Overview
Felty syndrome is a rare but serious extra-articular manifestation of long-standing, seropositive rheumatoid arthritis (RA), characterized by the classic triad of RA, splenomegaly, and neutropenia. It was first described in 1924 by the US-American physician Augustus Roi Felty. It most commonly occurs after at least 10 years of poorly controlled RA and is associated with severe joint damage and extra-articular features. It predominantly affects middle-aged Caucasian women and may signal more aggressive disease. Occurs in <1% of patients with RA.
Definition
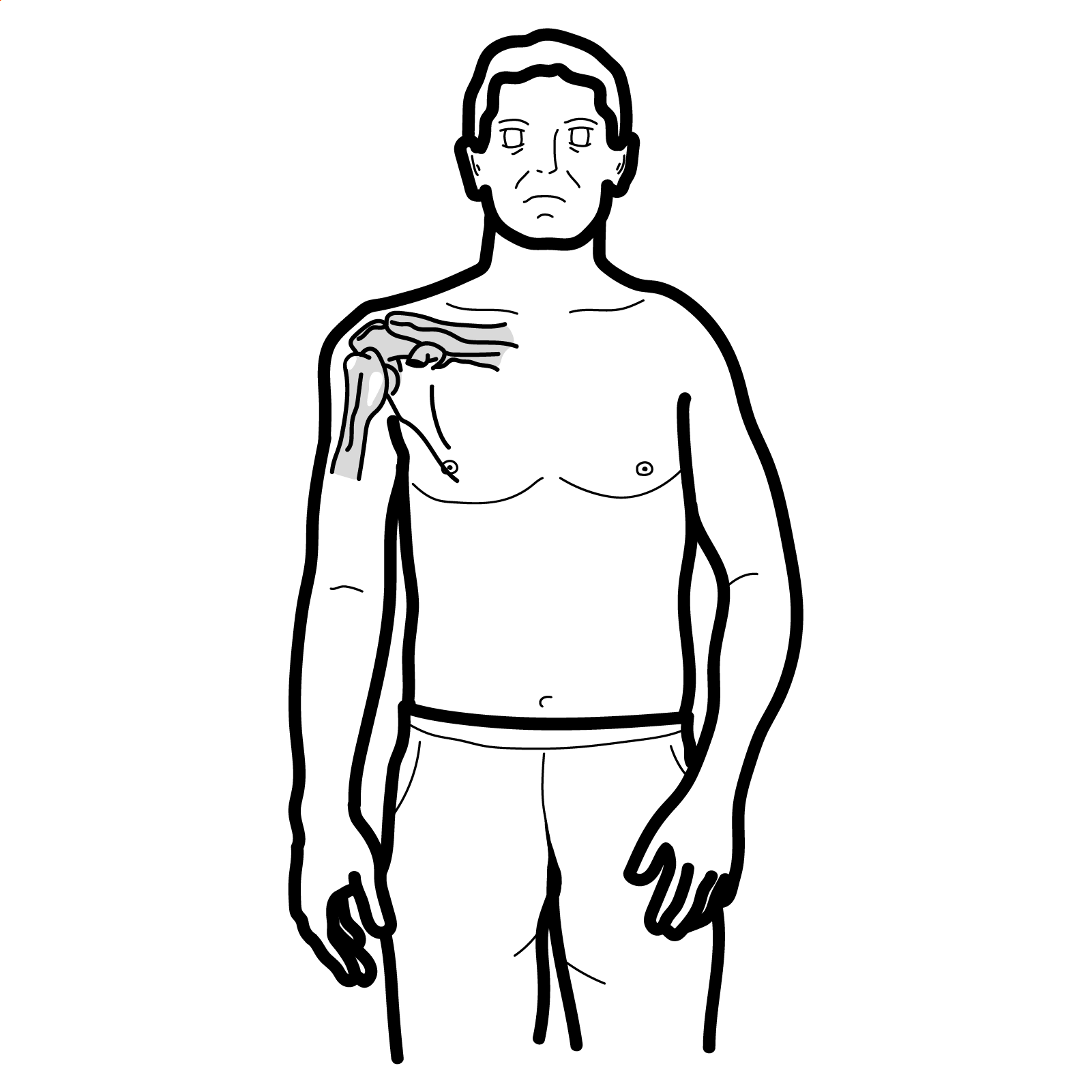
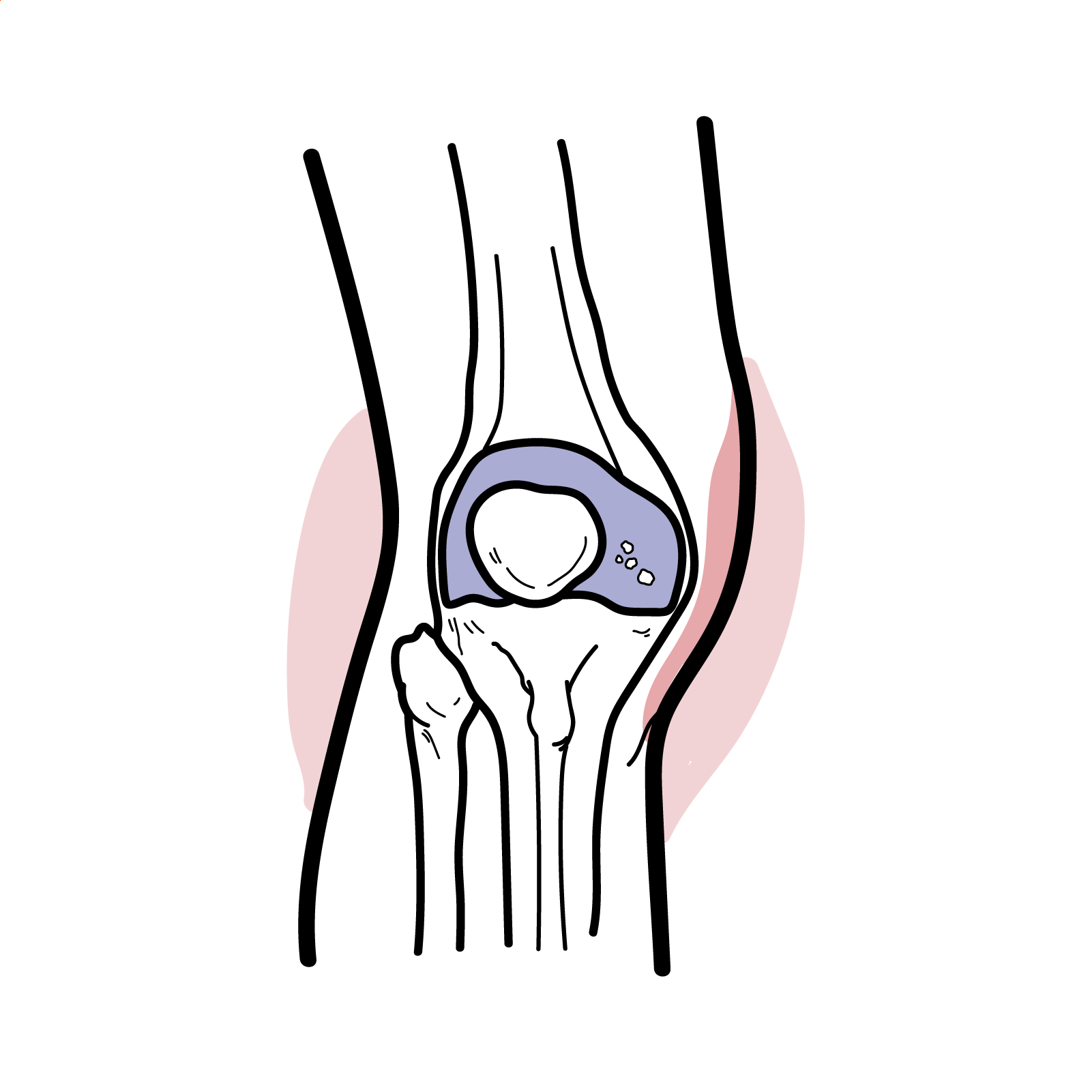
Rheumatoid arthritis: A chronic autoimmune inflammatory polyarthritis primarily affecting synovial joints, with systemic manifestations.
