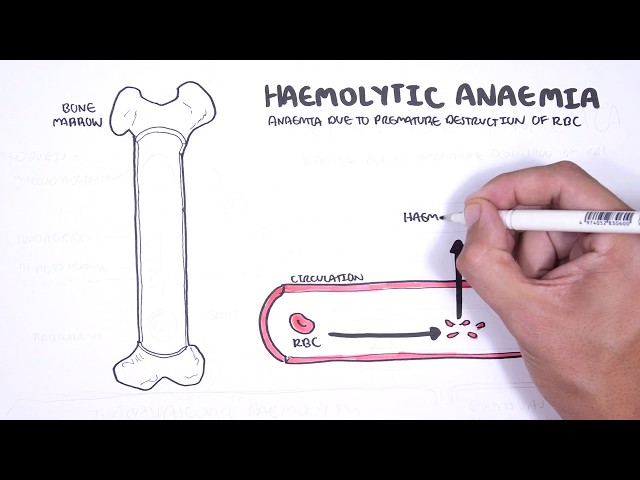
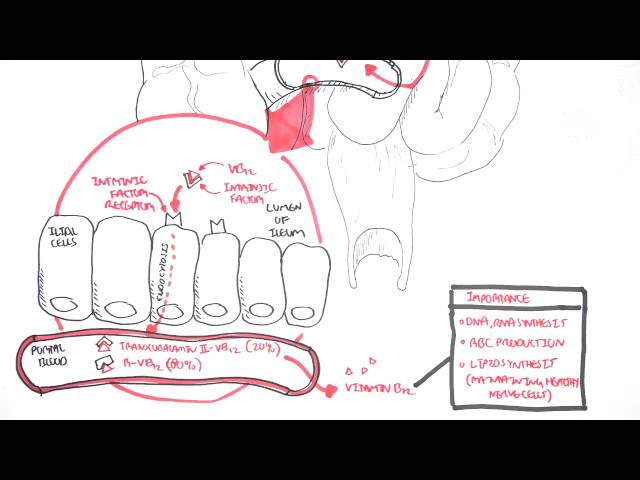
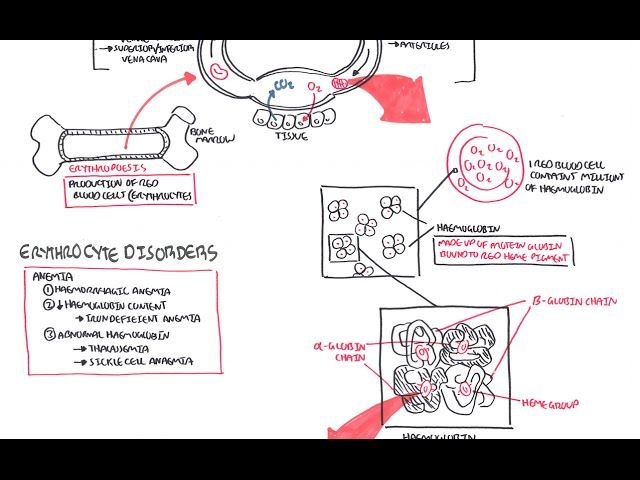
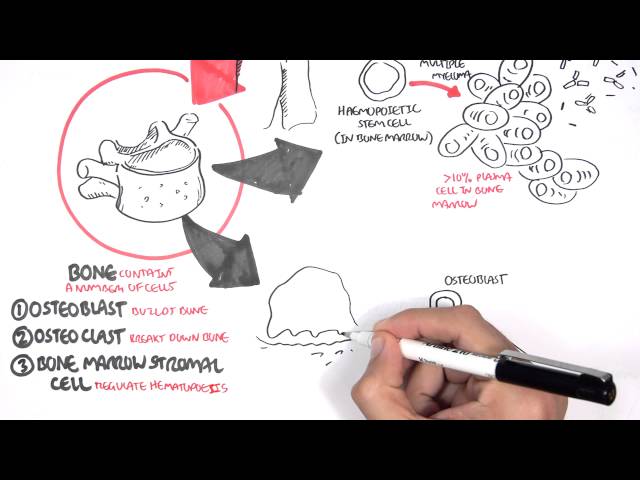
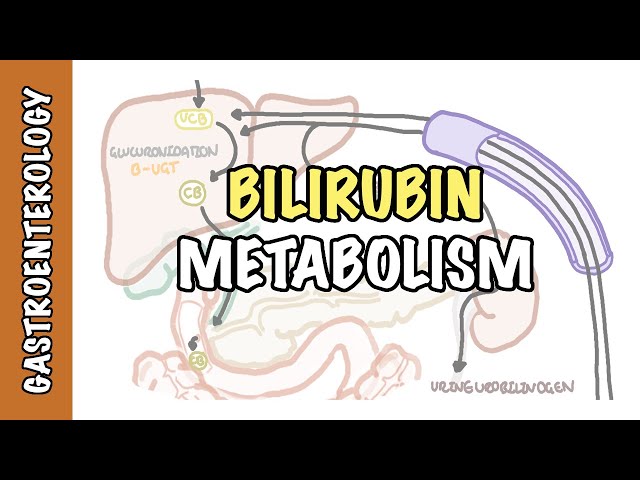
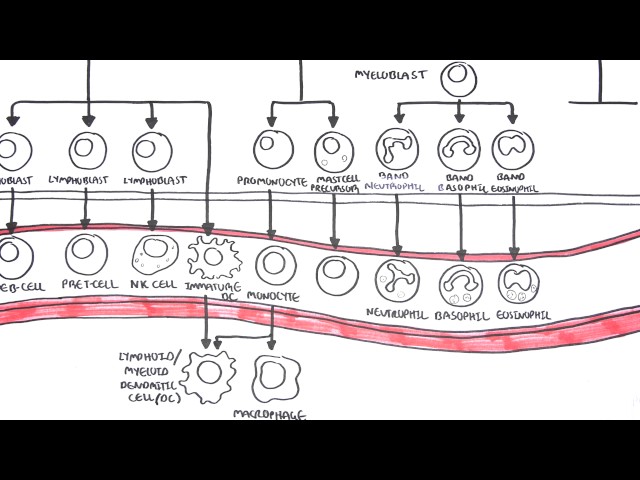
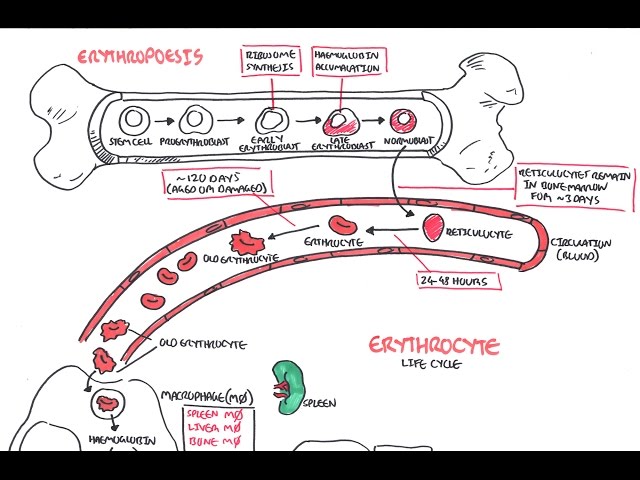
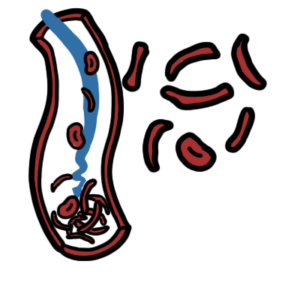
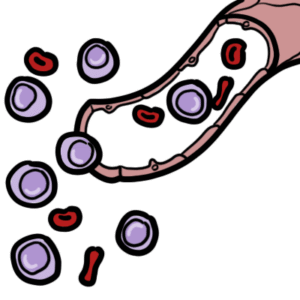
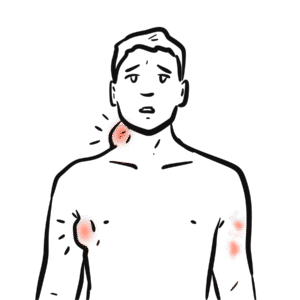
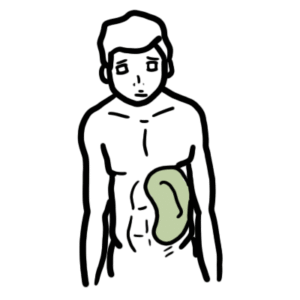
0:00 Hello, in this video we're going to talk about anemia. 0:09 Anemia can be rigorously defined as a reduced absolute number of circulating 0:13 red blood cells, 0:14 in practice a low hemoglobin concentration, or a low hematocrit is most widely 0:20 accepted 0:21 definition for anemia. 0:23 So anemia can be defined as hemoglobin level of less than 120 grams per liter 0:29 in females 0:29 and less than 140 grams per liter in males. 0:34 Red blood cells are the cells that carry oxygen around our body. 0:37 They contain hemoglobin molecules, millions of them, which help bind oxygen. 0:45 Red blood cells also contain many types of enzymes, including lactate dehyd 0:50 rogenase. 0:51 Red blood cells are important in carrying oxygen and carbon dioxide, as well as 0:55 maintaining 0:56 pH of the blood. 1:00 Red blood cells arise from myeloid progenitor cells in the bone marrow. 1:04 Erythropoasis is the process of erythrocyte production. 1:09 Myeloid progenitor cells become reticulocytes first, and this path is 1:13 stimulated by hormones, 1:15 including erythropoietin. 1:17 Erythropoietin is a true endocrine hormone produced in the kidney by cells that 1:24 sense 1:24 adequacy of tissue oxygenation relative to the individual's metabolic activity. 1:30 Other hormones that facilitate in red blood cell production are the thyroid 1:35 hormones and 1:36 androgen. 1:38 Reticulocytes are the premature erythrocytes, so the premature red blood cells. 1:43 A cell still capable of limited amount of hemoglobin and protein synthesis. 1:49 The reticular sites enter the bloodstream three days later, and matures to 1:54 become the 1:54 red blood cell as we know it. 1:57 The mature red blood cell circulates for around 120 days, after which time it 2:02 is removed 2:03 from the circulation by the reticular endothelial system. 2:07 The reticular endothelial system includes the spleen and the liver, where mac 2:12 rophages and 2:12 monocytes will eat up and clear up these old red blood cells, but also clear up 2:19 the 2:19 abnormal red blood cells. 