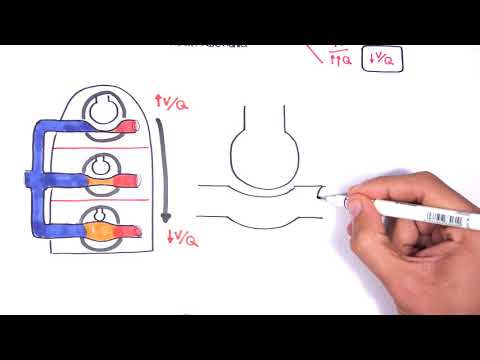
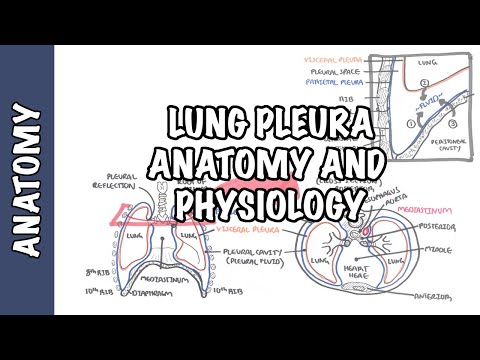
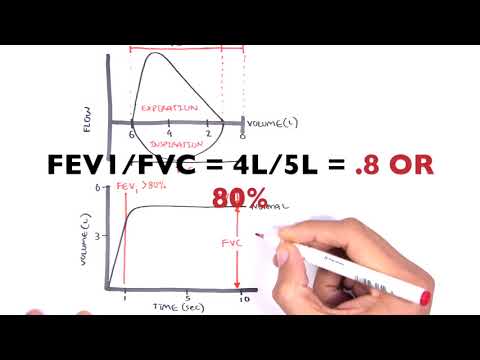
0:00 Now, let's proceed to investigations, what sort of investigations would you 0:13 perform if 0:15 someone presents with difficulty breathing, sputant production, as well as a 0:22 cough? 0:23 So number one is spirometry. 0:24 Now here is what it looks like essentially. 0:26 So basically what happens is you take a massive deep breath in and a forced exh 0:31 ale out for 0:32 about five, six seconds. 0:36 And this will give you a spirometry reading which can be printed out. 0:39 Now let's look at a normal spirometry graph that gets usually showed on the 0:45 paper or on 0:46 the screen. 0:47 So the spirometry can give you a graph. 0:50 We have flow on the y-axis and volume, the volume of air in the lungs or exh 0:57 aled out 0:58 or inhaled in on the x-axis. 1:01 So it's just the volume of air on the x-axis. 1:04 So here you're taking a deep breath in, a deep inspiration, and here you are 1:09 performing 1:10 a forced quick expiration and you do it for about six seconds. 1:14 So you're trying to empty out your lungs. 1:18 We can also find other measurements using just this graph. 1:22 The volume on the x-axis is therefore your total lung capacity and the amount 1:27 of air remaining 1:28 in the lung after your forced expiratory volume is your residual volume. 1:33 So this always stays there. 1:36 The amount of air following deep inspiration and forced expiration is known as 1:42 your vital 1:43 capacity. 1:45 When evaluating a patient with possible COPD, spirometry is performed. 1:51 Now spirometry is performed pre and post bronchodilator admission to determine 1:57 whether air flow limitation 1:58 is present, partial, or it's fully reversible. 2:04 So let us look at what the spirometry graph will look like in an obstructive 2:09 lung disease 2:10 such as chronic obstructive pulmonary disease, which again encompasses asthma, 2:15 chronic bronchitis, 2:16 and emphysema. 2:19 Here is the flow to volume diagram. 2:23 So the patients do lose some inspiratory volume when taking a deep breath in 2:27 and when breathing 2:28 out as hard and quick as possible, it becomes difficult to breathe out as time 2:34 progresses. 2:35 So as you exhale, forced exhale out for six seconds, it becomes more and more 2:40 difficult. 2:41 So you see here the dotted lines represent normal deep inspiration and normal 2:46 forced 2:47 expiration. 2:50 Compared to the normal spirometry on the right, in the obstructive spirometry, 2:56 you can see 2:58 a dent in the forced expiratory phase, which is indicative of the obstructive 3:08 pattern. 3:09 In obstructive, we have a decrease in forced expiratory volume and a decrease 3:16 in the forced 3:18 expiratory volume over forced viral capacity ratio. 3:22 Now a decrease of 70% of this ratio is indicative of COPD. 3:28 So again, less than 70% is like a diagnosis. 3:34 So because we looked at obstructive disease on the spirometry, we might as well 3:38 look at 3:38 restrictive lung problems. 3:41 So restrictive lung problems is actually much more obvious in that if this was 3:46 your normal 3:47 breathing, restrictive gives you something like this, a big decrease in both 3:52 flow and 3:53 volume. 3:54 Okay, so that was spirometry. 3:58 Another investigation you can perform is chest x-ray, which helps you rule out 4:03 cancers, 4:03 as well as other heart problems. 4:06 But you do see some features in advanced COPD. 4:10 So if here is a chest x-ray, you can see hyper-expansion or hyperinflation of 4:17 the lungs, which also 4:18 means you could have a flattening of the diaphragms, which is a sign of hyperin 4:23 flation as well. 4:25 Here, we can have also pulmonary hypertension, which means that there is a 4:32 prominent hyala 4:34 vascular shadow. 4:37 You also may find a bully, a fluid build-up in certain types of emphysema. 4:44 Also when you look at a chest x-ray, the chest x-ray can look darker within the 4:49 lungs, the 4:50 gas with the air, so the lung shadow can look a lot darker because there is a 4:56 lot of air 4:56 trapped. 5:00 We can also perform a pulse oximetry to check for oxygen saturation and the 5:04 signs of hypoxemia. 5:06 A full blood count is important to check for signs of anemia. 5:13 Arterial blood gas is another investigation to check for pH, so I guess the 5:18 severity of 5:19 the respiratory problem. 