
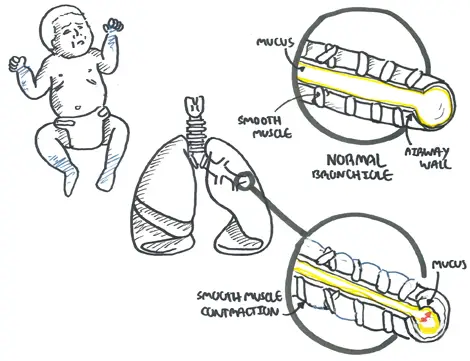
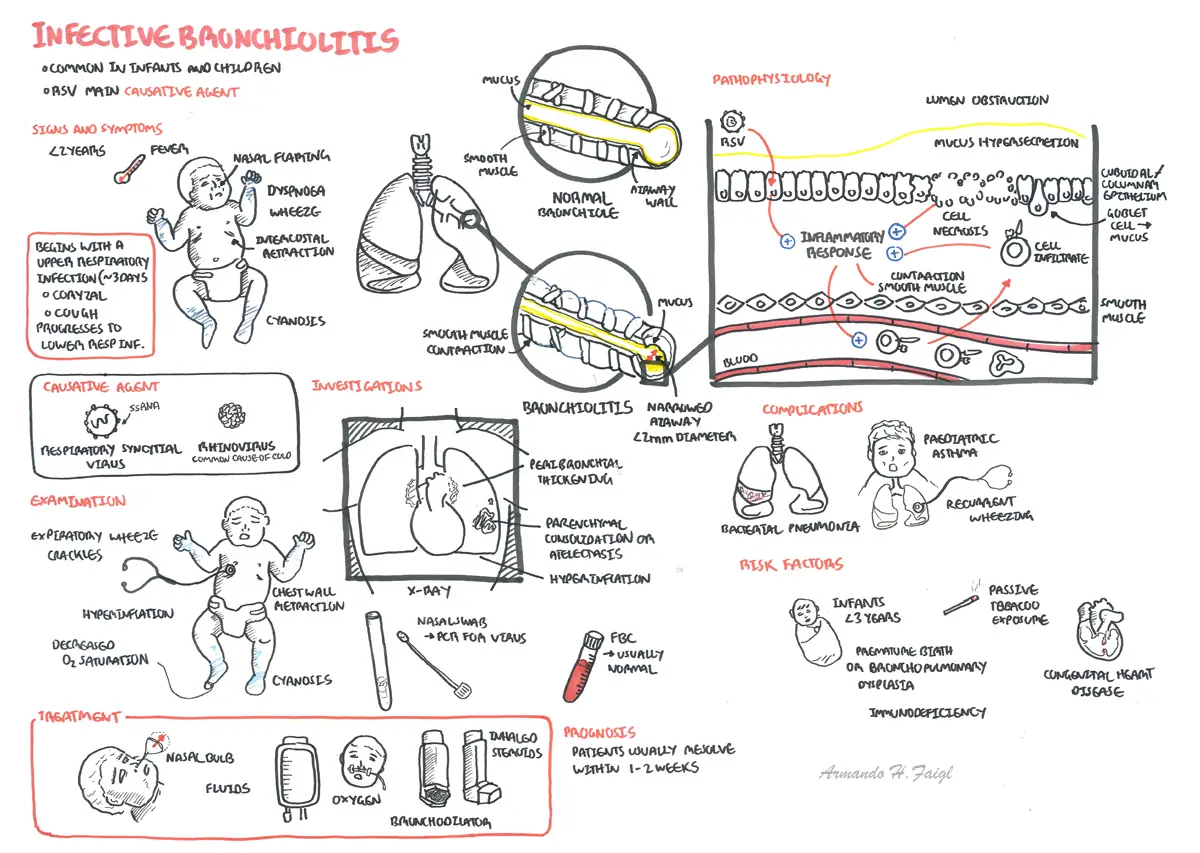
Overview Bronchiolitis is often a viral cause mainly Respiratory Syncytial Virus (RSV). Bronchiolitis is the most common respiratory tract infection of neonates and is usually self-limiting. A major source of confusion of treatment is differentiating a viral bronchiolitis to asthma. In summary bronchiolitis is usually seen in infants <2yo. Asthma is seen in older children.
Risk factors for severe bronchiolitis
| Side note Exclusive breastfeeding for at least 6 months is recommended to decrease the morbidity of respiratory infections. |
Examination
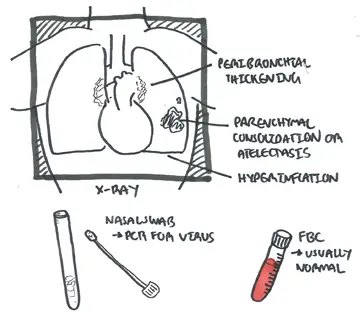
Diagnosis Clinical Diagnosis

Clinical Presentation Nasal obstruction +/- rhinorrhea and an irritating cough are usually noticed first. After one to three days there follows increasing tachypnoea and respiratory distress. The chest is often overexpanded.
Mild bronchiolitis
Moderate bronchiolitis
Severe bronchiolitis
High Risk Group
In most children with bronchiolitis no investigations are required unless severe.
Winter Respiratory Syncytial Virus (RSV)
Others
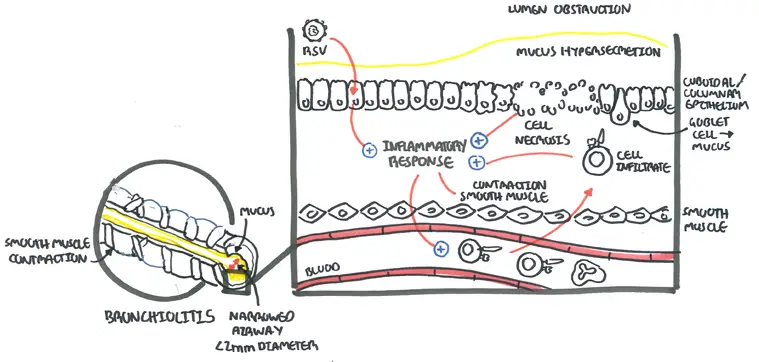
An RSV infection begins with replication of the virus in the nasopharynx. The virus spreads to the small bronchiolar epithelium lining the small airways within the lungs, and a lower respiratory tract infection can begin in one to three days. If a lower respiratory tract infection occurs, it causes edema, increased mucus production, and eventual necrosis and regeneration of these epithelial cells. This leads to small airway obstruction, air trapping, and increased airway resistance ()
Oxygen if saturation drops to 95%
Mild bronchiolitis
Moderate bronchiolitis
Severe bronchiolitis
Fluids
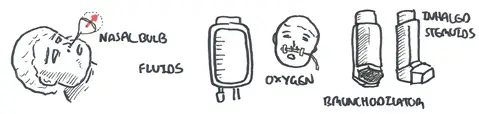
Pharmacological Therapy
| Remember Bronchodilators (albuterol, salbutamol), epinephrine, and corticosteroids are generally not administered to infants and children with the diagnosis of bronchiolitis. Only if another condition is suspected or person is not getting better |
Discharge
Complications
Prognosis 40 percent of children with bronchiolitis will develop further wheezing episodes through five years of age, and 10 percent will have wheezing episodes beyond this age.
Summary
| Watch: Bronchiolitis Overview |