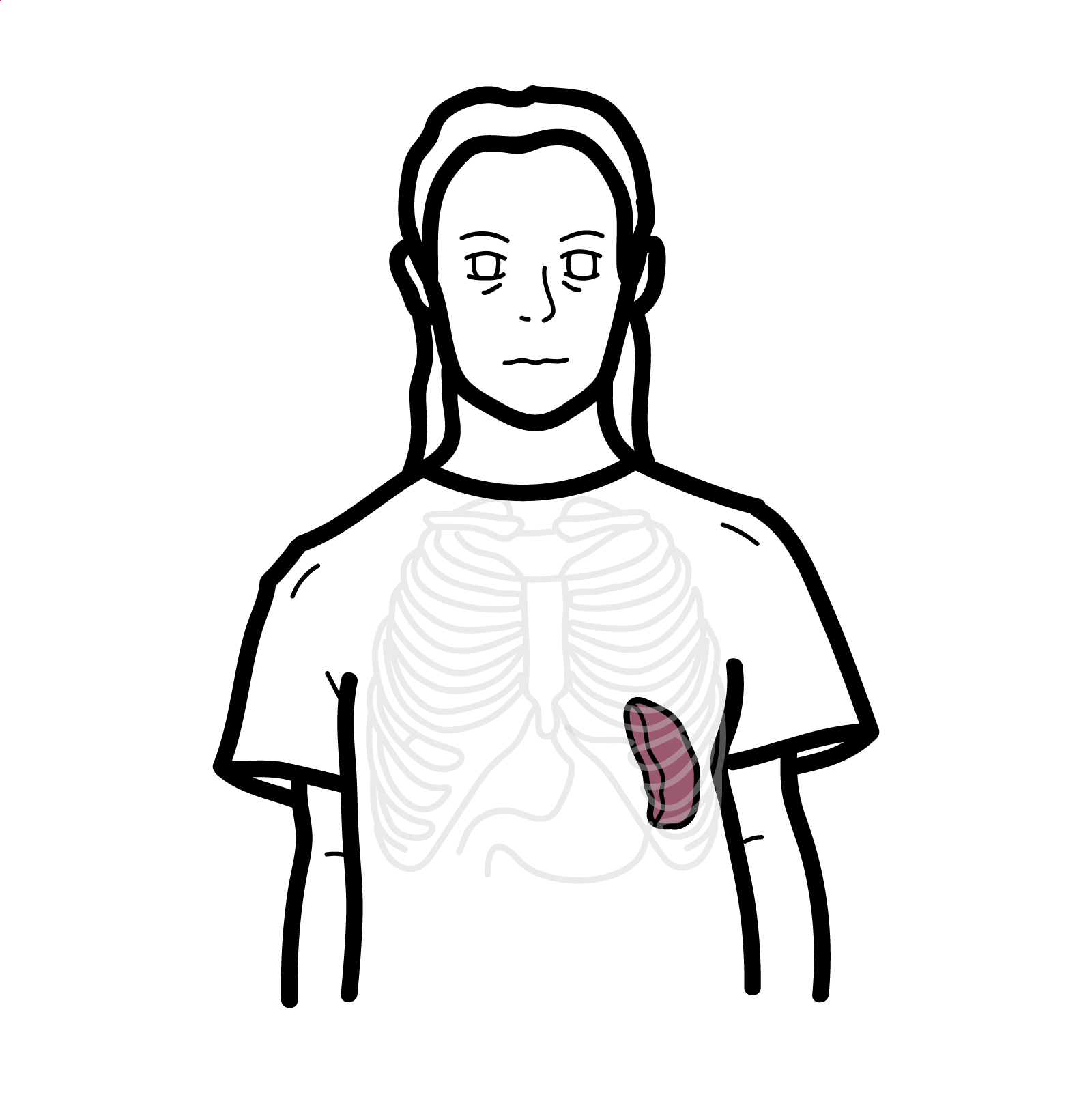
Splenomegaly: Enlargement of the spleen, commonly due to hyperplasia of lymphoid tissue or congestion.
Neutropenia: An absolute neutrophil count (ANC) <1500/μL, increasing the risk of infection.
Extra-articular RA: Manifestations of RA affecting organs outside the joints, including skin, lungs, and bone marrow.
Anatomy and Physiology
- Spleen plays a role in immune surveillance and removal of aged/damaged blood cells; in Felty syndrome, it is enlarged due to lymphoid hyperplasia
- Bone marrow and peripheral blood are critical in leukopoiesis and immune regulation; altered in Felty due to neutropenia and altered immune activity
Aetiology and Risk Factors
Aetiology
• Autoimmune process driven by chronic RA
• T-cell mediated destruction or peripheral sequestration of neutrophils
• Immune complex deposition in spleen
Risk Factors
• Long-standing RA (>10 years)
• Seropositive RA (RF and anti-CCP positive)
• Caucasian ethnicity
• Female sex (F:M ratio ~3:1)
• Presence of HLA-DR4 allele
Remember
>90% of patients with Felty syndrome are rheumatoid factor (RF) positive【1】.
