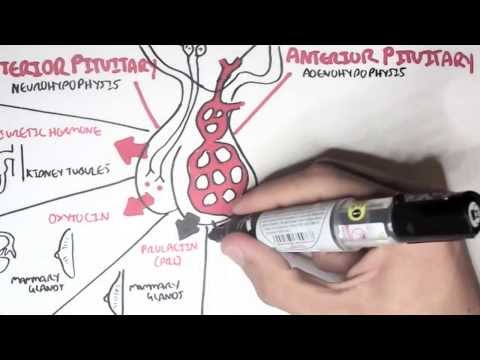
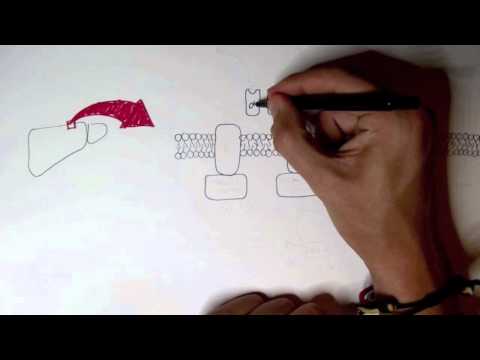
0:00 Hello, in this video, we're going to talk about syndrome of inappropriate anti- 0:11 diaryotic 0:11 hormones secretion, also known as SIADH. 0:16 The hypothalamus is a region of the brain involved in coordinating the physi 0:20 ologic responses 0:21 of different organs that together maintain homeostasis. 0:26 The hypothalamus have neurons running towards the posterior pituitary, which 0:30 produces neuropeptides, 0:32 and will release them into circulation. 0:35 ADH, also known as arginine vasopressin, is one of the neuropeptides which are 0:39 released 0:40 into circulation. 0:42 An increase in serum osmolarity, or a decrease in blood volume, will stimulate 0:48 the hypothalamus 0:50 to produce anti-diaryotic hormone, also known as ADH. 0:55 ADH is produced by magnus cellular neurons, which will carry and then release 1:01 them from 1:02 the posterior pituitary gland into systemic circulation. 1:08 So what does ADH do? 1:10 Well, ADH's main effect is to increase water reabsorption from the kidney. 1:17 How do they do this? 1:19 The kidneys are made up of their functional units called nephrons, and here is 1:23 one nephron 1:23 as an example. 1:26 Afferent arterial will bring blood to the head of the nephron, forming what's 1:30 known 1:30 as the glomerulus. 1:32 The glomerulus will filter blood through and into the nephron tubules. 1:36 It enters the first part of the nephron called the proximal-convlated tubule. 1:40 The proximal-convlated tubule have channels on it, called acroporin-1 channels, 1:47 which 1:47 reabsorb water. 1:49 The acroporin-1 channels are responsible for reabsorbing 90% of water that is 1:55 filtered 1:55 through the nephron. 1:57 The filtrate in the tubule remains that will continue along the tubule through 2:04 the loop 2:04 of Henley, the distal-convated tubule, and the collecting ducts. 2:09 The remaining 10% of water is actually reabsorbed in the collecting duct and 2:14 the distal-convated 2:15 tubule, and is primarily driven by the hormone ADH. 2:21 ADH increases expression of acroporin-2 channels, which results in water re 2:31 absorption. 2:33 Despite being responsible for only 10% of water reabsorption from the nephron, 2:38 this goes a 2:39 long way. 2:40 Let's take a closer look at how ADH actually reabsorbs water. 2:45 There are cells which line the collecting ducts called principal cells. 2:49 Principal cells have all these acroporin-2 channels in this endosome, the cyto 2:55 zone, ready 2:56 to be expressed by the cell membrane. 3:00 ADH will travel by blood and travel to the nephron. 3:04 ADH will bind onto ADH receptors on the basal surface, so the bottom part of 3:10 the principal 3:12 cells. 3:13 And this will stimulate then the expression of acroporin-2 channels on the ap 3:17 ical surface 3:18 of the principal cells. 3:20 These channels will increase the reabsorption of water from the nephron tubule. 3:25 Water enters the cell, the water then gets reabsorbed into circulation. 3:31 The increase in water reabsorption increases blood volume and also decreases 3:38 serum osmolarity. 3:40 SIADH is syndrome of inappropriate secretion of ADH, resulting in a lot of ADH 3:56 in the blood 3:57 in the serum and also increases the ADH activity. 4:03 Causes of syndrome of inappropriate anti-diarrhy common secretion include 4:07 trauma to the brain 4:08 or the pituitary area, central nervous system disorders or infections such as 4:14 meningitis, 4:16 as well as ectopic ADH production, such as from lung cancer or even non-neopl 4:23 astic ADH, 4:24 such as from respiratory infections. 4:29 Regardless of the cause, the pathophysiology of SIADH begins with uncontrolled 4:36 secretion 4:36 of ADH. 4:39 When this happens, you retain more water. 4:43 You increase blood volume and you will decrease serum osmolarity. 4:49 Pro-osmolarity is usually a result of dilution and secretion of sodium from the 5:01 body. 5:02 What contributes to water retention is also if you drink more in response to a 5:07 decrease 5:07 in blood volume or an increase in serum osmolarity. 5:13 The syndrome of inappropriate anti-diarrhy common secretion continues and you 5:19 get an 5:19 increase in blood volume for a while and after a while, you will actually cause 5:24 stretching 5:25 of the heart muscle walls in the atrium and in the ventricles and when this 5:29 happens, 5:30 the heart produces naturitic peptides, ANP and BNP as a response. 