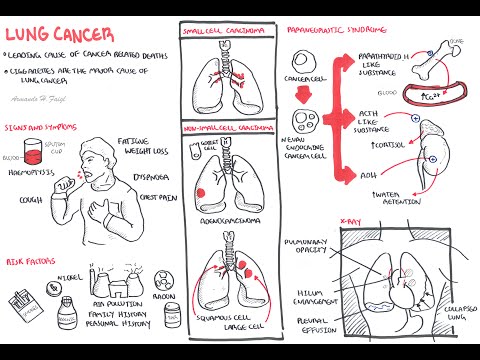
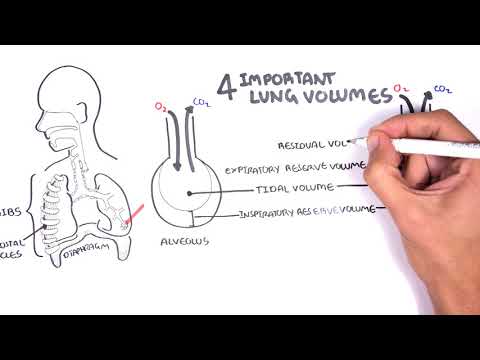
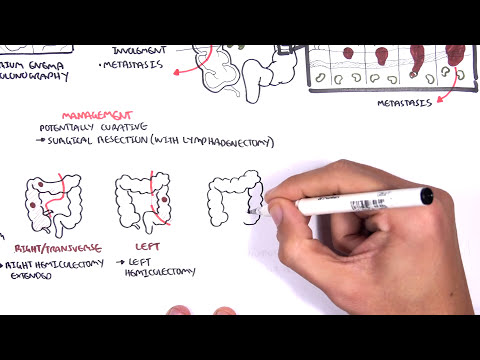
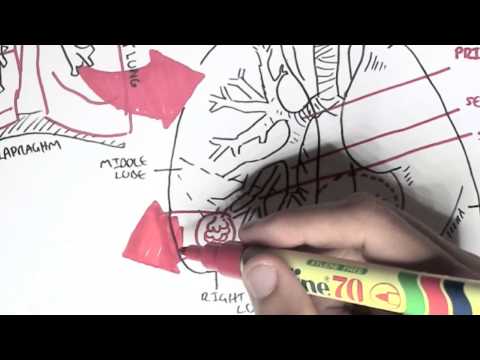
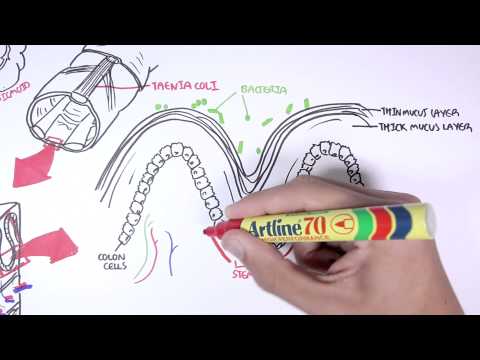
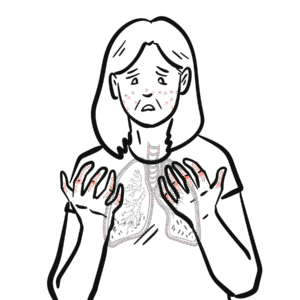
0:00 Lung cancer is the leading cause of cancer-related deaths, and it has a poor 0:10 prognosis. 0:11 In this video, we will focus on lung carcinomas. 0:17 So let us look at the different types of lung carcinomas, and it can be divided 0:21 into two 0:22 broad types, small cell carcinoma and non-small cell carcinoma. 0:28 Let us focus on small cell carcinoma. 0:32 Small cell carcinoma represents about 15% of lung carcinomas. 0:38 More than 60% actually present already with metastases. 0:44 The prognosis of small cell lung carcinoma is poor. 0:50 The tumor tends to grow proximally close to the highlum and involves neuroend 0:54 ocrine 0:55 cells in the area, because neuroendocrine cells are involved in this type of 1:00 cancer, 1:00 they undergo mutations, which allow them to produce hormones like hormone-like 1:06 substances 1:07 that they should not be able to produce. 1:10 And so as a result, they release these hormones, and it triggers a phenomenon 1:16 known as the 1:16 para-neoplastic syndrome, which we will talk about later on. 1:21 Small cell carcinomas represent the majority of lung carcinomas, 85%. 1:29 Non-small cell carcinoma is further divided into three types. 1:33 Idenocarcinoma is the most common type of non-small cell carcinoma. 1:38 Idenocarcinomas make up 38% of lung carcinomas. 1:43 These types of cancers tend to occur in the peripheral lung tissue, so away 1:47 from the highlum 1:49 and involves glands within the lung. 1:52 Squamous cell carcinoma is the other type of non-small cell carcinoma and makes 1:56 up about 1:56 20% of lung carcinoma cases, making it the second most prevalent type of lung 2:03 carcinoma. 2:05 These types of cancer tend to occur close to the main bronchus and can cause 2:10 obstruction 2:10 of the airways. 2:12 They are called squamous because the epithelial cells that line the airway 2:16 become mutated 2:17 and change from columnar, cuboidal to squamous, and essentially, dysplasia 2:25 cancer. 2:26 The last type of non-small cell carcinoma is large cell carcinoma, which make 2:32 up about 2:33 5% of lung carcinomas, so it is the least common. 2:38 Large cell carcinoma rapidly grows, like the small cell carcinoma, and can 2:43 present in the 2:44 periphery or the peripheral lung tissue or the proximal lung tissue. 2:49 Those were the different types of lung carcinomas. 2:53 Let us look at the signs and symptoms of patients that present with lung carcin 3:00 omas. 3:01 Not everyone presents with the same signs and symptoms, but the most common 3:08 signs and 3:09 symptoms include cough, weight loss, hematosis, dysnea, and chest pain. 3:17 There are many risk factors for lung cancer. 3:20 Major ones are smoking, radon, air pollution, arsenic, tar, asbestos, nickel, 3:27 as well as 3:28 those family and genetic factors. 3:32 Now with cancer, because it is a growth, it can cause some problems to 3:38 surrounding tissues 3:39 surrounding organs, so let us look at some media-stinal involvement of lung 3:46 cancer. 3:47 Let us zoom into the mediastinum, where we can find the heart, the lungs, and 3:55 all these 3:56 other structures, including the ribs. 4:00 Let us zoom into this first rib area and learn a bit of anatomy, so here is the 4:07 sternum and 4:08 the first rib. 4:10 Now, going over the first rib are some important structures, including the sub 4:16 clavian artery 4:17 and vein, and the brachial plexus, the nerves that innervate the upper limb. 4:26 Why are we talking about these structures? 4:29 Because these structures have to do with the pathophysiology, or the 4:34 complications associated 4:35 with lung carcinomas, lung cancers. 4:38 See, the mediastinal involvement of lung cancer include pan-coast tumor growth, 4:43 which is growth 4:44 on the apical lung surface, so on the top, which can block part of the brachial 4:50 plexus. 4:51 Depending on how much the brachial plexus is affected, it can cause shoulder, 4:57 arm pain, 4:58 weakness, and atrophy on the ipsilateral side, so on the same side. 5:04 Apical lung tumors can also block the sympathetic nerve fiber around this area, 5:09 causing what's 5:10 known clinically as hornet syndrome. 5:15 Another mediastinal involvement is pleural effusion, which causes dyspnea as 5:18 well as chest pain. 5:21 There can also be heart involvement causing pericardial effusion. 5:28 Another important structure that can be affected is the superior vena cava, 5:33 which when blocked 5:34 can cause the vena cava syndrome. 5:37 Forget about the inferior vena cava here, this is a complete mistake, ignore 5:42 that. 5:43 So it's superior vena cava. 5:46 So those were some mediastinal involvement associated with lung cancer growth. 5:55 Let us look at the airway involvement now. 5:57 So the airways of the lungs are the bronchi and the bronchioles, right, before 6:01 it terminates 6:02 at the alveoli. 6:03 Well, cancer can cause airway obstruction as it impedes air flow. 6:08 Airway obstruction leads to dyspnea. 6:10 When there is airway obstruction or irritation, this actually sends sensory 6:15 information to the 6:16 brain and triggers the cough reflex. 6:19 That is why in presentation we have dyspnea and cough. 6:23 The patients have dyspnea and cough. 6:26 Cancer or tumor also stimulates angiogenesis, which is blood vessel growth. 6:31 However, angiogenesis forms leaky and tortuous vessels, which when ruptures can 6:37 lead to what 6:38 leads to hematosis. 6:40 Okay, let us zoom into the blood vessels. 6:44 The blood vessels contain your red blood cells, platelets, and white blood 6:48 cells, right? 6:49 In lung cancer, we see some blood involvement, mainly anemia, which leads to 6:54 fatigue and 6:55 dyspnea, leukocytosis in 15% of cases, thrombocytosis in 15% of cases, and 7:02 hypercoagulable disorders. 7:07 Lung tumours can metastasise, and they do. 7:11 When it metastasises, it goes to the heart, and then the heart will pump the 7:17 tumor, the 7:18 growth, the cancer, either up to the brain and upper limbs or down to the 7:25 abdomen area. 7:27 Common sites of lung metastasies include the brain, the liver, the adrenal 7:34 glands, and 7:35 the bone. 7:38 Metastatic metastatic sites are commonly asymptomatic. 7:44 Now looking back to the different types of lung cancer, remember the neuroend 7:49 ocrine cells 7:50 that begin secreting hormones in the small cell carcinoma? 7:55 Well, it leads to the phenomenon called the paranere plastic syndrome. 8:00 Let us learn a bit more about what this encompasses. 8:03 So the paranere plastic syndrome typically occurs in small cell lung cancer as 8:09 well as 8:09 squamous cell carcinomas. 8:13 Paranere plastic syndrome are syndromes that occur not related to invasion, 8:19 obstruction, 8:20 or metastasies of primary tumour, and the paranere plastic syndrome include the 8:26 following. 8:29 Rectopic Cushing Syndrome, where the hormone released by cancer cells, 8:33 stimulate the adrenal 8:34 glands to produce cortisol. 8:39 We also have antidiuretic-like substance, which stimulates up, secreted by the 8:43 neuroendocrine 8:44 cells, which stimulate the kidneys to retain water. 