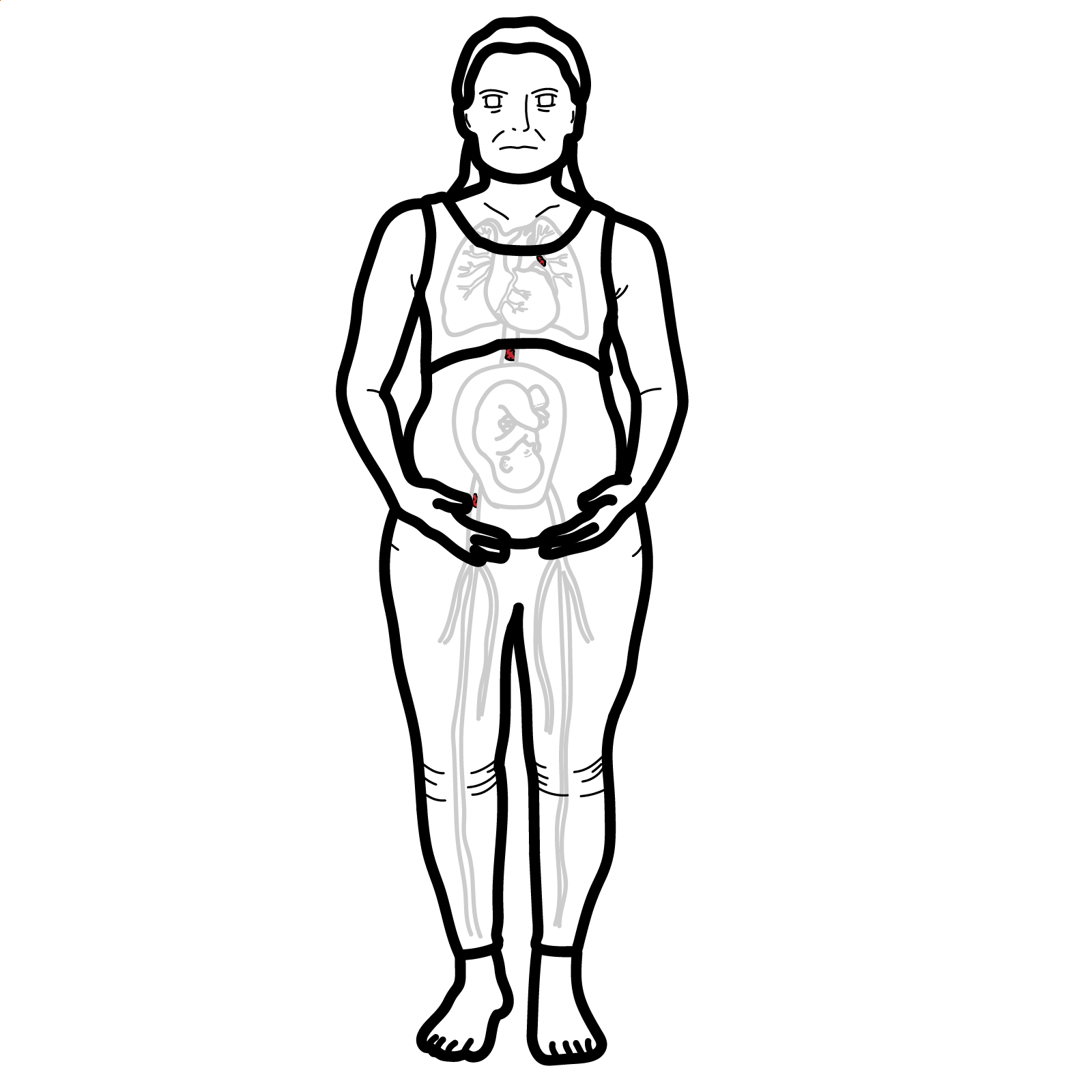
Pathophysiology
- Chronic RA leads to systemic inflammation and immune dysregulation
- Development of splenomegaly due to hyperplasia of lymphoid follicles and immune cell accumulation
- Neutropenia arises from splenic sequestration and immune-mediated destruction of neutrophils