5:37 Now ANP and BNP inhibits renin release and activity through a few mechanisms. 5:46 Regardless, the end result is a decrease in activity of the renin angiotensin- 5:51 aldosterone 5:52 system and because of this you decrease angiotensin to function and also ald 5:59 osterone function. 6:01 A reduction in aldosterone and an increase in ANP and BNP, the naturitic pept 6:08 ides, will 6:09 promote naturisis. Naturisis is the excretion of sodium in the urine. 6:18 Naturisis results in a decrease in blood volume and also a decrease in serum o 6:25 smolarity. 6:27 A decrease in blood volume means it will stimulate ADH release and promote its 6:31 activity again, 6:32 which is already present in SIDH. With so much SIDH remember, there will be an 6:40 increase 6:40 in blood volume, which really means that you are increasing the GFR, the amount 6:45 of blood 6:45 going into the kidneys and as a response, this will also cause a decrease in 6:50 renin production. 6:52 Decrease in renin means you have decrease in the renin angiotensin-aldosterone 6:57 system, 6:58 which means that you will essentially promote naturisis, the excretion of 7:02 sodium from the 7:03 body and with that water will follow. When you measure urine in people with SID 7:11 H, 7:11 there will be high amounts of sodium in urine. The urine tends to be 7:19 concentrated and when 7:19 you measure someone's blood, there will be low levels of sodium, termed hypon 7:27 aturemia. 7:27 This cycle continues. With more blood volume and decrease in serum osmolarity 7:34 over time 7:35 through an unknown mechanism, the kidneys will eventually adapt. 7:40 When the kidneys begin adapting, they will try to do something interesting. 7:48 The number of aqua-pouring channels decrease at the apical surface of principal 7:53 cells, 7:53 in order essentially to negate the increased amounts of ADH present. 8:00 This means that the kidneys will learn not to re-absorb water and so you will 8:05 have diorisis 8:06 and naturisis, peeing out water as well as sodium. And this will occur even if 8:12 you consume 8:13 salt and even if you ingest water. The urine in SIDH does not necessarily have 8:20 to be concentrated. 8:22 And this is one of the reasons why in patients with SIDH, the new steady state 8:28 is a u-valimic 8:29 state, not fluid overloaded but also not dehydrated, thanks to the mechanism we 8:35 discussed 8:36 just before. Remember, SIDH is characterized by hyponaturemia, an increase in 8:43 urine sodium 8:44 excretion, and u-valimia. Also remember clinically patients with SIDH are u-val 8:51 imic, despite 8:52 retaining water. The reason being, the body learns to excrete water eventually, 8:58 maintaining 8:58 this u-valimic state. The important clinical symptoms and signs of SIDH are 9:04 related to 9:04 the low sodium levels in the blood. Now low sodium levels can be acute or 9:10 chronic. Acute 9:11 is defined by hyponaturemia occurring less than 48 hours. Severe hyponaturemia 9:17 is defined 9:18 as serum sodium of about 120 millimoles per liter or less. And this is usually 9:24 when the 9:24 symptoms of hyponaturemia come up. Acute hyponaturemia is dangerous because it 9:30 can cause cerebral 9:31 edema, neurogenic pulmonary edema, seizures and even coma. The mechanism of ed 9:38 ema in acute 9:39 hyponaturemia can be explained here. Let's look at cerebral edema, the 9:43 dangerous complication 9:45 of acute hyponaturemia. You can imagine here is the brain and it's neuron and 9:51 here is the 9:51 circulation. In the circulation you have water and low sodium levels. In the 9:58 brain you have 9:58 adequate electrolyte levels including sodium and potassium. Now if you have 10:03 suddenly low 10:04 sodium in circulation, according to the osmotic gradient principle, water will 10:09 move to the 10:09 area with more solutes and so will develop edema rapidly. In chronic hyponatur 10:16 emia you 10:16 don't get cerebral edema because of cerebral adaptation. This is where because 10:21 of time 10:22 electrolytes from the brain are able to distribute, equalizing the electrolytes 10:28 in circulation 10:29 and in the brain. And so sodium and potassium for example can move into 10:34 circulation and 10:35 this allows water to equalize more safely. Chronic hyponaturemia is 10:42 characterized by 10:43 nonspecific signs and symptoms such as headache, nausea, vomiting and seizures. 