24 pleura, which attaches to the thoracic wall. 0:27 The visceral and parietal pleura is a continuous, serious sheet. 0:32 The space that separates them is the pleural space, which contains pleural 0:39 fluid. 0:39 Let's take a closer look. 0:41 Here is the parietal pleura layer, and attached to the lung is the visceral ple 0:48 ura layer. 0:49 In between is the pleural space, where we find pleural fluid. 0:53 The visceral space is really the lungs, which contains the pulmonary capill 0:57 aries and the 0:58 alveoli. 1:02 The parietal space is a thoracic wall, where we find the systemic capillaries. 1:08 In the parietal space, you also find lymph vessels, which drain the pleural 1:14 fluid from the pleural 1:15 space. 1:16 The pleural fluid comes from three main sources. 1:19 The main source being the systemic capillaries, then you also have fluid that 1:24 can enter from 1:24 the pulmonary capillaries and also from the abdomen, where fluid can come in 1:29 through small 1:30 tiny holes in the diaphragm. 1:32 Again, the lymphatics drain this pleural fluid and helps maintain the normal 1:39 pressure in the 1:40 pleural space. 1:44 So pleural effusions is essentially where you have accumulation of pleural 1:48 fluid in the 1:48 pleural space. 1:50 When this happens, you really get restriction of lung expansion, and so you get 1:55 shortness 1:55 of breath. 1:56 There are two main mechanisms for developing pleural effusions. 2:01 The first is where you have too much pleural fluid forming in the pleural space 2:05 . 2:06 And the second mechanism is where you have decreased in pleural fluid clearance 2:10 from the 2:11 pleural space. 2:13 Let's take a look at some examples of the first mechanism, where you have an 2:17 increase 2:17 in pleural fluid formation. 2:21 Let's zoom into the right lung here, where we find a pleural effusion. 2:25 Here again, you can have your pulmonary capillaries, part of your visceral 2:29 space. 2:30 And here are your systemic capillaries, which are part of your parietal space. 2:36 Imagine in either the pulmonary or systemic capillaries, you have inflammation. 2:41 This will trigger the vessel cells to contract, causing an increase in vascular 2:46 permeability. 2:47 When there is an increase in vascular permeability, fluid and proteins will 2:52 leak from the vessels 2:53 into the pleural space, which increases fluid formation essentially in the ple 2:59 ural space, 3:00 and so leads to pleural effusions. 3:04 The capillaries leaving the pleural membrane will return to the hot eventually 3:09 via the veins. 3:11 If there is an increase in venous pressure, such as left-sided or right-sided 3:18 hot failure, 3:19 this can lead to pleural effusion, because blood cannot travel back to the hot 3:27 efficiently. 3:29 Another cause of pleural fluid formation can be if there is a decrease in 3:33 plasma oncotic 3:34 pressure, which for example means when you have low amounts of protein in the 3:40 blood. 3:41 Because there is no proteins or not enough proteins in plasma, this means fluid 3:45 cannot 3:46 be kept within the vessels, and so it will leak out into the interstitial space 3:52 . 3:53 Another cause of increase in pleural fluid formation is if you have a decrease 3:57 in pleural 3:57 pressure, such as in lung collapse or atelectasis. 4:02 These are some examples of things that can cause an increase in pleural fluid 4:06 formation. 4:06 Note that in some of these examples, proteins also move into the pleural space, 4:12 causing an 4:13 increase in protein levels in the pleural fluid. 4:17 Plural fluid protein levels are not altered by clearance of fluid by the lymph 4:24 atics. 4:25 This is very important as protein levels in pleural fluid helps differentiate 4:30 between 4:30 two types of pleural effusions. 4:32 Anyway, we'll talk about this later. 4:36 The second mechanism of developing pleural effusion is when there is a decrease 4:40 in pleural 4:40 fluid clearance, which we sort of touched on, the lymphatics. 4:45 Let's now take a look at some examples that cause a decrease in pleural fluid 4:50 clearance. 4:51 Remember, fluid is cleared from the pleural space by the lymphatic system. 4:56 If you have a blockage of the lymphatic stoma, this means less fluid drains 5:01 leading to pleural 5:02 fusion, if there is an obstruction, compression obstructing the lymphatic 5:06 drainage, this means 5:08 fluid cannot be drained. 5:10 An example is if you have a granuloma in the lung, for example, compressing 5:13 against the 5:14 lymphatics. 5:16 Another example is if there is an increase in venous pressure. 5:20 Because if you think about it, the lymph vessels eventually will drain into the 5:23 venous system. 5:24 So if there is a buildup of pressure in the veins, this means buildup of 5:28 pressure in the 5:28 lymphatics, and so the lymphatic system cannot drain adequately. 