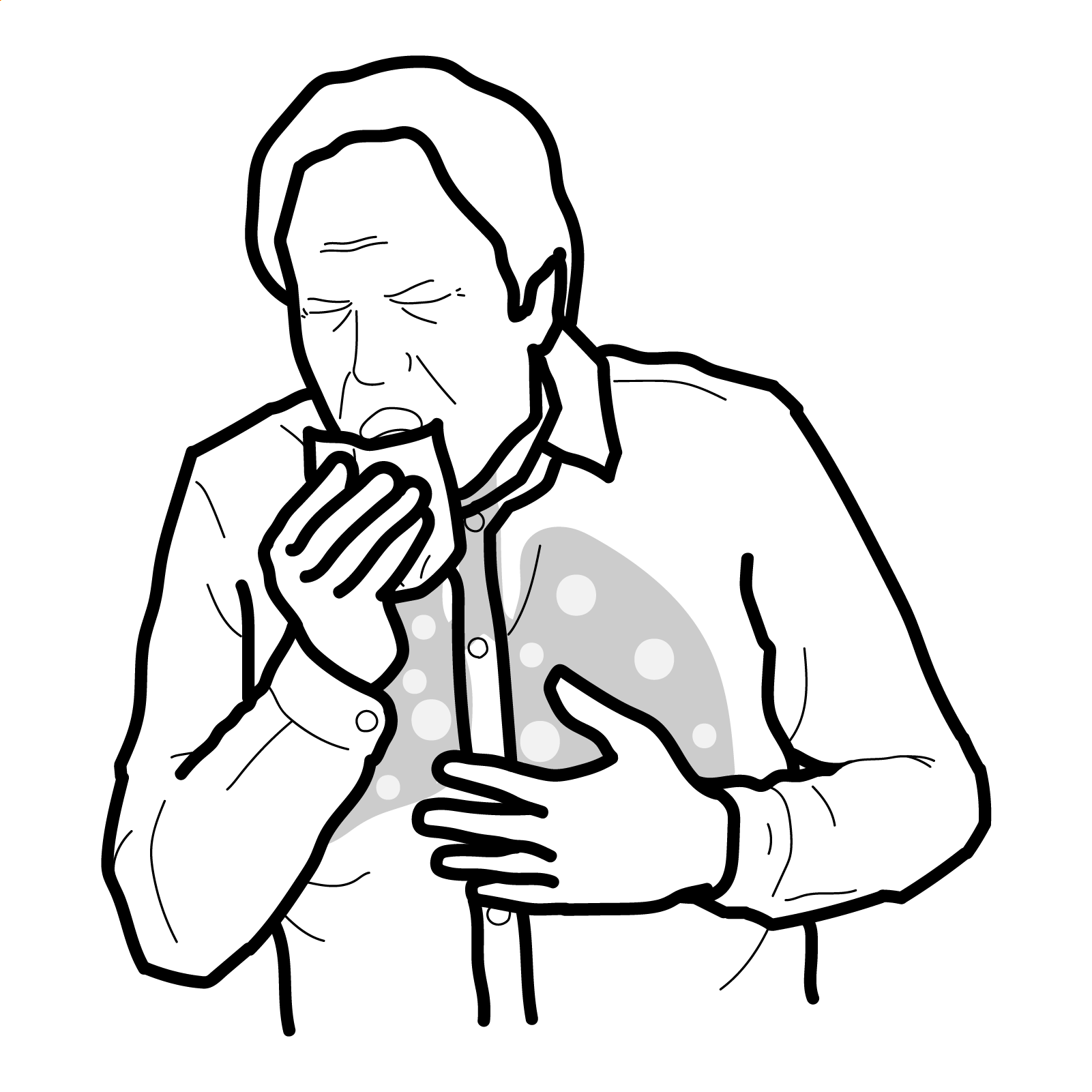
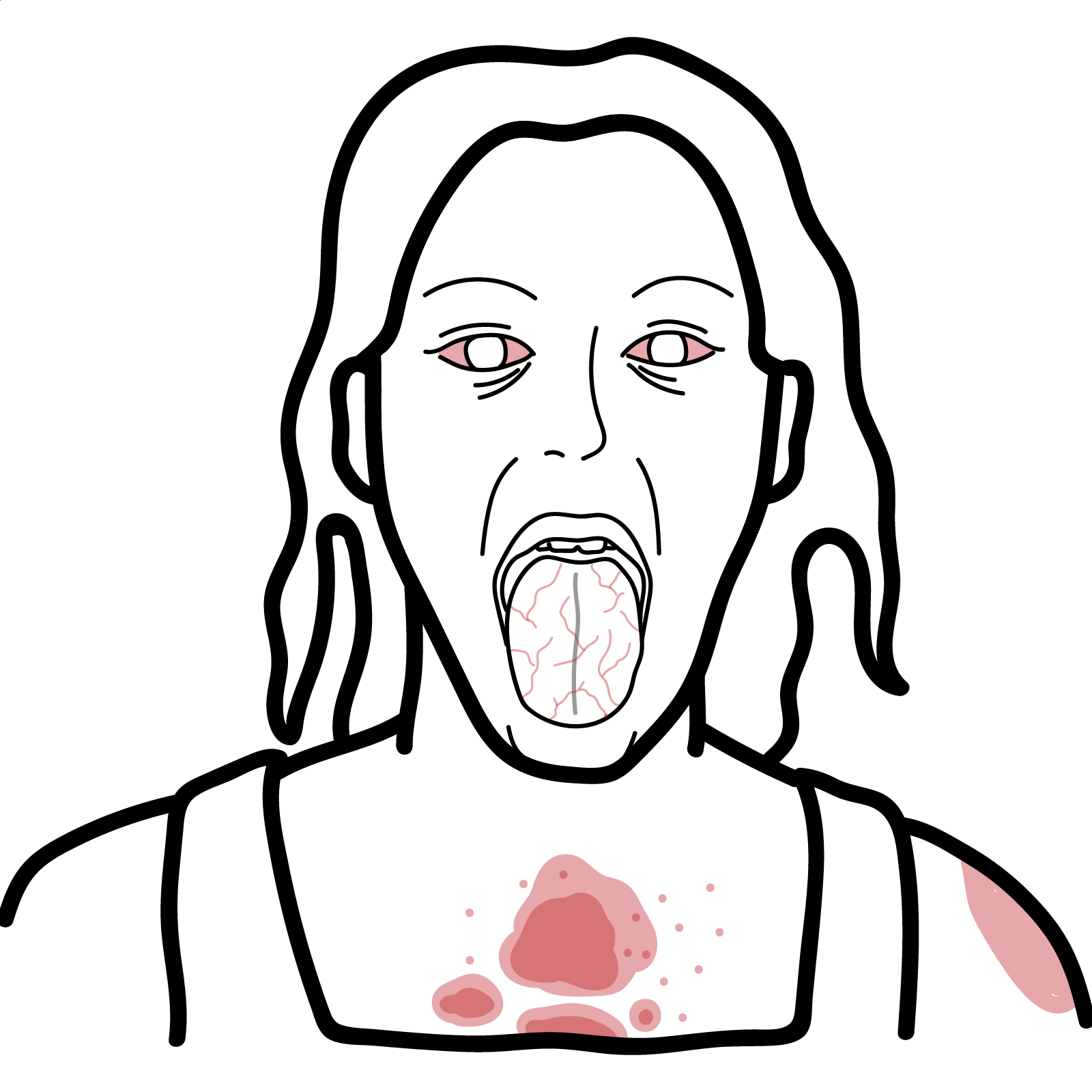
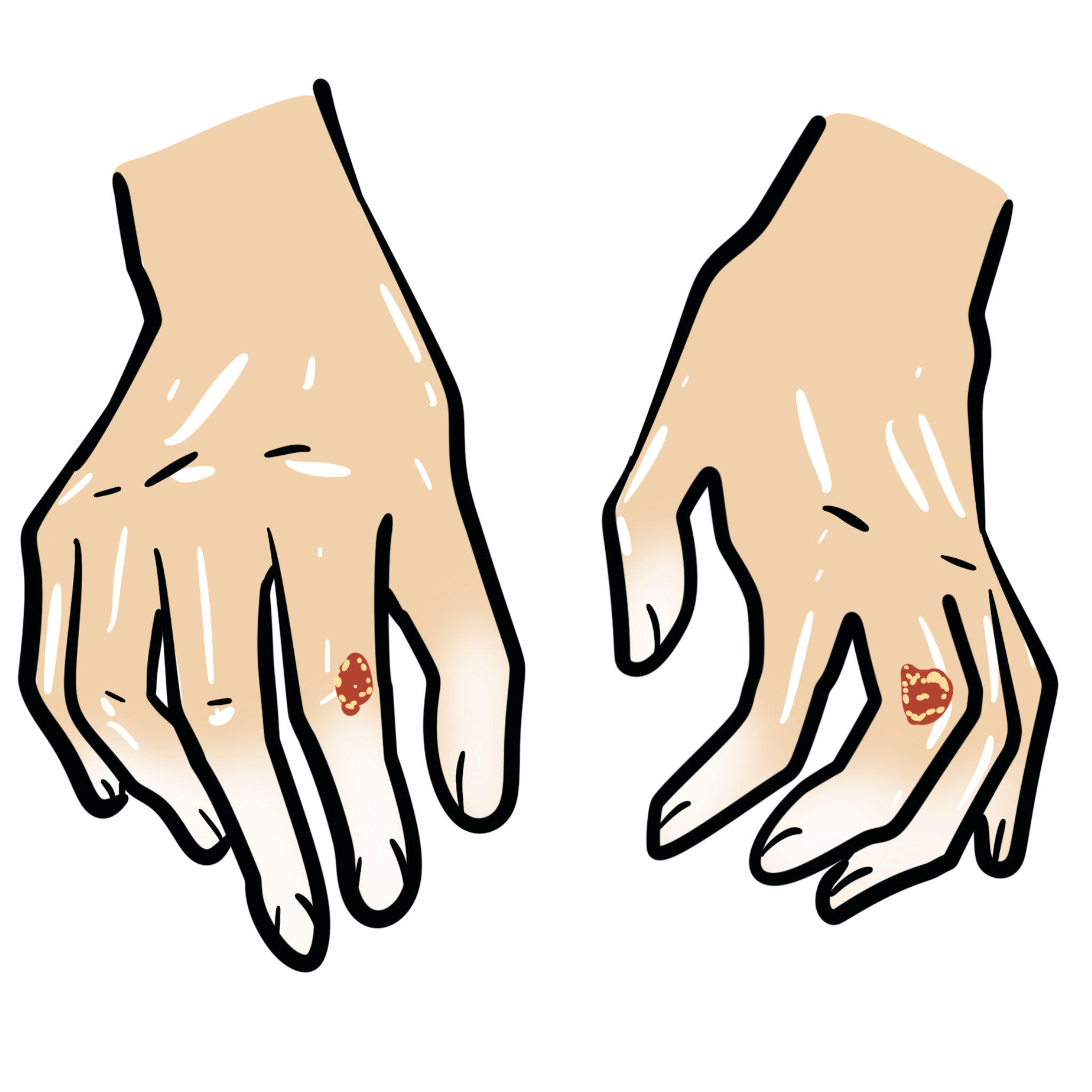
- Reduced neutrophil count leads to increased susceptibility to infections, particularly skin and respiratory tract
Think
Always consider Felty syndrome in patients with long-standing RA and unexplained recurrent infections.
Clinical Manifestations
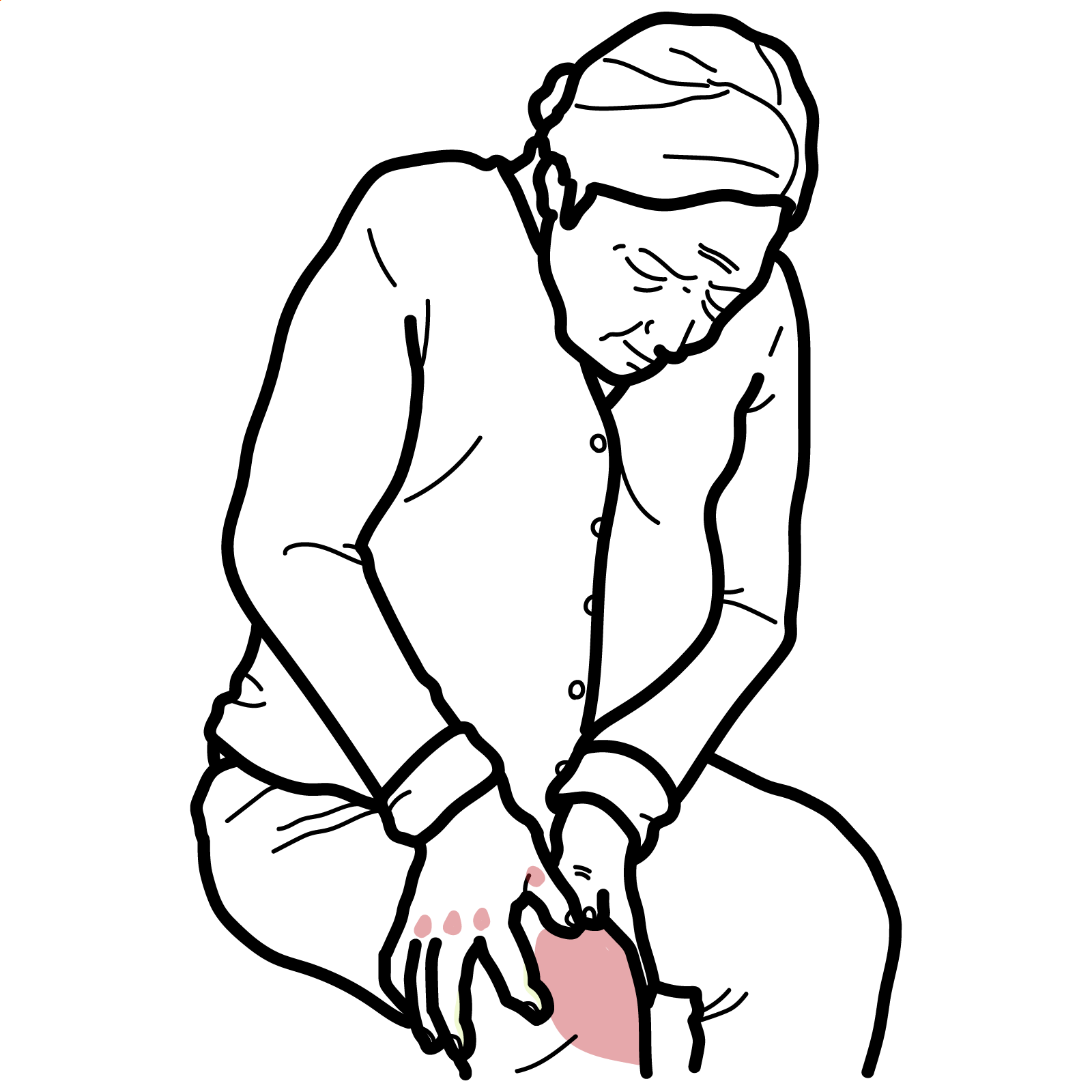
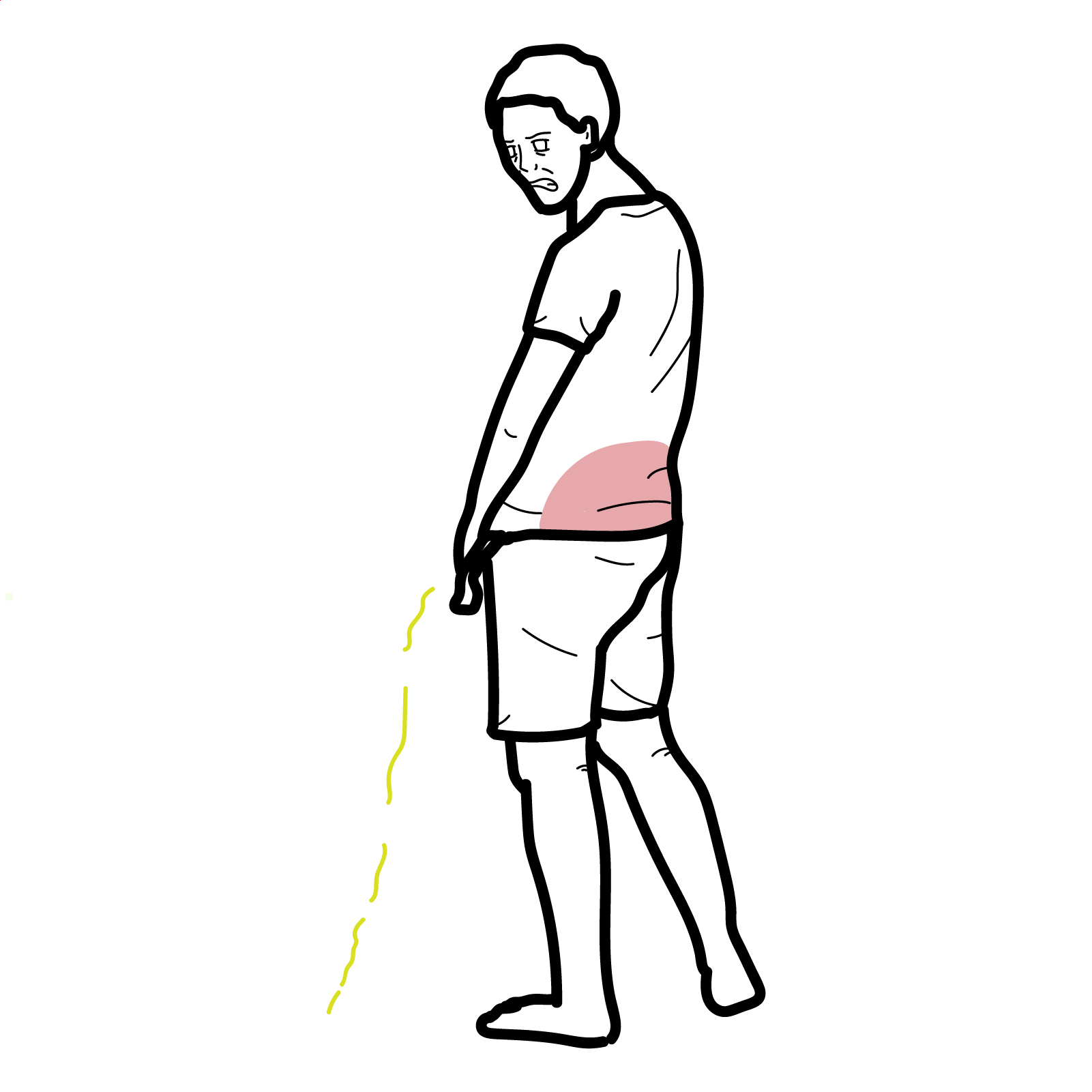
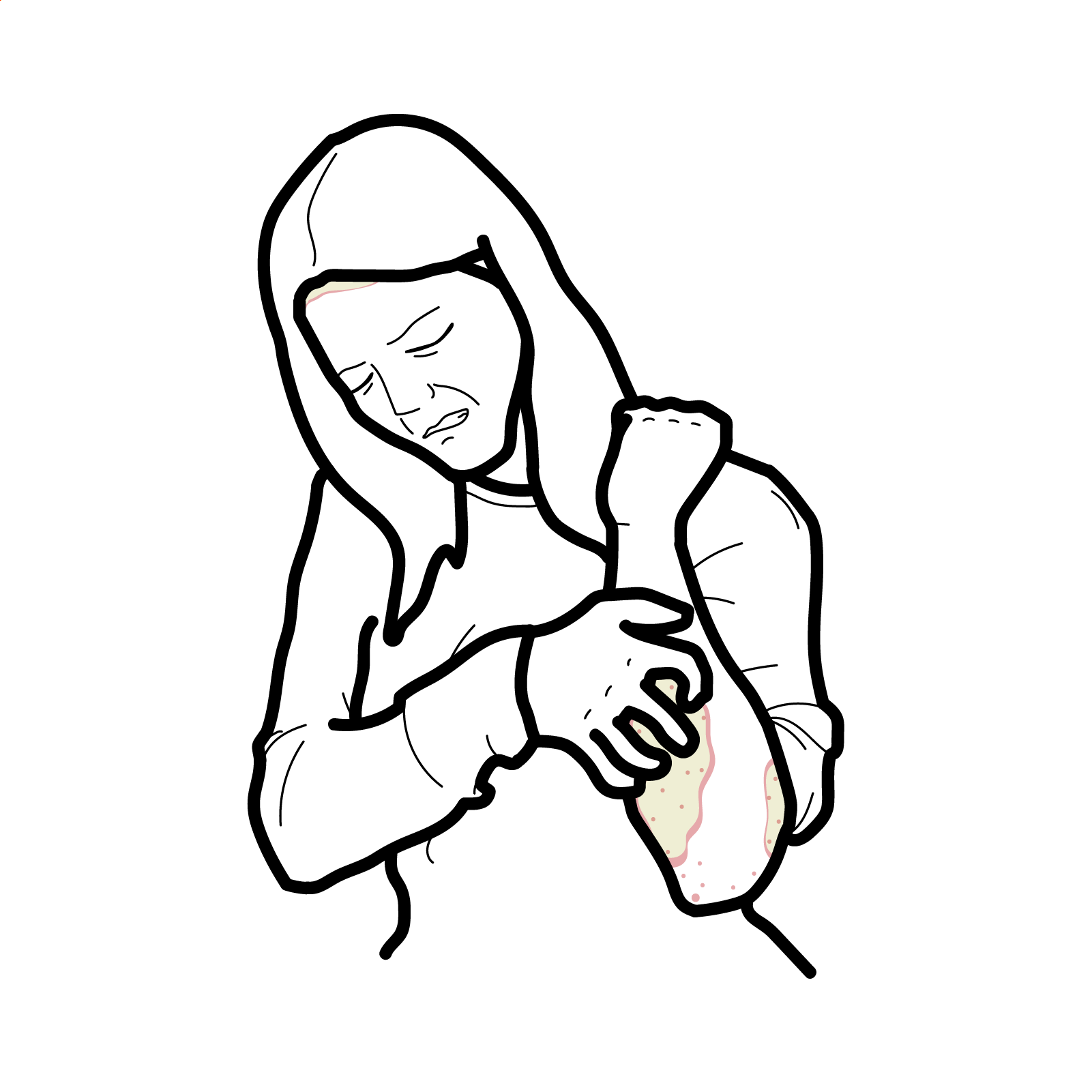
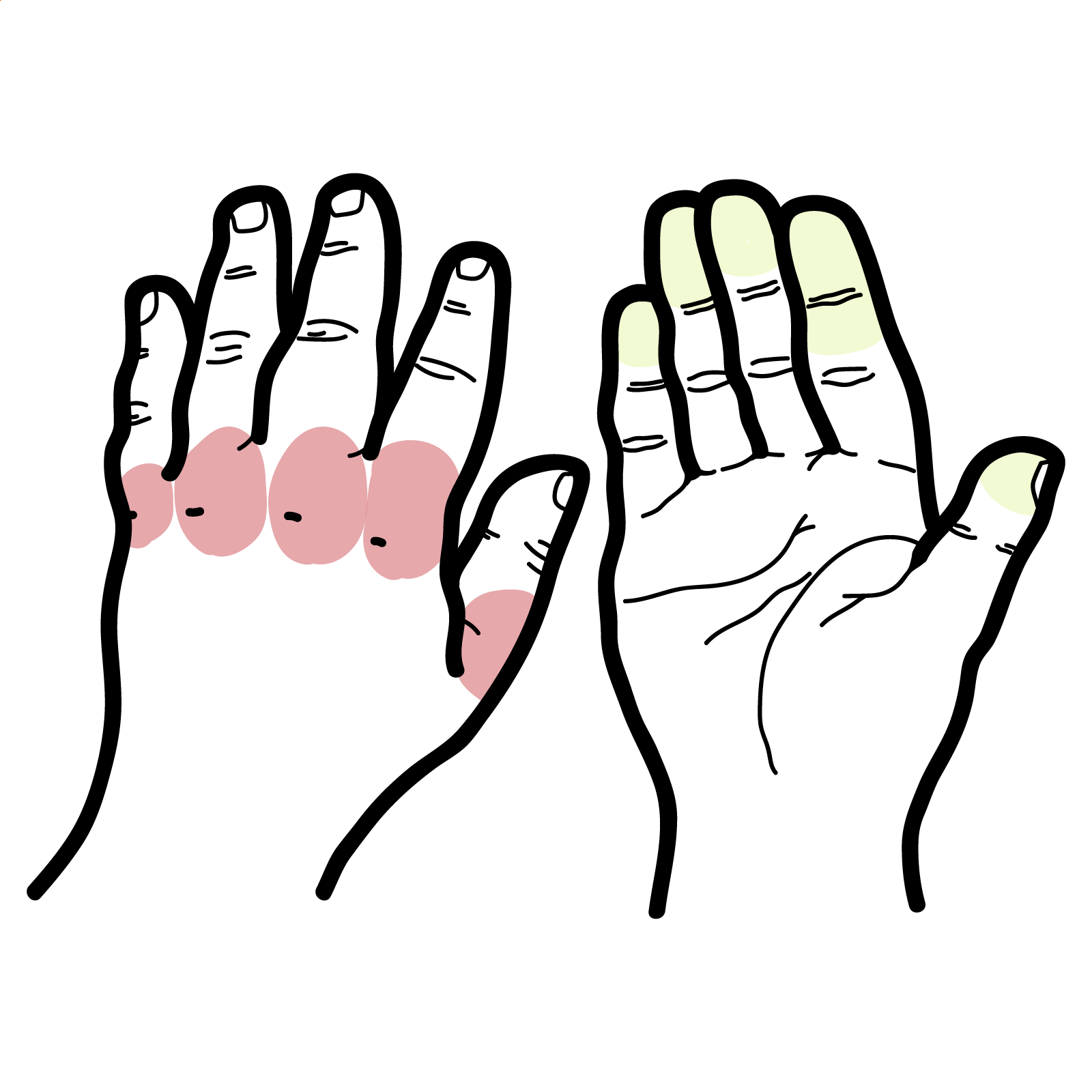
- Features of RA: joint pain, swelling, stiffness, especially in small joints
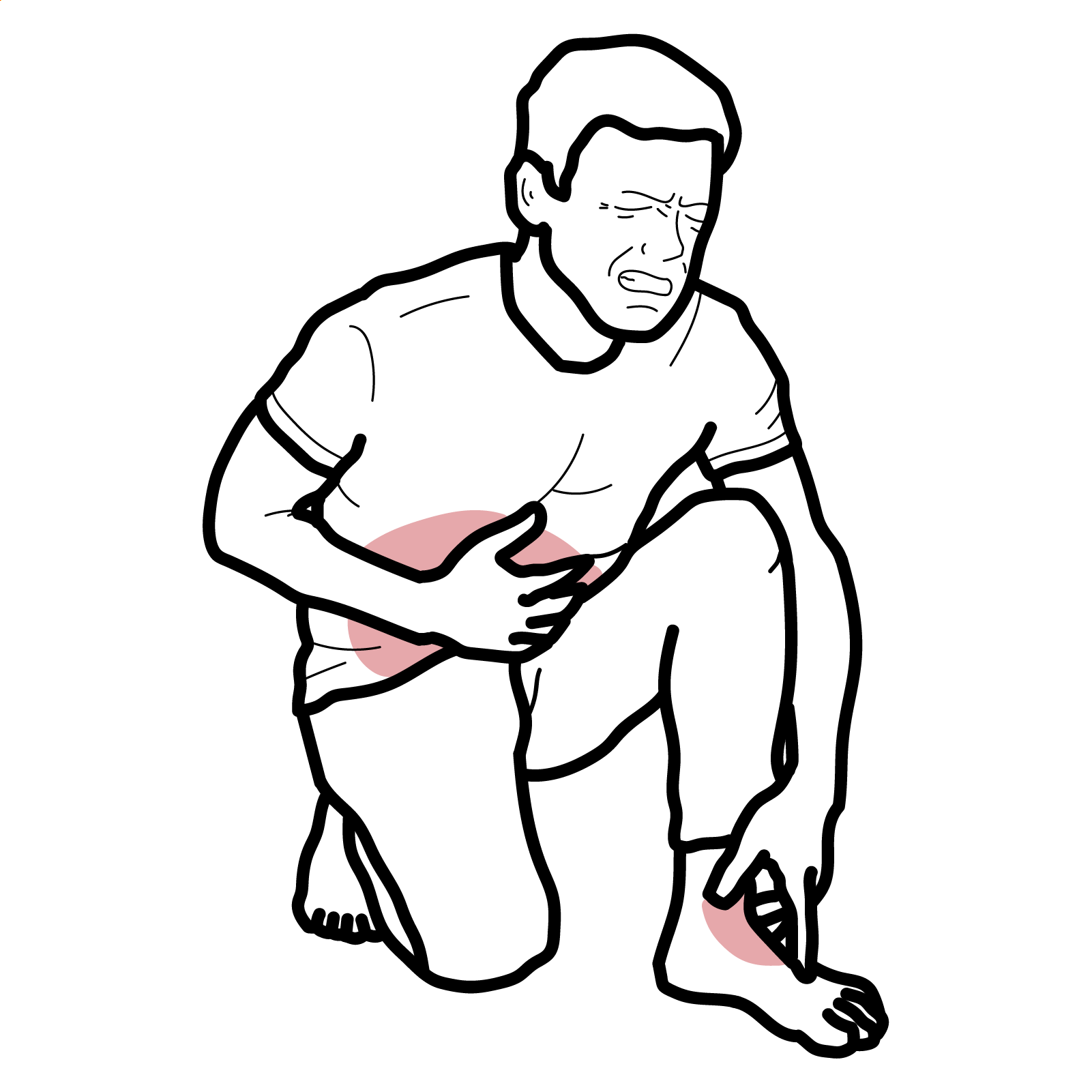
- Splenomegaly: may be asymptomatic or present as fullness in the left upper quadrant
- Neutropenia: leads to recurrent infections — skin ulcers, pneumonia, sepsis
- Extra-articular RA features: anemia, thrombocytopenia, lymphadenopathy, leg ulcers, hepatomegaly
