Overview
Dizziness is a broad term used by patient to describe a range of sensations that include vertigo, presyncope, imbalance sensation and light-headedness. Vertigo describes a spinning sensation but sometimes a sensation of falling or pitching. Presyncope is a result of decrease global perfusion to the brain resulting in near fainting sensation (syncope is a transient loss of consciousness due to decrease perfusion to brain). Sensation of imbalance describes dysequilibrium and is usually of a central cause such as the brain and brain stem. Patients and with mental health can also describe a sensation of light-headedness often as a result hyperventilation or emotion stress.
| Remember Vertigo is not only caused by pathology in the vestibular system but can also be caused by cerebellar and neurodegenerative disorders. |
| Categories of dizziness | Pathophysiology | Aetiology |
| Vertigo (Spinning sensation) | Vestribular pathology | Vestibular neuritis Labyrinthitis Meniere's disease |
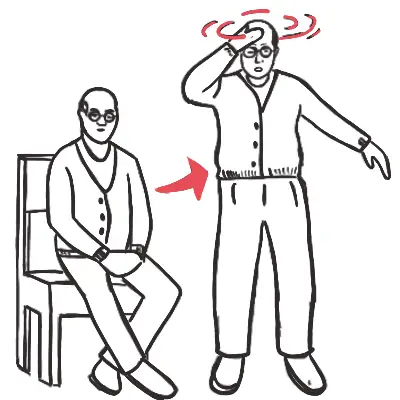
| Presyncope (fainting sensation) | Reduced cerebral perfusion | Neurocardiogenic syncope Situational syncope Carotid sensitivity Postural hypotension |
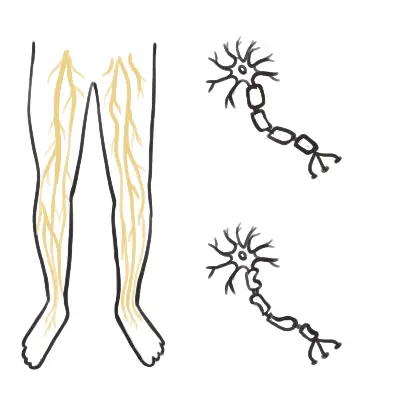
| Dysequilibrium (imbalance sensation) | Gait disorder | Myelopathy Peripheral neuropathy Parkinson's disease |
| Light-headedness (sensation of disconnection from the environment) | Psychological disorder | Anxiety Depression |
Vertigo
Vertigo is sensation of false movement, generally described as rotation or spinning sensation. It is caused by asymmetry of neural activity between the right and left vestibular nuclei located in the brainstem. Bilateral damage does not cause vertigo. Essential to determine if the vertigo is central or peripheral since cerebellar infarction/haemorrhage can present as vertigo and can be life-threatening.
| Remember Vertigo describes a spinning sensation but sometimes a sensation of falling or pitching. Presyncope is a result of decrease global perfusion to the brain resulting in near fainting sensation. |
Peripheral causes of vertigo (suggest inner ear pathology)
- Benign paroxysmal positional vertigo
- Vestibular neuritis
- Meniere's disease
- Otosclerosis
- Cholesteatoma
- Perilymph fistula
- Aminoglycoside ototoxicity
Central causes of vertigo
- Vestibular migraine
- Multiple sclerosis
- Tumour
- Cerebellar Stroke - especially involving the vertebrobasilar artery
| Peripheral features | Central features |
| Vertigo improves with visual fixation | Vertigo does not improve with visual fixation |
| Hearing loss | Ataxia |
| Tinnitus | Visual field loss |
| Aural fullness | Diplopia |
| Positive impulse test | Limb weakness |
| Unidirectional horizontal nystagmus | Dysarthria |
| Dysphagia | |
| Nystagmus all directions (especially vertical nystagmus and horizontal nystagmus that changes direction with gaze) |
Differential diagnosis of acute vertigo
- Acute vestibular neuritis
- Labyrinth infarction
- Perilymph fistula
- Brainstem and cerebellar infarction
Differential Diagnosis of recurrent acute vertigo
- Benign paroxysmal positional vertigo
- Meniere disease
- Migraine
- Vestibular schwannoma (slowly progressive)
Approach to someone with vertigo
History
- Unilateral or bilateral
- Acute or chronic or progressive
- Spontaneous vertigo (present when head is stationary) or motion induced vertigo
- Head movement likely BPPV
- Standing up likely orthostatic hypotension → dizziness
- Spontaneous or positional
- Duration of each vertigo spell?
- Signs and symptoms of stroke (dysarthria, limb weakness, blurry vision) - central cause
- Associated Otological symptoms
- Hearing loss, aural pressure with tinnitus likely Meniere's Disease
- Hearing loss, nausea and vomiting +/- tinnitus likely labyrinthitis or vestibular neuritis
- Hearing loss can also be associated with viral infection and ototoxic medications
- Hearing loss and otitis media can be associated with granulomatosis with polyangiitis
| Seconds | Minutes-Hours | Days |
| Benign paroxysmal positional vertigo | Meniere's Disease | Brainstem or cerebellar infarction |
| Perilymph fistula (trauma) | Vestibular migraine | Labyrinthitis |
| TIA | Multiple sclerosis | |
| Vestibular neuritis |
- Preceding history
- History of viral infection likely labyrinthitis or vestibular neuritis
- History of travelling prior to onset of symptoms associated with mal de debarquement syndrome
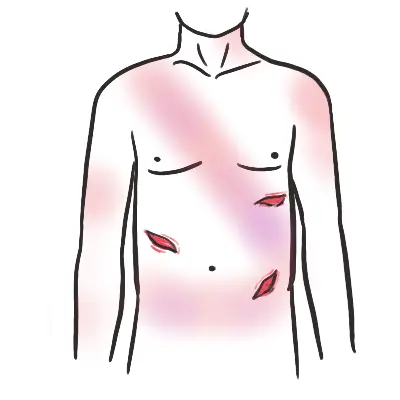
- History of trauma likely perilymph fistula
- Other associated signs and symptoms
- Past medical history
- History of migraines may have vestibular migraine
- Cancer history with dizziness, nausea and vomiting, ataxia, dysarthria, dysphagia and nystagmus can indicate paraneoplastic cerebellar degeneration
- Medications
- Aminoglycosides leading to ototoxicity
- Antihypertensive agents can cause presyncope → dizziness
- Alcohol intoxication
- Family History
- Migraines
- Friedreich's ataxia
- Risk factors for cardiovascular disease → cerebellar stroke
Examination - check cerebellar signs too
- Titubation - slow frequency bobbing of head and trunk
- Head tilt - patient tilts the head to the unaffected side to minimise diplopia.
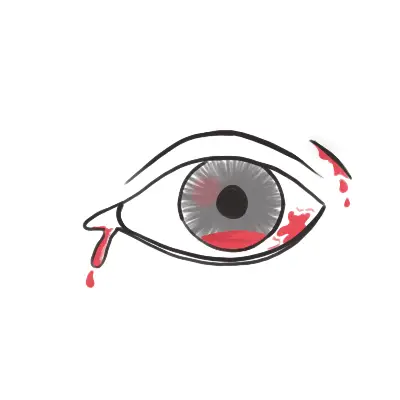
- Horner's syndrome - seen in brainstem strokes which accompany brainstem strokes
- Gait - ?ataxia
- Eye movements
- Looking at a fixed object - look for nystagmus or saccadic intrusions
- Peripheral vertigo - Horizontal nystagmus that beats away from the lesioned side
- Central vertigo - bidirectional, vertical or torsional vertigo
- Pursuit - ability to follow a smoothly moving target
- Saccades - ability to look back and forth accurately between two targets (
- Looking at a fixed object - look for nystagmus or saccadic intrusions
- Ear examination
- Fistula test - checking for evidence of perilymphatic fistula but also can be positive in cholesteotoma
- Head impulse test (to differentiate vestibular neuritis and central causes of vertigo)
- HINTS (horizontal head, impulse test, typical peripheral nystagmus, absence of skew deviation, and normal hearing)
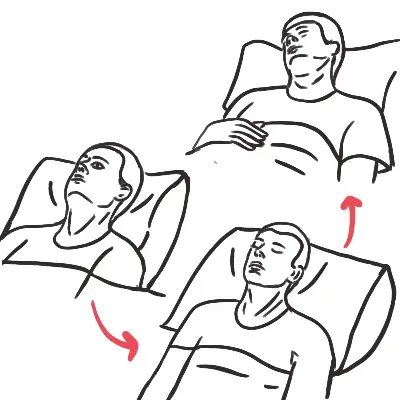
- Dix-Hallpike maneuver (testing for BPPV)
- Rhomberg's test
- Upright stance relies on vision, proprioception, and vestibulospinal contributions
- Distribution of any of the three can affect gait and stance.
- Unterberger test is performed by asking the patient to march in place with eyes closed for 30 seconds and noting any excessive turning to the side of vestibular impairment.
- Cranial nerve examination
- Upper and lower limb neurological examination
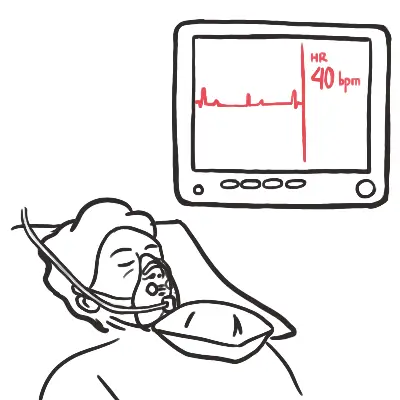
- Postural blood pressure and auscultations
| Remember Poor pursuit or inaccurate saccades usually indicate central pathology. |
Investigation
- ECG
- CT scan
- MRI scan
| Remember all patients suspected of central cause should get a CT and better MRI scan. |
Management
Depends on the cause of vertigo but can include:
- Physical therapy
- Repositioning maneuvers
- Vestibular rehabilitation
- Low sodium diet
- Antihistamines
- Benzodiazepines
- Anticholinergic
- SSRI