Notes »
clinical
» Nephrology
Acute Kidney Injury
Overview
Acute kidney injury (AKI) is the syndrome arising from a rapid fall in GFR (over hours to days). It is characterised by retention of both nitrogenous (including Urea and Creatinine) and non-nitrogenous waste products of metabolism, as well as disordered electrolyte, acid–base, and fluid homeostasis.
| Remember AKI is neither a diagnosis nor a disease. Rather, it is a clinical syndrome that is caused by, or complicates, a wide range of disorders. |
| Definition Acute Kidney Injury: Rapid reduction in kidney function over hours to days, as measured by serum urea and creatinine and leading to a failure to maintain fluid, electrolyte and acid-base homeostasis. Chronic Kidney Disease: Impaired renal function >3months based on abnormal structure or function, or GFR <60 for >3months. Oliguria: A urine output of <400ml/day may be the earlier sign of impaired renal function. |
Classification
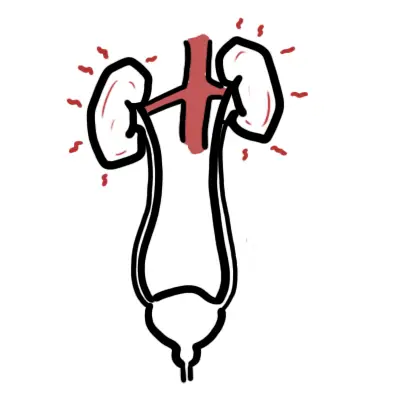
The aetiology of acute kidney injury can be simply divided into pre-renal, renal and post renal causes.
- Pre-renal - Sepsis and hypotension
- Severe sepsis
- Haemorrhage
- Dehydration
- Cardiac failure
- Liver failure
- Renovascular insult
- Intrarenal
- Toxicity
- Nephrotoxic drugs
- Iodinated radiological contrast
- Parenchymal kidney disease
- Glomerulonephritis
- Tubulointerstitial nephritis
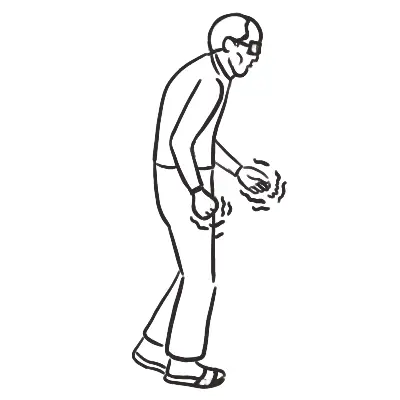
- Rhabdomyolysis
- Haemolytic uraemic syndrome
- Myeloma
- Malignant hypertension
- Toxicity
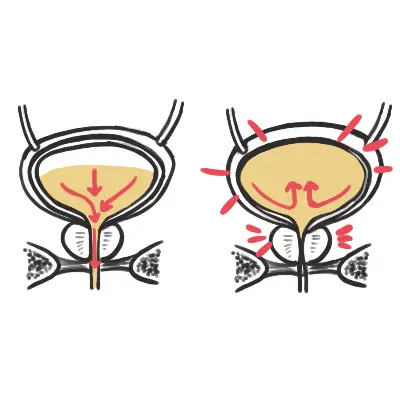
- Post renal Obstruction
- Bladder outflow
- Stones
- Tumour
- Surgical ligation of ureters
- Extrinsic compression (lymph nodes)
- Retroperitoneal fibrosis
