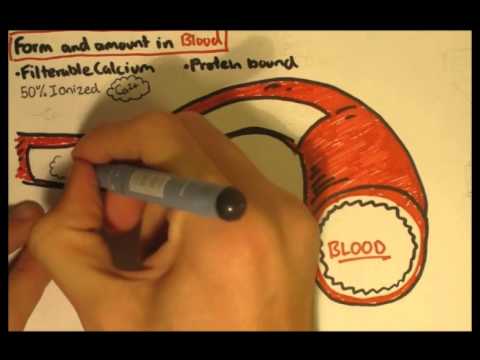
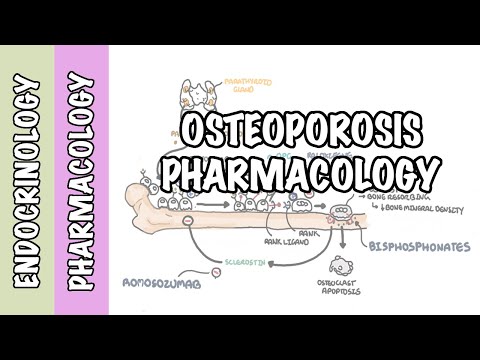
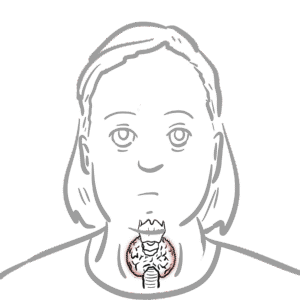
0:00 In this video, we're going to look at endocrinology, calcium and phosphate 0:06 regulation. 0:15 So the hormones essentially involved in regulating calcium and phosphate levels 0:20 in the blood. 0:21 And there's three important hormones involved. 0:24 These are vitamin D, parathired hormone, and calcitonin. 0:29 So like all endocrine systems, we should look at what glands and what tissues 0:33 are involved. 0:34 So here, I'm drawing the brain where we have the hypothalamus and the pituitary 0:38 gland. 0:38 But surprisingly enough, we won't really look at these in this video. 0:42 We will, however, look at this gland here called the thyroid gland, which is 0:46 situated 0:46 on our throat. 0:48 This is a dorsal view of the thyroid gland. 0:50 So it's the view from the back. 0:52 And at the back of the thyroid gland, we can find four glands, additional 0:58 glands, which 0:58 are different, called the parathired glands. 1:01 And we have four of these on the dorsal side of the thyroid gland. 1:05 Other important organs and stuff that we will talk about in this video include 1:11 the bone, 1:12 because this is where calcium and phosphate can be found, the minerals. 1:17 And actually, most of the calcium is 99% is stored in the bone. 1:22 And we also will talk about the kidneys, the gut, the GIT, the liver, as well 1:27 as the skin. 1:30 So let us first, the hormone that we'll first concentrate on is parathired 1:34 hormone. 1:35 But before that, we have to see what the significance of calcium and phosphate 1:39 is in 1:39 our body. 1:40 So we have to regulate calcium and phosphate levels, because for one, calcium 1:44 is important 1:45 for muscle contraction, nerve conduction. 1:50 And phosphate is important for other biochemical processes, as well as energy. 1:57 So now let's look at the first hormone, which is parathired hormone. 2:01 So parathired hormone is released when we have a decrease in plasma calcium 2:07 levels. 2:08 So a decrease in plasma calcium levels will stimulate the parathired gland to 2:14 release 2:14 a hormone called parathired hormone. 2:19 Parathired hormone targets a few things. 2:23 Firstly, it targets the bone. 2:25 It stimulates the bone to sort of break down its minerals so that calcium and 2:32 phosphate 2:33 can enter the plasma. 2:35 Therefore, it increases calcium and phosphate levels in the plasma. 2:39 The parathired hormone also targets the kidneys. 2:42 It targets the enzyme in the kidneys called one alpha hydroxylase. 2:47 One alpha hydroxylase's main function is to activate vitamin D. 2:52 So what it does is it converts a chemical to 25 hydroxyl vitamin D3, also known 2:57 as calcidiol, 2:59 to 125 dihydroxyl vitamin D3, which is calcitrial. 3:05 So calcitrial is the active form of vitamin D. 3:10 Calcidiol then targets a few things. 3:13 Firstly, it stimulates the bone as well somehow, and it to break it down so 3:17 that we can increase 3:19 the minerals, calcium, and phosphate in the blood. 3:24 Calcidiol also has a negative feedback on the parathired gland, so it inhibits 3:29 it because 3:29 if we have so much calcidiol, we don't need that much parathired hormone 3:36 anymore. 3:37 And then calcitrial also targets the GIT. 3:40 It stimulates the GIT to increase calcium and phosphate absorption. 