5:35 Cancer invasion can block and disrupt fluid drainage, leading to pleural eff 5:40 usions. 5:40 Chemotherapy and radiation can also damage the lymph vessels. 5:44 Finally, if there is limitation of respiratory motions, this decreases the 5:50 draining rate. 5:51 Because as we know, the lymphatics and vessels also rely on contraction of 5:56 muscles to support 5:57 the movement. 5:58 Again, the two main mechanisms of pleural effusion are increase in fluid 6:02 formation and decrease 6:04 in fluid clearance. 6:05 And we learned a few examples of each. 6:07 However, it's very important to know that pleural effusions don't occur from a 6:11 single 6:11 factor we talked about. 6:13 Usually multiple factors contribute to pleural effusions. 6:18 Pleural effusions usually present with an underlying disease such as pneumonia. 6:23 The clinical findings of pleural effusion specifically include shortness of 6:27 breath because the fluid 6:28 prevents proper ventilation and lung expansion. 6:33 If you percuss the lung bases, they will be dull. 6:37 There will be also decreased chest wall movement on the affected side because 6:41 the fluid restricts 6:43 the movement here. 6:45 On our scultation there will be decreased breath sounds around where the fluid 6:53 is. 6:54 Investigations to order include a chest x-ray and on the x-ray you will find bl 6:58 unting of 6:59 the cost of phrenic and cardiophrenic angles which signifies effusion. 7:05 Here is a chest x-ray of someone sitting down. 7:08 You can see straight away that there is a large pleural fusion on the left hand 7:12 side. 7:12 There's blunting of the costo and cardiophrenic angles and there's also the min 7:17 iscule sign, 7:18 the darker pink on the top. 7:20 Here again is another chest x-ray and again you can see the classic miniscule 7:26 sign. 7:27 Here's a less subtle one, a bilateral pleural effusion. 7:30 You can see blunting of the costo and cardiophrenic angles bilaterally and also 7:34 the miniscule 7:35 sign just. 7:38 If someone prevents with suspected pleural fusion of unknown cores initially, 7:43 blood tests such 7:44 as full blood count, EUC and LFTs can be helpful. 7:50 The diagnosis of pleural fusion, gold standard would be an ultrasound and 7:54 looking for the 7:55 specific cause of the pleural fusion, thoracosentesis is warranted. 8:01 Thoracosentesis is where they stick a needle in between the ribs with guidance 8:06 of the ultrasound 8:07 and then fluid is drawn up for fluid analysis. 8:13 Thoracosentesis is both diagnostic and therapeutic. 8:17 Thoracosentesis gets you a pleural fluid sample which can be then analyzed. 8:21 Initially you would order lactate dehydrogenase and protein levels here. 8:26 This will help differentiate the two main types of pleural fusions or the two 8:30 categories 8:30 of pleural fusions which are transudative pleural fusion and exudative pleural 8:36 fusions. 8:36 This is where we bring in what's called lights criteria and lights criteria 8:41 will essentially 8:41 tell you if the pleural fusion is from an exudative cause or a transudative 8:48 cause. 8:48 Exudative requires one of the following where you have pleural fluid protein to 8:55 serum protein 8:56 ratio greater than 0.5 which really means that it will be exudate if there is 9:03 more protein 9:04 in the pleural fluid. 9:08 The second is where you have a pleural fluid lactate dehydrogenase to serum 9:12 lactate dehydrogenase 9:14 ratio greater than 0.6 which really means it's exudate if the pleural LDH level 9:20 is higher. 9:23 Or finally it is an exudative pleural fusion if the pleural fluid LDH is 9:28 greater than two-thirds 9:30 the upper limit of the laboratory normal value of serum LDH. 9:34 Unfortunately the lights criteria misidentifies 25% of transudative effusions 9:40 as exudative 9:41 infusions. 9:43 Now if transudative effusions is suspected based on clinical presentation or 9:49 laboratory 9:49 findings other things can be analyzed within the pleural fluid such as your 9:54 brain naturally 9:55 peptide which if very elevated signifies heart failure. 10:02 Causes of transudative pleural fusion include congestive height failure with 10:06 elevated brain 10:07 naturally peptide, liver cirrhosis and nephrotic syndrome and superior vena c 10:14 ava obstruction. 10:16 Exudative pleural fusions really means that there is a lot of LDH and/or a lot 10:20 of proteins 10:21 in the pleural fluid in comparison to the serum levels. 10:25 If exudative pleural fusion is suspected and you want to diagnose a potential 10:30 cause of 10:30 exudative pleural fusions other tests you can order here include pleural fluid 10:37 microscopy 10:37 culture sensitivity, pleural fluid cell differentiation and pleural fluid 10:43 glucose levels. 