Approach to Acute Kidney Injury
History
- Prerenal causes
- Vomiting, diarrhoea, polyuria
- Use of diuretics
- Dehydration
- Assess for comorbidities which may reduce renal perfusion - heart failure, shock
- Renal causes
- Diuretics and other nephrotoxins (NSAIDs, ARBs, ACEI)
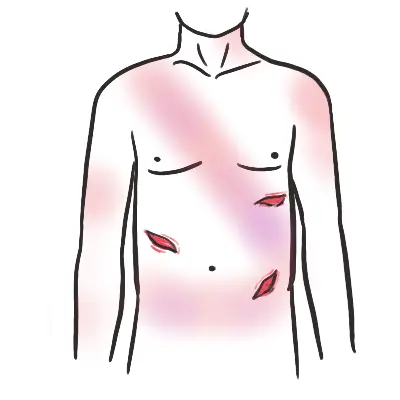
- Palpable purpura, pulmonary haemorrhage or sinusitis raises suspicion of systemic vasculitis with glomerulonepritis
- Polyarthralgia, rash suggests rheumatological cause such as SLE
- Recent injury, limb ischaemia suggest rhabdomyalsis
- Fevers night sweat and chills may suggest vasculitis or urine infection
- Postrenal obstruction
- Nocturia, hesitancy and urgency suggest prostate issues
- Severe flank pain with history of stones suggest nephrolithiasis
- Suprapubic discomfort may suggest urinary retention
- Other questions
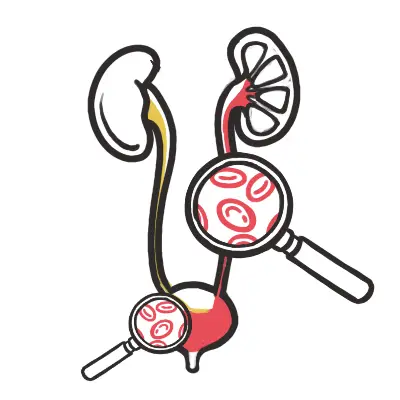
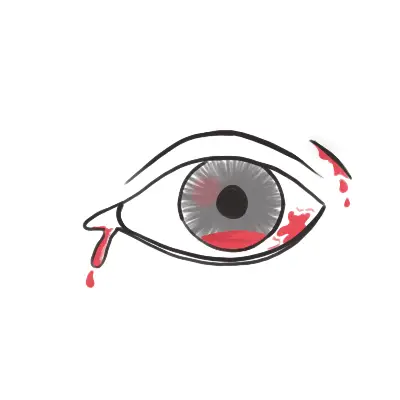
- Haematuria
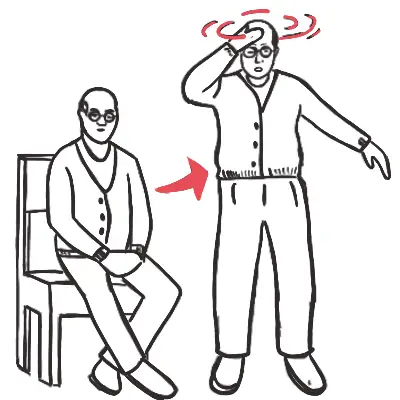
Examination
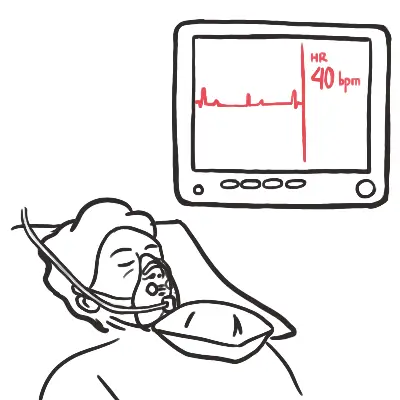
- Stable or unstable patient
- Vitals signs
- Catheter in situ? - Haematuria
- Urine output chart
- Assess fluid status - hypovolaemia, normovolemic or hypervolaemic
- Hypovolaemic - reduced skin turgor, dry mucus membranes
- Hypervolaemic - JVP elevated, peripheral oedema, pulmonary coarse inspiratory crackles (pulmonary oedema)
Bedside test
- Urine analysis
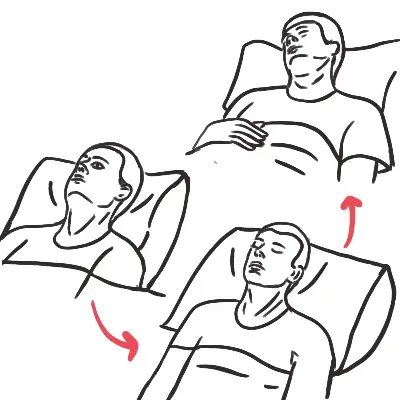
- Urine sediment examination and microscopy
- Urine that has been centrifuged to concentrate the substances in it at the bottom of a tube
Drawing for urine sediment examination....
Investigations
- FBC
- EUC
- LFT
- CMP
- Urine casts
- Urine albumin/creatinine ratio
- Urine protein/creatinine ratio