3:47 Calcidiol also targets the kidneys itself. 3:50 So if we zoom into the functional units of the kidneys, these are the nephrons. 3:55 Here I am drawing one nephron. 3:57 The nephron is made up of the head, the proximal convoluted tubules, PCT, lup 4:02 of Henley, LOH, 4:04 convoluted tubule, DCT, and collecting ducts, CD. 4:09 So calcitrial actually targets the proximal convoluted tubules here to 4:15 stimulate the reabsorption 4:17 of calcium, thus increasing plasma calcium levels. 4:23 In this diagram, in the nephron, the parathired hormone also has an effect, but 4:28 it has an 4:28 effect on the distal convoluted tubules. 4:31 It stimulates the cells in the distal convoluted tubules to reabsorb calcium as 4:37 well, thereby 4:38 increasing plasma calcium levels. 4:43 So now I hope that all made sense. 4:45 Now let's go back to calcidiol and calcitrial, calcitrial being the active form 4:50 of vitamin 4:50 D. But where do these things come from? 4:54 Well actually the 25 hydroxy vitamin D3 or calcidiol comes in the liver. 5:00 But the whole process actually originates in the skin. 5:04 In the skin, we have a chemical just there, a cholesterol there known as 70 5:10 hydroxy cholesterol. 5:11 And when the sun, the sun's UV rays hits this, it actually converts 70 hydroxy 5:16 cholesterol 5:17 to vitamin D3, cholocalciferol. 5:21 And this all occurs in the skin. 5:23 Cholocalciferol then travels to the liver, where it gets converted by the liver 5:28 enzymes 5:29 to 25 hydroxy vitamin D3 or calcidiol. 5:33 And then this calcidiol is what moves into the kidneys. 5:37 And in the kidneys calcidiol as we know, gets converted by one alpha hydroxyl 5:41 ase. 5:42 So I hope that all made sense. 5:45 So essentially when we look back at the three important hormones, vitamin D, 5:49 its main goal 5:50 is to increase plasma calcium levels. 5:53 Our thyroid hormone, its main goal is to increase calcium plasma levels as well 5:59 . 5:59 Now whereas calcitonin does the opposite, it will aim to decrease plasma 6:03 calcium levels. 6:05 So we can say that if there is for example an increase in plasma calcium levels 6:10 , this 6:11 will stimulate the thyroid gland. 6:14 And it will stimulate the thyroid gland to produce calcitonin. 6:18 Calcitonin essentially has the opposite effects of parathyroid hormone. 6:23 So calcitonin's goal is to decrease plasma calcium levels when we have an 6:27 increase of 6:28 it. 6:30 But I think calcitonin does not have that big of a role, much of a role in the 6:36 human body 6:37 as comparison, it does have a role but not as significant as parathyroid 6:43 hormone. 6:44 So I hope you understood the main goal, the main roles of the three important 6:48 hormones 6:48 in calcium and phosphate regulation. 6:51 But now it is important to look into a bit more detail at how parathyroid 6:56 hormone elicits 6:57 its effects on the bone. 7:00 Because the bone as I mentioned earlier is the main reservoir for calcium, the 7:05 minerals. 7:06 So the bone are made up of two main cells that we will talk about. 7:10 These are osteoblasts which build bone and these are osteoclasts which break 7:17 down bone. 7:18 However, this osteoclast is not activated yet, so we call it a pre-Osteoclast. 7:24 And it is the active osteoclast that will re-resorb bone. 7:29 So it will break down bone which will allow calcium and phosphate to be 7:32 released in the 7:33 blood. 