2:22 When performing a full blood count or a completed blood count, looking at hem 2:26 oglobin is the 2:27 first step to diagnosing anemia. 2:30 But how does one categorize anemia? 2:32 Well, one way is to look at the full blood count first and look at the mean 2:37 corpuscular 2:37 volume. 2:38 The mean corpuscular volume, abbreviated MCV, is the average size of the person 2:45 's red blood 2:46 cell. 2:47 Therefore, one way to categorize anemia is using the mean corpuscular volume. 2:53 You can have microcytic anemia less than 80 femto-liters, normalcytic anemia 2:59 between 2:59 80 to 100 femto-liters, and then macrocytic anemia, which is greater than 100 3:05 femto-liters, 3:06 and these are essentially the sizes of the red blood cell. 3:11 Causes of microcytic anemia include iron deficiency, chronic inflammatory 3:16 disease, and 3:17 thalassemia. 3:20 Investigations that should be performed in this context include iron studies, 3:24 and then 3:24 calculating the Menser Index, which is helpful in differentiating iron 3:29 deficiency anemia 3:31 from beta thalassemia. 3:33 When someone with anemia has a normal MCV, a reticular site count should be 3:40 performed. 3:41 Remember, the reticular sites are the premature red blood cells that are still 3:45 in the bone 3:46 marrow. 3:47 The reticular site count can be either high or it can be low. 3:54 If it's a high reticular site count, this can mean a hemolytic anemia or blood 3:59 loss, because 4:00 the body is trying to compensate and produce more reticular sites to replenish 4:05 the red blood 4:05 cells that are lost. 4:08 If the reticular site counts are low, this could signify a bone marrow disorder 4:13 , such 4:13 as aplastic anemia, because the bone marrow is unable to produce adequate 4:19 amount of red 4:20 blood cell. 4:23 When the hemoglobin is low, and the MCV is high, this signifies macrocytic an 4:29 emia. 4:29 A blood film should be performed to differentiate between megaloblastic or non 4:34 megaloblastic 4:35 macrocytic anemia. 4:38 Megaloblastic anemia is basically where on the blood film, you can see large, 4:43 immature 4:44 red blood cells called megaloblast. 4:47 Also you can potentially see hypersegmented neutrophils. 4:51 These findings on the blood film signify someone that has vitamin B12 4:55 deficiency, folate deficiency 4:57 or drug toxicity side effect from methotrexate for example. 