- Possible constitutional symptoms: fatigue, low-grade fever, weight loss
Triad: Rheumatoid arthritis, Splenomegaly, Neutropenia
Diagnosis
Diagnostic criteria (clinical diagnosis based on classic triad; no universal criteria established):
• Known seropositive RA
• Absolute neutrophil count <2000/μL
• Splenomegaly on imaging or examination
Investigations
• FBC: neutropenia, anemia, thrombocytopenia
• ESR/CRP: elevated in active RA
• RF and anti-CCP: usually positive
• ANA: may be positive
• LFTs: mild elevation possible
• Bone marrow biopsy: to exclude myelodysplastic syndrome
• Imaging: ultrasound/CT showing splenomegaly
• Synovial fluid analysis (if effusion present)
Differential diagnoses
| Condition | Key Features | Differentiating Points |
| Large granular lymphocytic (LGL) leukemia | Neutropenia + splenomegaly | Clonal T-cells on flow cytometry |
| SLE | Cytopenias, autoantibodies | Malar rash, renal, serositis; lacks erosive arthritis |
| Myelodysplastic syndrome | Pancytopenia, dysplasia | Bone marrow biopsy shows dysplastic changes |
| Hypersplenism | Cytopenias with splenomegaly | No RA or autoantibodies |
Think
Always rule out LGL leukemia with flow cytometry when neutropenia is present with RA【2】.