5:21 If the problem can also be respiratory acidosis or respiratory alkalosis, but 5:24 typically it's 5:25 respiratory acidosis. 5:27 Usually in COPD, especially late stage, it's respiratory acidosis. 5:32 ECG is also important to check for heart involvement and to rule out MI and 5:39 heart failure. 5:41 Here we are looking at an ECG strip. 5:43 Here is a normal ECG with the PQRST waves. 5:51 On an ECG for a person who has severe chronic bronchitis, for example, we may 5:57 see signs 5:58 of right ventricular strain. 6:03 This in a right ventricular strain on leads V1 to V4, we can see inverted T 6:12 waves. 6:13 That was some investigations that you can perform, the main ones. 6:18 People can have different severities of chronic obstructive pulmonary disease. 6:22 They can have different severities. 6:23 There is a classification made to categorize this. 6:28 The classification helps to assess the severity so that appropriate management 6:33 and treatment 6:33 can be made. 6:35 This is the classification, which is also for the diagnosis, by the way. 6:40 We will look at the severity of the COPD as well as the forced respiratory 6:48 volume 1. 6:50 Let's look at stage 1. 6:51 Stage 1 is mild severity. 6:54 The ratio, the FEV over FVC ratio is less than 70%, which is, again, important 7:00 because 7:01 it diagnoses obstructive pulmonary disease. 7:04 For mild COPD, the FEV1 is equal to or greater than 80 predicted. 7:14 We will look at mainly the American system, I think, but it is important to 7:18 note the Australian. 7:20 In Australia, the FEV1 can be between 60% to 80%, and this can be classified as 7:27 mild. 7:28 Stage 2, which is moderate, the ratio, again, has to be below 70 because that 7:33 is your diagnosis 7:34 of obstructive. 7:36 The FEV1 is between 50% to 80% predicted, but in Australia, this is moderate is 7:42 classified 7:43 as between 40% to 59%. 7:47 Stage 3 is severe, which is where the ratio is less than 70%, which is normal 7:53 for COPD. 7:54 Then we have the FEV1, which is between 30% to 50% predicted. 7:58 In Australia, severe is classified as below 40%. 8:03 There is another staging, which is stage 4, which is very severe. 8:07 This is where the ratio FEV1 to FVC ratio is less than 70%. 8:14 But the FEV1, it can be less than 30%, or the FEV1 is less than 50, plus you 8:21 have chronic 8:22 respiratory failure, and chronic respiratory failure, you have two types, and 8:27 this depends 8:28 on the level of oxygen and carbon dioxide in your blood. 8:33 So 4 stages, different severities, and different FEV readings. 8:40 So that was the classification for the severity of COPD. 8:44 Now, how did we come to that? 8:46 Well, assessment of severity of condition is based on three factors, the 8:50 severity of 8:50 the symptoms, spirometry, and risk of exacerbations. 8:57 Using the three features above, you classify the COPD, which we just looked at, 9:02 mild, moderate, 9:03 severe, very severe, and using the COPD classification, as well as other 9:09 factors, you follow what's 9:10 called the gold guidelines for COPD management. 9:15 Before looking at the management of COPD, it's important to look at, just 9:19 quickly, the physical 9:21 examination. 9:22 When we perform a physical examination, what are some things we see? 9:26 So physical examination of emphysema is what we'll look at. 9:31 In examination of emphysema, we see prolonged respiratory phase, because we're 9:36 trying to 9:36 push the air out of our lungs. 9:39 There's also pursed lips. 9:41 There's also over-distached of the lungs, barrel chest, use of accessory 9:45 muscles. 9:46 There's decreased intensity of breath sounds. 9:50 And finally, we hear wheezing during oscillations. 9:55 Now let us move into the management. 9:57 We will look at the main things for management, according to the Davidson's 10:01 textbook. 10:02 So it is very important to stop smoking, smoking cessation, because smoking 10:08 increases 10:09 the severity of COPD. 10:11 That's common sense. 10:12 Number two is vaccination. 10:14 It's important to prevent exacerbations of COPD, because usually lung 10:18 infections make 10:19 things a lot worse. 10:20 So by vaccinating the patient, you prevent further problems. 10:26 Third management, which is very important, is the use and administration of 10:31 Bronco dilators. 10:32 So we're going to pharmacology now. 10:35 The two types of Bronco dilators, there's beta-2 agonists or anti-colonurgics. 10:43 Both beta agonists or anti-colonurgics can be short-acting or long-acting. 10:47 And they're typically inhaled. 10:50 So inhaled is the, it goes, you puffers, essentially. 10:56 So let us zoom into the lungs here, the bronchials. 10:59 And let's look at the short-acting Bronco dilators. 11:03 The short-acting SA. 11:05 These are prescribed on an as-needed basis. 11:10 What the short-acting Bronco dilators essentially do is that they decrease the 11:15 symptomatic exposure 11:17 in patients with less severe symptoms. 11:25 Short-acting Bronco dilators are not considered maintenance. 11:28 Long-acting Bronco dilators are needed for this. 11:32 Now let's look at the mechanism of action of the beta-2 agonists and the anti- 11:38 colonurgics. 11:43 So let's zoom into the layers of like the smooth muscle of the bronchial here. 11:49 So here we have the epithelial cells which are surrounded by the smooth muscles 11:54 . 11:54 The smooth muscles can contract and relax depending on the signals they are 11:58 receiving. 11:59 The smooth muscle have receptors on their cell surface. 12:02 These are the muscuringic 3 receptors as well as the beta-2 receptors. 12:07 The parasympathetic nerve supplies the smooth muscle of the airways and it 12:11 releases acetylcholine. 12:13 When acetylcholine binds to the M3 receptor, muscuringic 3 receptor, it 12:17 activates the G 12:19 protein, intracellularly, which stimulates the phospholipase C, converting PIP2 12:25 to IP3. 12:27 Essentially what's important is that IP3 is then responsible for the 12:33 contraction of the 12:34 smooth muscles downstream through the release of calcium. 12:40 Now the short-acting muscuringic antagonists, they essentially inhibit these M3 12:46 receptors 12:47 and so because they block the empty receptors on the respiratory smooth muscles 12:51 , it also 12:51 inhibits the downstream cascade thus inhibits the contraction of smooth muscles 12:57 . 12:58 I hope that made sense. 12:59 Now let us look at the beta-2 receptors. 13:03 Well adrenaline and noradrenaline from the sympathetic stimulation binds to 13:06 this receptor 13:07 and activates, stimulates G protein again, activating adenylate cyclase. 13:14 Activated adenyl cyclase converts ATP to cyclic AMP. 13:18 An increase in intracellular cyclic AMP causes or results in smooth muscle 13:25 relaxation. 13:26 Cyclic AMP is important because it causes smooth muscle relaxation and this is 13:30 a good 13:30 thing for obstructive lung diseases and so prescribing short-acting beta-2 agon 13:37 ist stimulates 13:38 the beta-2 receptors and thus leads to bronchodilation. 13:44 So looking at long-acting drugs, long-acting drugs are regularly scheduled. 13:51 Long-acting inhaled bronchodilators are added for those who are more severe and 13:58 they do 13:58 essentially the same thing but work for longer essentially and these are your 14:04 long-acting 14:05 muscuringic antagonists which inhibits the M3 and your long-acting beta-2 agon 14:10 ists which 14:11 stimulates your beta-2 receptors on smooth muscles in the respiratory airways. 14:19 Inhaled glucocorticoids are used in combination with long-acting bronchodil 14:23 ators and corticosteroids 14:25 are not used alone. 14:29 Number five pulmonary rehabilitation is another very important aspect of 14:34 management. 14:35 COPD patients often have a decreased physical level of physical activity 14:39 because of dyspnea, 14:40 a decrease in physical activity causes that leads to a vicious cycle so we get 14:45 worsening 14:46 dyspnea because we don't exercise, we lose muscle. 14:50 Now pulmonary rehabilitation aims to break this cycle through several things. 14:55 Firstly by exercising, through exercise, two, through nutrition because 30% of 15:01 severe 15:01 COPD patients have protein calorie malnutrition for example, three smoking 15:07 cessation, four 15:08 education of their condition, and five breathing exercises such as per slips 15:15 which helps with 15:16 the gas trapping. 15:18 Finally, there is also SIGS management which is oxygen therapy and this is very 15:24 important 15:24 for a chronic COPD who are suffering who has hypoxemia. 15:32 So the last management is the surgical intervention and there's two main ones. 15:37 The first is lung volume reduction surgery which is essentially removing parts 15:41 of the 15:42 lung that don't work and then this last one is lung transplantation which 15:47 obviously has 15:48 a criteria for that so I hope that made all sense. 15:54 Thank you for watching.