10:44 These tests can help identify potential causes of the exudative pleural fusions 10:50 . 10:50 Some of the more common causes of exudative pleural fusions include infections, 10:55 malignancy, 10:56 pulmonary embolism, gastro intestinal pathology such as pancreatitis and 11:01 connective tissue 11:02 diseases. 11:05 Now the management of pleural fusions briefly obviously you can treat the 11:11 underlying cause. 11:12 Thorocosentesis is helpful to identify the potential cause but also can be 11:18 therapeutic. 11:19 If the effusion is large enough the definitive treatment is a chest strain 11:23 where a tube is 11:24 inserted into the pleural space to drain the fluid out. 11:28 You can see on this x-ray on the left hand side you have a pleural effusion and 11:33 a tube 11:33 inserted in a safe triangle which will drain the fluid out. 11:40 Pleural thesis can also be used if pleural fluid continues to build up within 11:44 the pleural 11:45 space despite the chest strain being used. 11:48 Pleural thesis is used in conditions such as cancer where fluid is continuously 11:55 formed. 11:56 Pleural thesis is a procedure where ductus cyclin or talcum powder are put in 12:03 within 12:04 the pleural space to obliterate the pleural space to prevent recurrent pleural 12:09 effusions 12:10 or even pneumothorax. 12:13 Pleural effusion is a surgical option which removes the pleural altogether. 12:19 Let's now look at some different causes of pleural effusions specifically in 12:23 more detail 12:24 beginning with transudative pleural effusions, first looking at heart failure. 12:31 So normally the pulmonary arteries pumps blood to the lunges where it will 12:35 return to the 12:35 left side of the heart. 12:37 Imagine you have left ventricular failure, main cause of heart failure. 12:42 This causes fluid to go backwards to the pulmonary vein, pulmonary capillaries. 12:46 When fluid goes backwards it will result in pleural effusions bilaterally. 12:55 Let's take a closer look at how this happens. 12:57 Here are the pulmonary capillaries, the pulmonary interstitium and the pleural 13:01 space. 13:02 If there is left ventricular failure pressure builds up here and blood can pull 13:06 in the pulmonary 13:06 capillaries, this results in fluid moving into the pulmonary interstitium 13:10 initially causing 13:11 pulmonary edema, then fluid can shift to the pleural space causing pleural eff 13:18 usions. 13:18 Usually the lymphatics can help maintain equilibrium, but with so much pleural 13:23 fluid being produced 13:24 there is less lymphatic drainage causing pleural effusions. 13:29 Again here the pleural fluid typically has raised brain-naturary peptides BNP 13:34 which is 13:34 a marker for ventricular strain. 13:37 Other causes of transudative pleural effusions we talked about was liver cirrh 13:40 osis and nephrotic 13:41 syndrome. 13:42 There are many factors which lead to pleural fluid in these examples, but the 13:46 main one 13:46 would be low protein levels in the blood. 13:49 In liver cirrhosis there is a decreased protein production such as albumin, the 13:53 main protein 13:54 that circulates in our blood. 13:56 In nephrotic syndrome there is an increase in protein loss, there is an 14:00 increase in albumin 14:00 loss through urine. 14:03 Both liver cirrhosis and nephrotic syndrome means that there is low protein 14:06 levels in 14:07 the blood, hypo protonemia or hypo albumenemia. 14:12 This means that there will be a decrease in oncotic pressure in the vessels due 14:16 to the 14:16 low protein levels, which means that the vessels can't hold the water within 14:21 the vessels. 14:22 And so water will shift into the pleural space as a result causing pleural eff 14:31 usions. 14:33 The pleural effusions are the pleural effusions with high LDH and/or high 14:37 protein levels 14:38 in the pleural fluid compared to serum. 14:42 Examples include malignancy. 14:50 Malignancy can cause effusions in many ways. 14:57 It can obstruct the storm of the lymph vessels, it can compress the lymph 15:01 vessels itself, 75% 15:03 of malignant infusions are from lung, breast and ovarian cancer. 15:10 Finally, pulmonary embolism is a cause of pleural effusions, exudative pleural 15:16 effusions, 15:18 and probably an unrecognized one. 15:21 Polyembolisms occurs when there is a thrombus which occludes a pulmonary artery 15:27 or pulmonary 15:28 capillary here as shown. 15:31 When this happens, the pulmonary vessels will compensate in a few ways. 15:36 One way is that it will cause shunting of blood flow to capillaries which work, 15:40 which 15:40 means more blood flow, which means more fluid can enter the pleural space. 15:46 There will be an increase in vascular permeability there, and fluid will shift 15:52 into the pleural 15:53 space.