Treatment
Control RA inflammation:
- Consider lowering methotrexate dose initially (potential cause of neutropenia)
- Control RA with csDMARD and bDMARD: methotrexate, leflunomide
- bDMARDs: Rituximab or anti-TNF agents
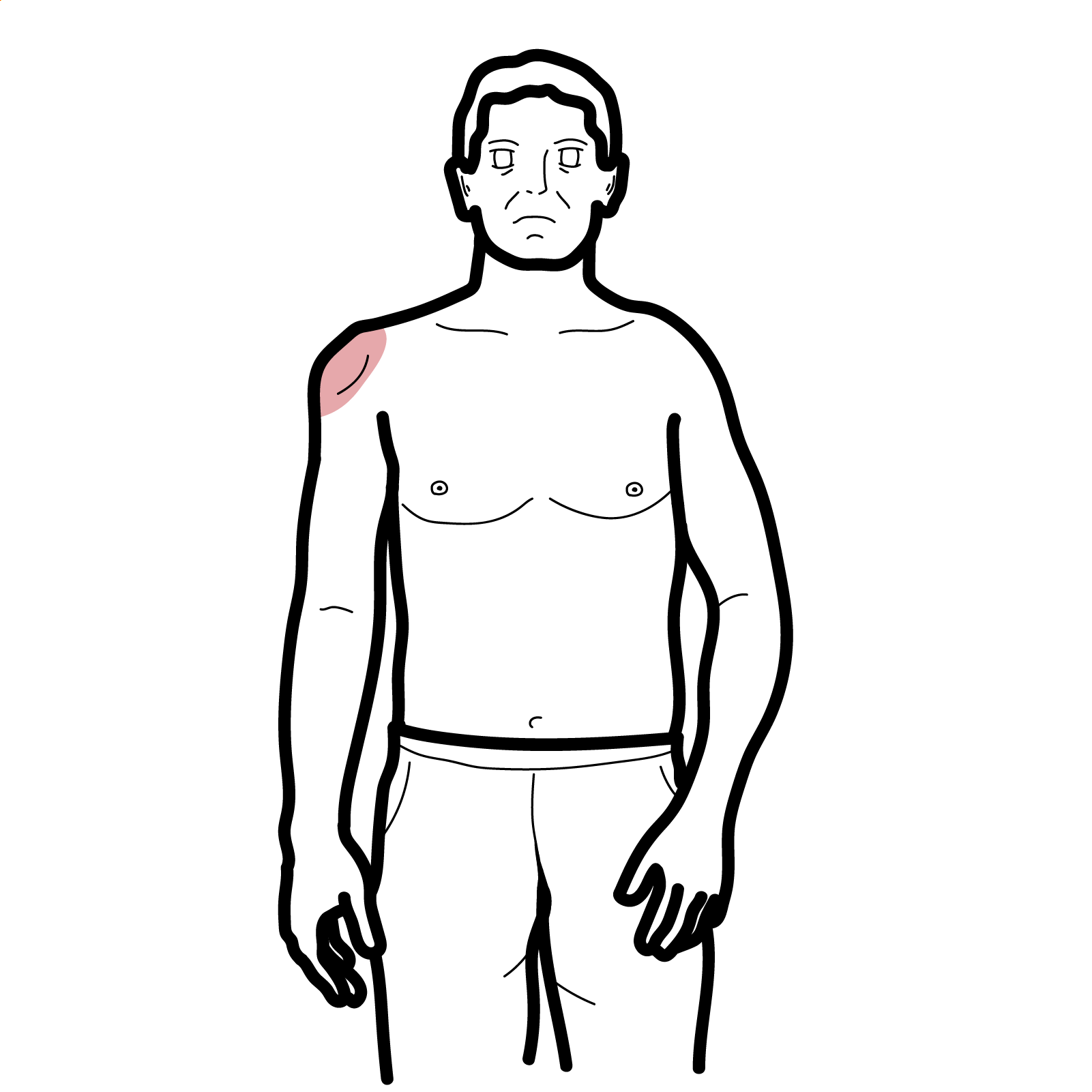
Treat neutropenia:
- G-CSF (e.g. filgrastim)
- Consider splenectomy if persistent symptomatic neutropenia
Manage infections promptly
- Prophylactic antibiotics not routinely recommended but early use during infection is critical
- Skin ulcer care
Complications and Prognosis
- Recurrent and severe infections
- Leg ulcers — difficult to treat, chronic
- Hematological malignancy (especially LGL leukemia)
- Bone marrow failure
- Ongoing neutropenia despite splenectomy
Prognosis depends on recurrent infection. Splenectomy may normalise Neutrophil count in 50-80 of refractory cases.
References
- Owlia MB, Newman K. Felty’s syndrome, insights and updates. Open Rheumatol J. 2011;5:129–36.
- Moosig F, et al. Large granular lymphocyte expansion in Felty’s syndrome and rheumatoid arthritis: a clinical and pathophysiological study. Arthritis Res Ther. 2008;10(3):R71.
- Bartok B, Firestein GS. Fibroblast-like synoviocytes: key effector cells in rheumatoid arthritis. Immunol Rev. 2010;233(1):233–55.



Discussion