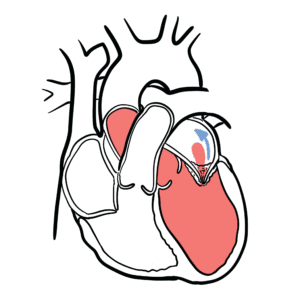
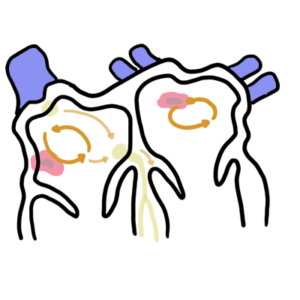
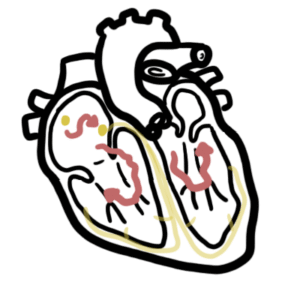
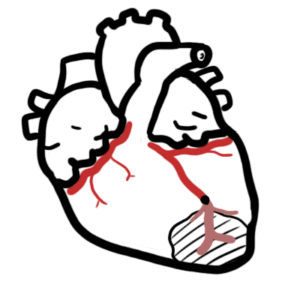
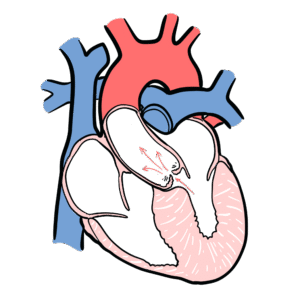
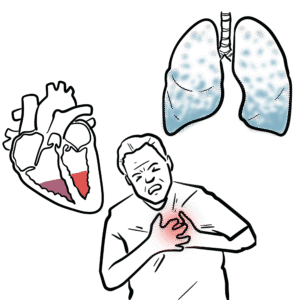
0:00 Superventricular tachycardia is an arrhythmia, which occurs above the ventric 0:11 les. 0:11 Examples of superventricular tachycardia include atrial tachycardia, atrial f 0:16 ibrillation, atrial 0:18 flutter, atrial ventricular reentry tachycardia (AVRT) and atrial ventricular 0:24 nodal reentry 0:25 tachycardia, or AVNRT. AVNRT is the classic superventricular tachycardia, and 0:34 is a result 0:35 of abnormal, unsynchronized electrical transmission from the atrial ventricular 0:41 node to the ventricles. 0:44 The sinoatrial node is a dominant pacemaker cell in the heart, which sends 0:48 impulses to 0:49 the atrium causing atrial contraction. From there, the impulse arrives at the 0:56 AV node. 0:57 The AV node conducts the impulse slower before entering the bundle of hiss, 1:02 bundle branches 1:03 and purkinji fibers, where the impulse travels rapidly, resulting in vent 1:11 ricular contraction. 1:13 Atrial ventricular nodal reentry tachycardia, as the name suggests, is tachyarh 1:17 ythmia caused 1:18 by a reentry circuit in the atrial ventricular node, the AV node. In AVNRT, 1:26 there are two 1:28 atrial ventricular nodal pathways. Patients can have two atrial ventricular nod 1:33 al pathway 1:34 and be fine. However, some people have a slow and fast conducting atrial vent 1:40 ricular 1:41 nodal pathway. A fast conducting pathway has rapid conduction, but a slow ref 1:48 ractory period, 1:50 whereas a slow conducting pathway has a rapid refractory period coupled with 1:59 slow conduction. 2:02 The differences in the slow and fast conducting pathways can trigger AVNRT, the 2:07 atrial ventricular 2:08 nodal reentry tachycardia, and there are two main types of AVNRT. The slow, 2:15 fast AVNRT 2:16 accounts for 90% of AVNRTs. Impulse travels slow along the slow pathway and 2:24 fast along 2:24 the fast pathway. The impulse traveling down the fast pathway will eventually 2:30 excite cells 2:31 at the bundle of hiss, but also in the slow pathway as well. The fast impulse 2:36 will thus 2:37 cancel out the slow impulse in the process. The next impulse that travels from 2:44 the syno-atrial 2:45 node will enter the slow pathway first, because the refractory period here is 2:50 fast and the 2:51 cells are able to get excited again. Because of this, the impulse traveling 2:56 down the slow 2:57 pathway may eventually re-excite fibers along the fast pathway and the bundle 3:04 of hiss. 3:05 The impulse will travel rapidly backwards along the fast pathway retrograde to 3:13 the atrium 3:14 and also re-enter the slow pathway again, causing a re-entry circuit that will 3:20 continue 3:21 and continue, causing simultaneous ventricular and atrial contractions. 3:29 In slow, fast AVNRT, there is anterograde conduction by the slow atrial vent 3:37 ricular 3:38 nodal pathway and retrograde conduction by the fast atrial ventricular nodal 3:48 pathway. 3:49 Then there is also fast, slow AVNRT, which represents approximately 5 to 10% of 3:57 the 3:58 AVNRTs. 4:07 Here, there is anterograde conduction by the fast atrial ventricular nodal 4:16 pathway and 4:18 retrograde conduction by the slow atrial ventricular nodal pathway. 4:26 Up the fast pathway is very rapid, that retrograde atrial depolarization, which 4:32 is represented 4:33 by the P-wave in the ECG, is simultaneous or almost simultaneous with the anter 4:39 ograde 4:40 ventricular activation, represented by the QRS on ECG here. 4:47 This causes the low amplitude P-wave to be obscured in the much higher 4:54 amplitude QRS complex. 4:56 The ECG findings are no visible P-waves. 5:00 If there are visible P-waves, the PR interval is shortened. 5:04 A narrow QRX complex with high amplitude, tachycardia, a rate of about 150, but 5:11 it could 5:12 range from 120 to 220 beats per minute. 5:21 AVNRT usually affects young people. 5:22 A young female, for example, will present with palpitations. 5:27 Palpitations is almost always reported. 5:31 They can be diaphoretic. 5:32 Patients uncommonly are hemodynamically unstable. 5:38 People often have a feeling of diuresis, which is due to elevated atrial 5:41 pressure and release 5:42 of ANP, which is a hormone that promotes peeing of sodium and water. 5:50 Neck pulsations occur secondary to simultaneous contraction of the atria and 5:55 ventricles against 5:56 the closed mitral and tricuspid valve, and this is called Bruegada phenomenon. 6:04 In terms of management, in an acute setting, anyone who has tachycardia, a very 6:09 fast heart 6:10 rate and is unstable, will require cardioversion. 6:15 As cardioversion picks up the QRS complex and delivers a shock. 6:21 If not synchronized, it can create a ventricular tachycardia. 6:26 Cardioversion is followed by a 24-hour infusion of amiodarone. 6:31 The supraventricular tachycardia will revert back to sinus rhythm. 6:37 In patients who are stable without hemodynamic compromise, patients can undergo 6:42 a vagal maneuver. 6:44 All maneuvers include valsaba maneuver, which can be done, for example, by 6:48 asking someone 6:48 to blow into a syringe. 6:52 If vagal maneuvers does not work, adenosine can be given. 6:56 Adenosine temporarily stops the conduction in the atria ventricular node, 7:00 thereby potentially 7:02 terminating the re-entry circuits in the atria ventricular node. 7:07 If AVNRT becomes recurrent, or does not terminate, radiofrequency delivered via 7:14 catheter ablation 7:15 can be directed at either the fast or slow pathway. 7:19 Ablation of the slow pathway is preferred to lower risk of complete heartblock. 7:24 Thank you for watching, I hope you enjoyed this video.