5:03 If the blood film only shows large, mature red blood cells, this is non megalob 5:08 lastic 5:09 and can signify alcohol abuse, hypothyroidism and pregnancy as potential causes 5:14 of the anemia. 5:17 Anemia can be categorized based on the size using the mean corpuscular volume 5:20 as we have 5:21 talked about. 5:22 Another way to categorize anemia is by the mechanism of anemia. 5:26 We can easily categorize anemia in this way by looking at the red blood cell 5:32 life cycle. 5:33 A cause of anemia can be from a decreased production, so reduced erythropoasis. 5:39 Examples include bone marrow disorders such as aplastic anemia, because 5:43 remember red blood 5:44 cells are formed from the bone marrow. 5:47 Chronic kidney disease can also cause anemia, because when you have chronic 5:51 kidney disease 5:52 or kidney failure you're reducing erythropoate in production and therefore 5:57 reducing erythropoasis. 5:58 Hypothyroidism, because remember thyroid hormones play a role in stimulating 6:03 erythropoasis. 6:04 Vitamin B12 deficiency and iron deficiency can also lead to anemia because 6:10 these are 6:10 the substances needed in order to produce good functioning red blood cells. 6:18 Chronic inflammatory disease which basically causes a form of iron deficiency 6:23 but also 6:23 is thought to reduce the lifespan of the red blood cell. 6:27 Another mechanism which leads to anemia is through blood loss, and this can be 6:31 gastrointestinal 6:32 blood loss, someone going through heavy periods, trauma, accidents, motor 6:37 vehicle accidents 6:39 for example leading to blood loss. 6:42 Another mechanism leading to anemia is through the increase in red blood cell 6:48 destruction. 6:49 Increased destruction of red blood cells really means hemolysis and this can be 6:53 further divided 6:54 into intravascular hemolysis which means destruction of red blood cells in 6:59 their vasculature and 7:01 extravascular hemolysis which means destruction of red blood cells outside the 7:05 vasculature typically 7:06 in the reticular endothelial system we talked about. 7:11 Examples of intravascular hemolysis include disseminated intravascular coagul 7:16 opathy, thrombocytopenic, 7:18 thrombotic thrombocytopenic purpera, hemolytic euremic syndrome and mechanical 7:25 heart valve 7:26 where the red blood cells dive from sheer stress of a mechanical valve in the 7:31 heart. 7:31 Extravascular hemolysis occurs when there is increased destruction of red blood 7:34 cells 7:34 typically through the reticular endothelial system. 7:39 Examples include hypersplinism, inherited hemolytic anemia disorder such as 7:44 sickle cell anemia 7:45 and hereditary spherocytosis, acquired hemolytic anemia such as in malaria. 7:53 When a red blood cell gets destroyed they release a number of things which are 7:58 important 7:58 things to measure to see whether someone has hemolytic anemia. 8:03 Red blood cell destruction causes the release of lactate dehydrogenase. 8:08 Red blood cells is made up of a lot of hemoglobin, millions of hemoglobin 8:12 molecules. 8:12 When hemoglobin is broken down you get globin which is a protein, unconjugated 8:17 bilirubin 8:18 and iron. 8:19 Usually the body is able to clear all these byproducts of red blood cell 8:23 destruction up. 8:24 However, in hemolysis you have overwhelming red blood cell destruction and as a 8:29 result 8:30 you can also have free hemoglobin in circulation. 8:34 Luckily, there are molecules which float around our body which help clear up 8:37 these free hemoglobin 8:39 molecules. 8:40 These are called haptoglobins. 8:42 Therefore, blood tests to order in someone with suspected hemolytic anemia 8:47 include measuring 8:49 their lactate dehydrogenase which should be elevated, the reticular side count 8:54 which should 8:54 be elevated because the body is trying to compensate by producing more red 8:59 blood cells. 9:00 There should be an increase in bilirubin which also means the person can 9:03 present with jaundice 9:05 and finally low haptoglobin levels because they are bound to free hemoglobin 9:11 and are 9:12 being cleared up by the body. 9:14 Red blood cells as mentioned are very important in carrying oxygen to the body 9:19 providing energy 9:20 for the cells and therefore with low amounts of red blood cells you can have 9:26 signs of basically 9:27 fatigue and low energy. 9:29 A person with anemia can therefore present with pala, conjunctiva pala, fatigue 9:35 , scleral 9:36 ictrus if you are thinking hemolysis, bony tendonus if you are thinking bone 9:41 marrow disorders, 9:43 lymph adenopathy if you are thinking infection or malignancy, dysnia and hepat 9:49 osplatomically 9:51 if you are thinking hemolysis or bone marrow disease. 9:54 I hope you enjoyed this video on the overview of anemia. 9:59 To learn more about other hematological disorders please check out the playlist 10:03 .