Systemic Sclerosis (SSc)
Systemic sclerosis (SSc), also known as scleroderma, is a rare chronic autoimmune connective tissue disease characterized by fibrosis, vasculopathy, and autoimmunity. It primarily affects the skin but can also involve the lungs, GI tract, kidneys, and heart. The estimated prevalence is 50–300 per million, with a female-to-male ratio of ~4:1, and peak onset between 30–50 years. There are two main clinical subsets: limited cutaneous (lcSSc) and diffuse cutaneous (dcSSc), with differing organ involvement and prognosis.
Systemic sclerosis (SSc): Chronic autoimmune disease with progressive fibrosis of skin and internal organs, vasculopathy, and specific autoantibodies.
CREST syndrome: Subset of limited SSc (Calcinosis, Raynaud’s, Esophageal dysmotility, Sclerodactyly, Telangiectasia).
Fibrosis: Excess deposition of extracellular matrix (mainly collagen).
Raynaud’s phenomenon: Episodic vasospasm of digits in response to cold/stress.
TGF-β is the central cytokine driving fibrosis.
| Feature | Limited Cutaneous SSc (lcSSc) | Diffuse Cutaneous SSc (dcSSc) |
| Skin Involvement | Distal to elbows and knees (face, hands, forearms, feet) | Proximal and distal limbs, trunk, face |
| Onset & Progression | Gradual onset; slow progression | Rapid onset; early organ involvement |
| Raynaud’s Phenomenon | Precedes skin changes by months/years | Occurs concurrently or after skin changes |
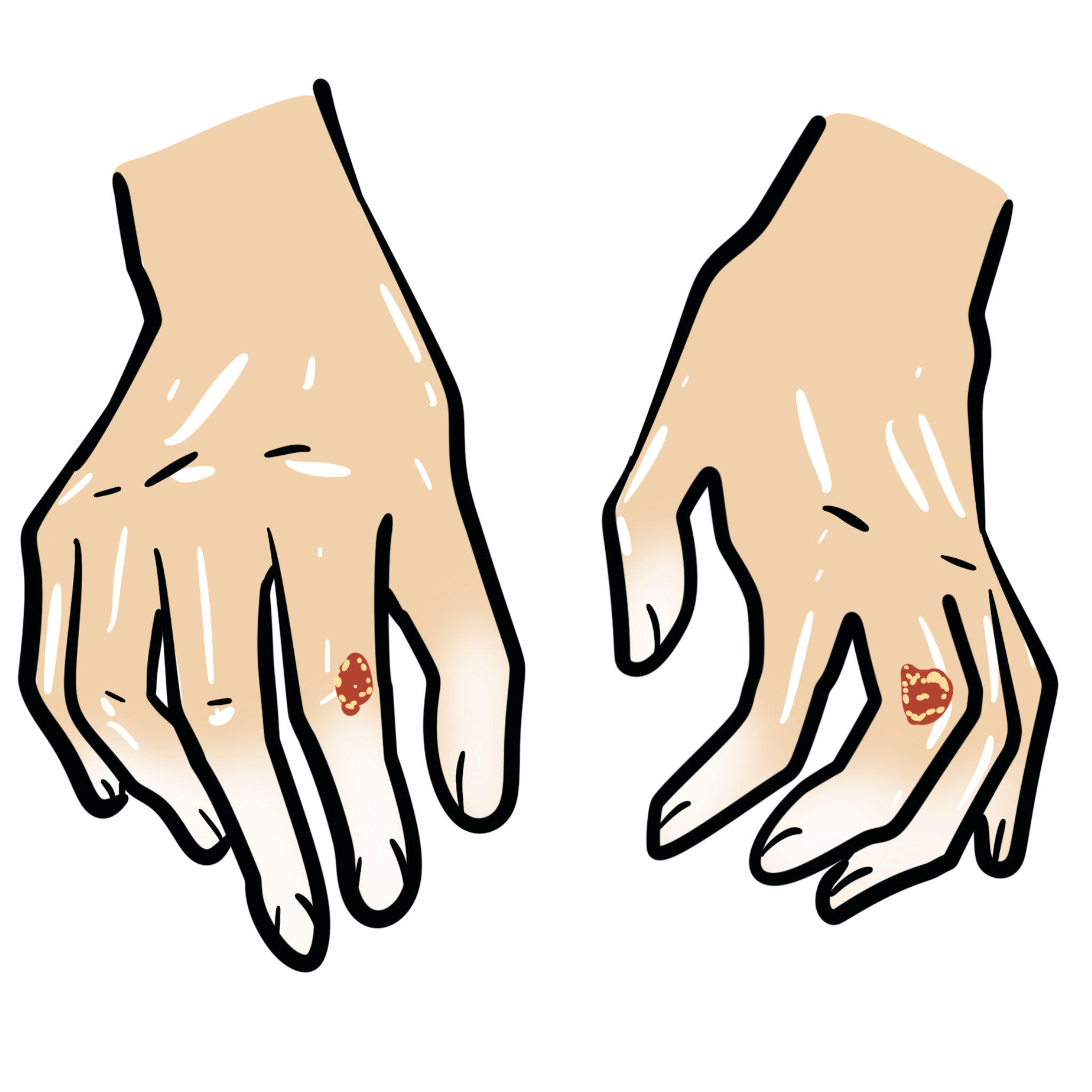
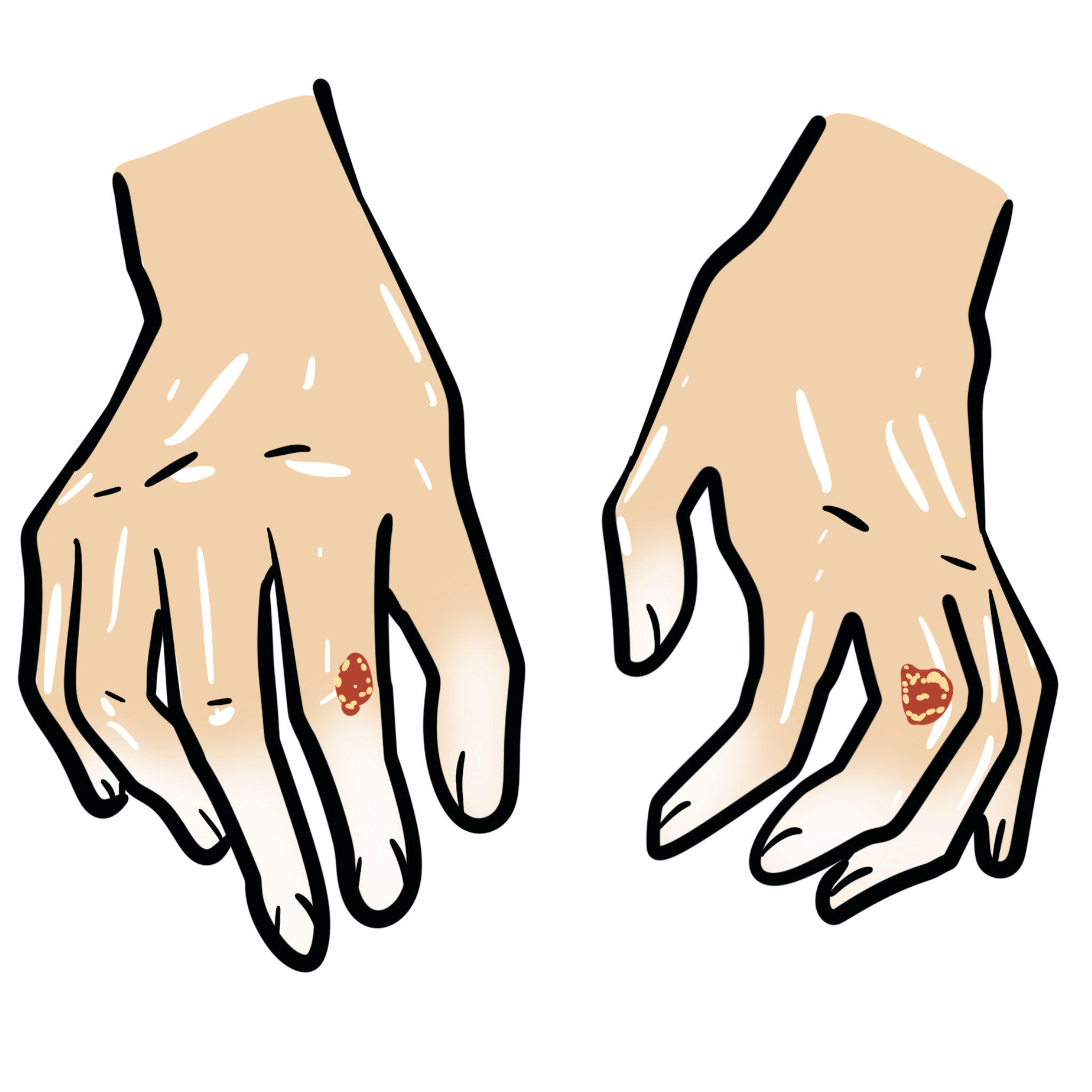
| Skin Features | Sclerodactyly, digital ulcers, telangiectasias, calcinosis cutis (CREST) | Sclerodactyly, diffuse skin thickening, hyperpigmentation |
| GI Involvement | Esophageal dysmotility common; late small bowel involvement | Early and more severe GI involvement (including malabsorption, pseudo-obstruction) |
| Pulmonary Involvement | Pulmonary arterial hypertension (PAH) more common | Interstitial lung disease (ILD) more common |
| Renal Involvement | Rare | Scleroderma renal crisis (SRC) — life-threatening |
| Cardiac Involvement | Arrhythmias possible | More common: myocarditis, pericardial effusion, conduction defects |
| Vascular Manifestations | Telangiectasia, digital ischemia | Digital ischemia, fingertip pitting/scars |
| Autoantibodies | Anti-centromere (ACA) | Anti-Scl-70 (topoisomerase I), anti-RNA polymerase III |
Raynaud’s may predate systemic symptoms by years — always screen ANA and ENA in persistent cases.
CREST
Calcinosis cutis
Raynaud’s phenomenon
Esophageal dysmotility
Sclerodactyly
Telangiectasia
Diagnostic Criteria: 2013 ACR/EULAR Criteria
RNA polymerase III is associated with rapid scleroderma, renal criss and GAVE.
Differential Diagnoses
| Condition | Differentiating Feature |
| SLE | Malar rash, arthritis, more systemic but no skin thickening |
| Dermatomyositis | Heliotrope rash, proximal muscle weakness, Gottron’s papules |
| Mixed CTD | Overlapping features; high anti-U1 RNP |