7:35 So here I'm drawing a bone again, a simplified diagram. 7:39 And on the outside we have the hard bone, also known as a compact bone where we 7:44 can find 7:44 collagen as well as minerals, and this is what bone is made up of essentially. 7:50 And then on the inner part we have soft bone. 7:52 But in this case, I think it's just good to know that it's just bone. 7:57 Okay, so now let's go back to the osteoblasts. 8:02 And because osteoblasts see have the main role in activating these osteoclasts, 8:08 even 8:09 though they have opposite roles. 8:11 So on osteoblasts we have a receptor, the parathired hormone receptor. 8:16 So when parathired hormone comes along, it will bind onto this receptor and it 8:20 will cause 8:21 and it will have three effects on the osteoblasts. 8:24 Firstly, it will cause osteoblasts to proliferate, second it will stimulate the 8:31 expression of 8:33 rank ligand on the osteoblasts, thirdly, the parathired hormone will cause oste 8:40 oblasts 8:41 to stop making osteoportidurin. 8:45 Now osteoportidurin, also known as OPG, normally inhibits basically the 8:50 activity of 8:51 rank ligand binding onto another receptor. 8:56 So basically parathired hormone inhibits this process. 8:59 So it doesn't want OPG to have an effect. 9:02 Now on pre-osteoclast, the pre-osteoclast expresses a receptor called the rank 9:09 receptor. 9:10 So essentially what happens is the rank ligand being expressed on osteoblasts 9:14 will bind 9:15 onto the rank on the pre-osteoclast. 9:18 And when this occurs and when it's not inhibited by OPG, the rank ligand rank 9:24 complex will 9:25 cause the osteoclasts to proliferate and differentiate. 9:31 There's another chemical which sort of stimulates this whole process as well, 9:36 where on the osteoclast 9:38 we have a receptor CFMS. 9:41 And the chemical that I'm talking about is macrophage colony stimulating factor 9:47 or MCSF. 9:49 And when MCSF binds onto this receptor, it will stimulate the osteoclast to 9:53 proliferate 9:54 and to differentiate. 9:57 So if either of these things occur, the pre-osteoclast will then become an 10:02 active osteoclast and 10:04 it will become multinucleated, osteoclasts are actually big things, it's much 10:09 bigger 10:09 than osteoblasts. 10:12 And it is a type of macrophage, that's why macrophage colony stimulating factor 10:17 . 10:17 So here we have osteoclasts which will release some form of acid and when it 10:21 releases acid 10:22 it will basically eat away on the bone and this will cause bone resorption. 10:27 So it will allow the minerals to leave out of the bone. 10:31 And these minerals that I'm talking about are calcium and phosphate. 10:35 So it's essentially parathyroid hormone stimulates this whole process, thereby 10:41 allowing osteoclasts 10:42 to become activated and to basically release calcium and phosphate from the 10:47 bone by eating 10:48 it up. 10:51 And just to recap, osteoblasts have the opposite effect in that their main goal 10:55 is to build 10:56 bone so they are the ones that release collagen as well as some minerals. 11:05 So I hope you enjoyed this video on endocrinology, calcium and phosphate 11:09 regulation. 11:09 We looked at three main hormones, vitamin D, active form, calcitrile, parathy 11:14 roid hormone 11:15 as well as calcitonin. 11:18 Thank you for watching.