10:48 The other signs 10:49 and symptoms of SIADH will depend on the cause of the SIADH. Causes of SIADH 11:02 include trauma, 11:04 surgery, CNS infections and stroke which affect the hypothalamic/paturity axis, 11:12 increasing 11:12 the production of ADH. Medications also somehow increase production or the 11:18 effect of ADH. 11:19 These medications can be remembered with the acronym CARDISH, chemotherapy, 11:25 antidepressants, 11:26 recreational drugs, diuretics, inhibitors such as ACE inhibitors and SSRIs, 11:33 sulfenoluria 11:34 and H is for hormones such as dismopressin. Another cause for SIADH are the mal 11:42 ignancies 11:43 which cause ectopic production of ADH. Common examples include small cell 11:50 carcinoma of the 11:50 lung and pancreatic cancer. Pulmonary disease such as pneumonia can increase AD 11:57 H production 11:58 somehow and there are nephrogenic causes mainly the mutation in the aquaportin 12:04 type 2 channels 12:05 in the distal collecting ducts which will increase the retention of water. Nef 12:14 rogenic 12:14 SIADH is aquaportin 2 mutation which causes aquaportin 2 to remain open 12:21 resulting in 12:22 water retention. Diagnosing SIADH requires a set criteria and ruling out other 12:29 causes 12:30 of hyponaturmia. So let's look at some criteria to diagnose SIADH. 1. You need 12:37 to have hyponaturmia 12:39 with a normal extracellular fluid state so a uvelemic state. 2. Urine osmol 12:46 ality needs 12:46 to be higher than plasma osmolality. The urine sodium needs to be greater than 12:51 20 millimoles 12:52 palleta and you need to roulette other causes of hyponaturmia. This includes 12:57 making sure 12:58 the patient is not on diuretics. Patients have to have normal function of 13:03 kidneys, thyroid 13:04 and adrenal glands namely the production of cortisol. Management of SIADH is 13:11 relatively 13:11 similar. 1. Treat symptomatic acute hyponaturmia quickly as this can be left 13:19 threatening. Treat 13:20 chronic hyponaturmia slowly. The reason for this is to prevent what's called 13:25 central 13:25 pontine mylonosis which we will talk about later. It's important to treat the 13:33 main cause 13:33 that could be leading to the low sodium and SIADH. 2. Restrict fluid intake 500 13:41 ml to 13:42 1 liter a day is good. This will lead to a reduction in blood volume, an 13:48 increase in 13:48 testosterone and so will hopefully increase sodium retention. 3. Administration 13:54 of hypertonic 13:55 saline if patients are symptomatic in any way. This has to be given slowly. 14:02 Hypertonic 14:04 saline has sodium in it, the fluid will also increase plasma volume. Fruzomite 14:11 can also 14:12 be given with patients who have features of mild fluid overload. Fruzomite 14:19 works at the 14:19 ascending loop of Henley, inhibiting a tri-porter. Fruzomite causes an increase 14:25 in water, sodium, 14:27 chloride and potassium excretion. It's important to consider to replace the 14:32 potassium chloride 14:33 that's being excreted and you can give potassium chloride in the hypertonic 14:38 saline solution. 14:39 Finally, the meclocyclin can be given. The meclocyclin is mainly used in 14:46 chronic hyponatremia. The 14:49 meclocyclin inhibits the renal action of antidiaradic hormone by inhibiting its 14:55 binding 14:56 onto the ADH receptors. Finally, rapid correction of hyponatremia can lead to 15:04 central pontine 15:05 melanosis, which leads me to the complications of rapid correction of hyponat 15:17 remia. So imagine 15:19 you are using medications, fluids to increase serum sodium rapidly. This means 15:24 you suddenly 15:25 get all the sodium in circulation. Remember, water follows sodium. So what you 15:31 get is water 15:32 from the brain, for example, escaping into circulation because of the osmotic 15:38 gradient. 15:38 This causes shriveling and shrinkage, you can say, of the brain parenchima. It 15:43 is termed 15:44 central pontine melanosis because when first described, it was found in the p 15:52 ons and what 15:53 was seen was damaged to the myelin sheath. Central pontine melanosis is 15:59 characterized 15:59 by a progressive development of spastic quadripleces, suitable with a palsy and 16:05 emotional liability.