| Eosinophilic fasciitis | Skin tightening sparing fingers, eosinophilia |
| Scleromyxedema | Generalized waxy papules, mucin deposition, monoclonal gammopathy (usually IgG λ), no Raynaud’s, no internal organ fibrosis |
Use nailfold capillaroscopy + ENA panel in all cases with Raynaud’s + skin symptoms.
| Subtype | Features |
| Limited cutaneous (lcSSc) | Distal skin involvement (fingers, face), CREST, late organ involvement, anti-centromere antibodies |
| Diffuse cutaneous (dcSSc) | Proximal limb/trunk skin thickening, early organ fibrosis, renal crisis, anti-Scl-70/RNA pol III |
| Sine scleroderma | Internal organ involvement without skin changes |
| Overlap syndromes | Features of SSc + another CTD (e.g. SLE, myositis) |
No cure — aim to control symptoms and prevent complications
Supportive
• Annual echocardiogram (or pBNP) and PFTs
• Occupational therapy for hand function
• Regular BP monitoring
ACE inhibitors are life-saving in scleroderma renal crisis.
ASCT should only be considered in high-volume centers with multidisciplinary teams. Careful pre-transplant cardiac screening is essential due to risk of treatment-related mortality. HSCT does not cure systemic sclerosis but may induce long-term remission in selected patients.
Complications
Poor Prognostic Factors
In young patients with early aggressive dcSSc and deteriorating lung function despite immunosuppression, refer early for HSCT evaluation.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion