COPD
The diagnosis of COPD is usually limited to individuals who have chronic airflow obstruction associated with tobacco smoke or some other noxious inhalant, and it is usually not difficult to distinguish it from other causes of chronic airflow obstruction. The most commonly associated clinical disorders associated with COPD are emphysema and chronic bronchitis.
Chronic Obstructive Lung Disease: A serious, progressive and disabling condition that limits airflow in the lungs. It includes emphysema and chronic bronchitis. Strongly associated with smoking
Interstitial Lung Disease: Includes a diverse group of respiratory conditions characterised by inflammation and fibrosis of the interstitium. Worsening hypoxia and respiratory failure may develop with disease progression. The disease is considered a restrictive lung disease
Restrictive Lung Disease: Unable to fully fill the lungs with air. Their lungs are restricted from fully expanding.
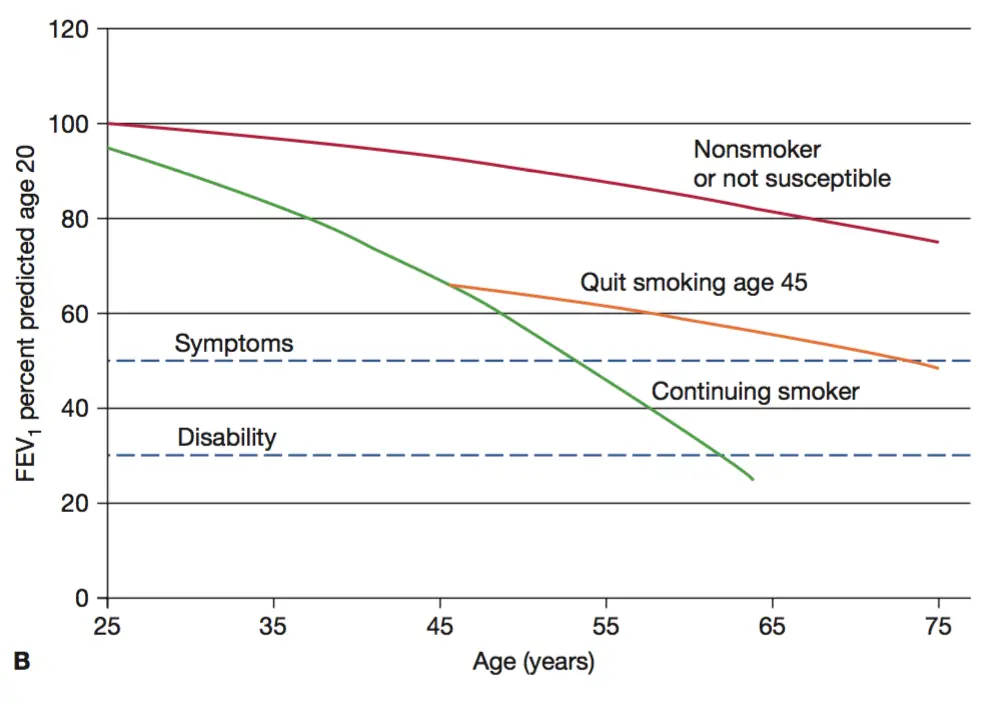
COPD results from an increase in the rate of decline in lung function over time.
Cardinal Triad of COPD: (exertional) Dyspnoea, Chronic cough and sputum production.
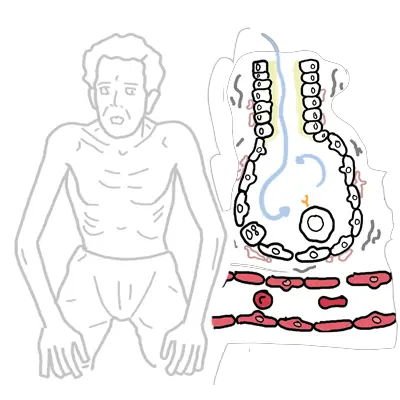
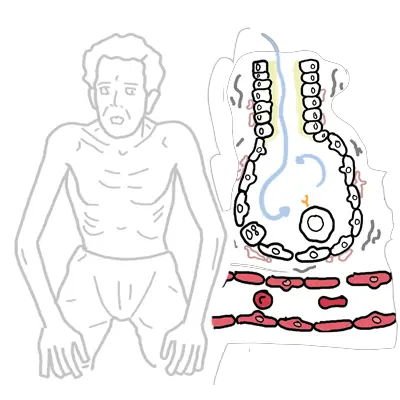
Clinical Examination – Pure emphysema (pink puffers)
Clinical Examination – Pure chronic bronchitis (blue bloaters)
| COMMON CAUSES OF CHRONIC COUGH |
| COPD |
| Asthma |
| GORD |
| Post nasal drip |
| COMMON CAUSES OF CHRONIC DYSPNOEA | |
| Respiratory Disease | Cardiovascular Disease |
| COPD | Myocardial Dysfunction (Heart Failure) |
| Asthma | Obesity/de-conditioning |
| Interstitial lung disease | |
| Emphysema | Chronic Bronchitis |
| Defined Pathologically Dilation and destruction of air spaces distal to the terminal bronchiole without obvious fibrosis. Decreased elastic recoil of alveoli causing decreased expiratory driving pressure, airway collapse and air trapping. | Defined Clinically Productive cough on most days for at least 3 consecutive months in 2 successive years. Obstruction is due to narrowing of the airway lumen by mucosal thickening and excess mucus |
| COPD Severity is based on FEV1 (COPD is diagnosed by FEV1/FVC) |
| Mild FEV1 <.7 |
| Moderate FEV1 0.5-0.3 |
| Severe FEV1 <0.3 |
| MRC Dyspnea score | |
| 1 | Not troubled by breathlessness except on streous exercise |
| 2 | Dyspnea when hurrying or walking up a slight hill |
| 3 | Walks slower than contemprorores on level ground due to dyspnea, or has to stop for breath when talking at own pace |
| 4 | Stops for breath after walking 100m or less on ground level |
| 5 | Too breathlesss to leave house, or when getting dressed |
Smoking cessation and supplemental oxygen to treat chronic hypoxemia are the only medical therapies shown to decrease mortality among persons with chronic obstructive pulmonary disease.
to step down therapy to lowest doses which control symptoms.
What are the 5 “A’s” of smoking cessation counseling?Ask about tobacco useAdvise to quitAssess willingness to attempt quittingAssist in attempt to quit (e.g., pharmacotherapy such as nicotine gum or patch)Arrange follow-up.
Emergency (acute exacerbations) sustained (>24-48 h) worsening of dyspnea, cough, or sputum production leading to an increased use of medications
Overview α1-antitrypsin deficiency
| Conditions suggesting a1- Antitrypsin Deficiency |
| Early onset |
| Non-smoker |
| Emphysema predominantly in lung bases (paracinar) |
| Necrotising panniculiitis |
| Family history |
| Bronchiectasis without other etiology |
The hallmark of restrictive lung disease is decreased lung capacities, particularly the TLC but also the vital capacity.
In both obstructive and restrictive lung disease, the FEV1 is decreased, the FEV1 /FVC is decreased in obstructive processes and normal in restrictive processes.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion