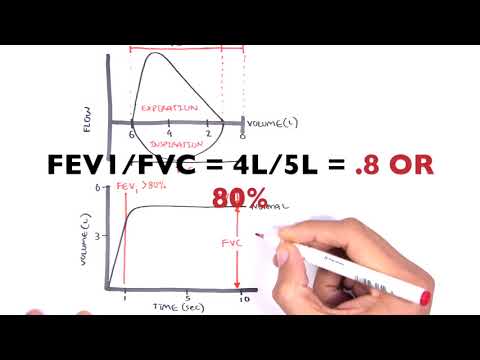
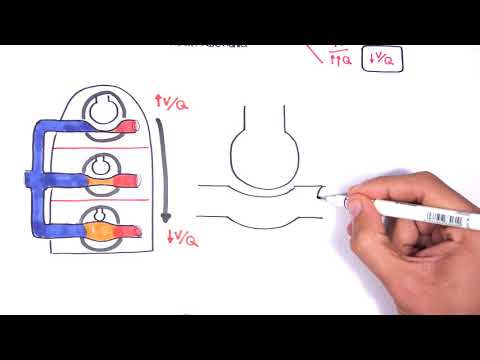
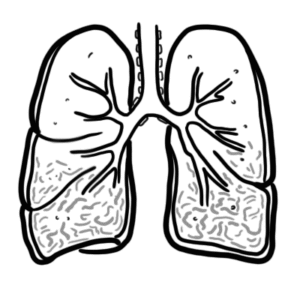
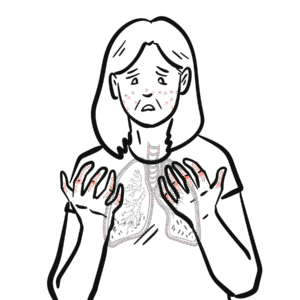
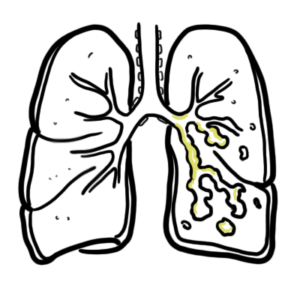
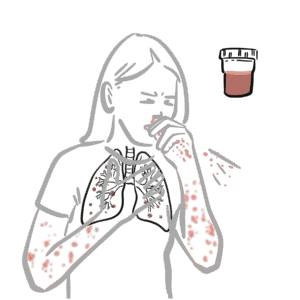
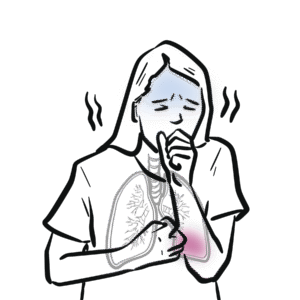
0:00 In this video, we're going to look at COPD, Chronic Obstructive Pulmonary 0:07 Disease. 0:09 This is an overview, an introduction. 0:11 COPD encompasses a number of diseases, including emphysema, chronic bronchitis, 0:17 and chronic asthma. 0:20 In this video, we will mainly focus on and compare chronic bronchitis and emphy 0:26 sema. 0:27 Let us first begin by looking at the signs and symptoms of both of these. 0:32 Patients with emphysema are also known as the pink puffers, because they have 0:37 difficulty 0:37 breathing, but are well-perfused. 0:41 Patients with chronic bronchitis are also known as the blue bloaters, because 0:45 they are 0:45 usually signosed. 0:48 Some signs and symptoms in emphysema and chronic bronchitis include dyspnea, 0:53 difficulty breathing, 0:55 having a productive cough and chest tightness. 0:59 Patients with pure emphysema have a barrel chest, muscle wasting, as well as 1:04 pursed lips. 1:08 Patients with pure chronic bronchitis can have peripheral edema and a raised J 1:14 VP, due to 1:14 a potential right-sided heart failure. 1:21 Let us now look at the pathology. 1:24 Here I am drawing a lung. 1:26 Let us first begin by looking at changes that occur in emphysema. 1:31 Pure emphysema mainly affects the functional units of the lungs, which are the 1:38 alveoli. 1:39 Alveoli are covered with elastic fibers, which allow the alveoli to expand and 1:44 recoil back, 1:45 pushing air out as we exhale. 1:48 However, in emphysema, what we see is a loss of elastic fibers. 1:55 You also have a decrease in surface area of the alveoli. 1:59 This could potentially lead to a collapsed alveoli. 2:04 You can have something called air trapping occurring, which is where air is 2:09 still trapped 2:10 in the alveoli as we exhale, because the recoil mechanism is not working. 2:18 In pure chronic bronchitis, we have problems along the airway tract, 2:22 specifically the bronchioles. 2:25 Here I am drawing a normal bronchiol with smooth muscle and mucus. 2:31 In chronic bronchitis, we have smooth muscle hypertrophy and contraction, as 2:37 well as mucus 2:38 hyper secretion. 2:41 This all leads to difficulty breathing. 2:46 Some risk factors for COPD, both emphysema and chronic bronchitis, include 2:52 smoking, advanced 2:53 age, low socioeconomic status, genetic factors, constant exposure to air 2:59 pollution, and developmentally 3:02 abnormal lungs, which predisposes one to COPD. 3:09 Examples that should be performed in a suspected person with COPD include HSX- 3:16 ray, where findings 3:18 can include a flattened diaphragm and hyperinflation. 3:25 Another important investigation or examination to perform is asperometry. 3:31 Asperometry is a machine that a patient blows into. 3:36 This is to measure the lung function. 3:40 Here we have a normal sprometry reading with a normal inspiratory and expir 3:46 atory curve. 3:48 However, let's compare this to a graph with someone who has COPD. 3:54 So again, here we have the normal inhalation and exhalation curve in black and 3:59 in red COPD. 4:01 There is a decrease in volume, especially during exhalation. 4:07 The criteria to diagnose COPD is forced expiratory volume 1 over forced vital 4:13 capacity ratio, 4:14 less than 70%. 4:17 Also to be sure it is COPD, the administration of a bronchoid dilator following 4:22 the first 4:23 sprometry reading should improve the lung function. 4:28 And so on the next brometry reading, the graph should go closer to normal. 4:36 The management of COPD involves smoking cessation, use of oxygen in late stage, 4:42 bronchoid dilators 4:43 B2 agonists or M3 antagonists, and steroid inhalers for as a preventer. 4:58 [BLANK_AUDIO]