8:49 These neuroendocrine cells also produce a parathyroid hormone-like substance, 8:53 which 8:53 stimulates the bone to break down its minerals and release calcium into plasma, 8:59 increasing 8:59 blood calcium levels, resulting in hypercalcemia. 9:03 Paranere plastic syndrome also includes the hyperpulmonary osteoarthropathy 9:09 leading to 9:09 clubbing and periosteal proliferation of the tubular bone. 9:13 And lastly, inflammatory myopathies can result from lung cancer, which leads to 9:20 the muscle 9:21 weakness, and so that is why we see signs of finger weakness upon examination 9:28 of patients 9:29 with lung cancer. 9:32 Okay, so that was essentially the pathophysiology. 9:34 Now, lung tumors can be staged. 9:37 We will not look at the staging in this video, because all I will do is regurg 9:42 itate what 9:43 I wrote. 9:44 But I will draw it out, out quickly, and leave you to interpret it yourselves. 9:56 Next, let us look at some investigations we would do if we were suspicious of 10:06 lung cancer. 10:08 So lung involvement, we always do a chest x-ray to rule out other differentials 10:14 . 10:15 Common and clinical findings on x-ray for lung cancer include a high-lem enlarg 10:19 ement, 10:20 pulmonary opacity, which represents the tumor, three rib bone lesions, pleural 10:29 effusion, 10:30 and also lung collapse. 10:34 Another investigation which is critical for lung cancer is CT scan, and should 10:40 be performed 10:41 early to determine stage and management of the cancer. 10:52 Not only CT scans, but biopsy are to be performed, which include the bronchosc 10:57 opy, which is where 10:58 the primary lung tumor is visualized, and sample is taken using the instrument. 11:08 You can also perform a CT-guided fine needle biopsy, which is a more reliable 11:13 way to obtain 11:14 a histological diagnosis. 11:17 A needle aspiration, this is where a needle is inserted in the lump on the lung 11:23 , or lymph 11:24 node to see for lymph node involvement. 11:28 Another form of investigation for biopsy is the ophthalrocosentesis, which is 11:33 where fluid 11:34 is collected from the pleural cavity, and this is used for sampling. 11:41 Again our numbers three, four, five, and six are used for biopsy to stage the 11:48 tumor so 11:49 that appropriate management can be taken. 11:56 And so management is the next topic we will talk about. 11:59 So these are one surgical treatment, which is the most important. 12:06 Surgical treatment is for the removal of tumor of the lung tumor cancer for 12:11 stages one and 12:12 stages two. 12:14 After surgery, or if surgery cannot be performed, there is also radiotherapy 12:19 and chemotherapy, 12:21 as well as laser therapy and stenting. 12:24 Geotherapy is less effective than surgery, however radiotherapy is used in 12:31 combination 12:32 with chemotherapy for stages three. 12:36 Chemotherapy increases survival up to one year. 12:40 Nausea and vomiting are side effects. 12:43 These side effects are managed best by the five HT3 receptor antagonists, 12:47 because these 12:48 drugs will target the chemoreceptor trigger zone, thus preventing the vomiting 12:53 nausea 12:53 associated symptom. 12:56 Laser therapy and stenting can also be done. 12:59 Airway obstruction from the tumor growth causing serious symptoms can be 13:03 managed using laser 13:05 treatment and stenting. 13:07 So essentially the obstruction of the airway, you basically remove it so air 13:13 flow can return 13:14 as normal. 13:16 I hope you enjoyed this video on lung cancer, thank you for watching. 13:23 .