Overview Benign bone tumours account for 99% of cases. Malignant bone tumours account for 1% of cases.
Risk Factors
- Advanced age
- Existing cancer or history of cancer
- Paget’s disease
- Bone infarcts
- Irradiation
- Chronic osteomyelitis
- Metal prosthetic implants
History
- Pain
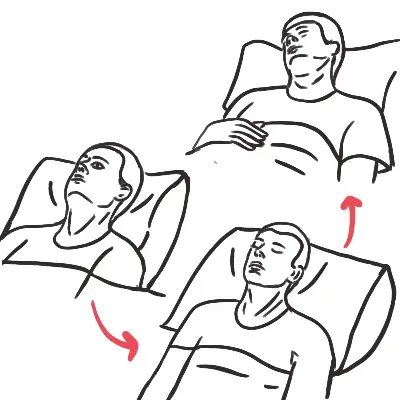
- Nocturnal pain
- Sudden severe pain – possible pathologic fracture
- Persistent pain, especially in children
- Pain which doesn’t respond to analgesia.
- Fracture in the absence of trauma (pathological fracture)
- Overlying erythema or ulceration
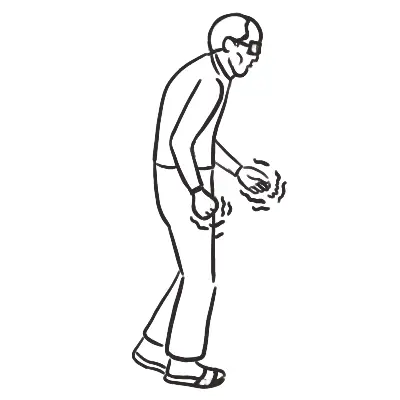
- Sign of Hypercalcaemia
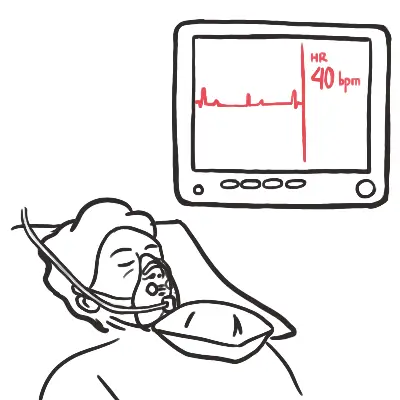
- Anaemia
- Neurological deficits – motor weakness, paralysis, sensory deficits, bowel and bladder dysfunction and ataxia. Suggestive of spinal cord compression. Indicative of neuropathic pain from nerve involvement or compression of the spinal cord
- Constitutional symptoms
- Weight loss
- Night sweats
- Loss of appetite
- Fever
| Remember Persistent deep pain not relieved with NSAIDs suggest malignant bone lump |
Examination
- Tenderness to palpation
- Warmth
- Overlying ulceration
- Ill-defined edge
Investigations
- X-ray
- FBC
- LFTS
- CRP/ESR
- Bone biopsy
| X-ray Findings | |
| Benign | Malignancy |
| Regular border | Irregular border |
| Smaller size | Larger size |
| - | Codman's Triangle |
| No sclerosis | Sclerosis |
| Homogenous | Heterogenousity |
| Non-invasive | Invasion |
Staging Investigations
- Radionucleotide scan
- CT Chest and ribs
Differential Diagnosis
Benign Bone Growth - Child or young adult without symptoms or with signs and symptoms of pain, swelling, decreased range of motion, deformity and pathological fracture.
- Osteoid osteoma (10% of benign bone growth)
- Osteochondroma (45% of benign bone growth)
- Chondroblastoma (2% of benign bone growth)
- Chondromyxoid fibroma
- Giant cell tumour
- Bone cysts
Malignant Bone Growth
- Osteosarcoma (Commonest primary bone sarcoma)
- Chondrosarcoma
- Ewing Sarcoma
- Metastatic bone lesions - skeletal metastases are typically multifocal but cancers from kidney and thyroid may be singular
| Side Note Malignant tumour: haemopoetic (common), metastatic bone tumour (very uncommon) and primary bone tumour (very uncommon) |
| Benign tumour | Clinical Features | Origin | Pathology | Radiology |
| Osteoid osteoma | ||||
| Osteochondroma | Symptomatic: Pain, decreased range of motion, deformity | Metaphysis of long bones and the ileal crest |
Benign cartilage-capped tumour attached to the underlying skeleton by a bony stalk.
|
Well-defined bony protuberance emerging from metaphysis. Bony spur points away from the joint |
| Chondroblastoma | Low grade joint pain (constant, unrelated to activity) Swelling/joint effusion | Epiphysis of the proximal long bones |
Composed of chondroblasts and chondroid matrix. There may be calcium deposition surrounding the chondroblasts causing a “chicken-wire calcification”. |
Well-demarcated radiolucent area. Sclerotic border |
| Chondromyxoid fibroma | Pain, swelling, pathological fracture | Metaphysis of the bones of the lower limb | Solid tumour of mixed cartilage, fibrous and myxomatous (connective) tissues. |
Eccentric, intramedullary, lobulated or bubbly lesion Sclerotic border Typically lucent |
| Giant cell tumour | Pain, swelling, decreased range of motion, deformity, pathological fracture | Epiphysis and diaphysis of long bones |
Macroscopic – fleshy, reddish tumour often containing cystic and haemorrhagic areas. Tumour may breach the cortex and extend into the soft tissues. There is little to no periosteal reaction. Microscopic – abundance of giant cells scattered on a background of stromal cells. |
Expansile, eccentrically-placed lytic area May extend into the joint No matrix calcification or periosteal new bone formation |
| Bone Cysts | Pain, swelling, decreased range of motion, deformity, pathological fracture | Metaphysis and diaphysis of long bones | Fluid filled lesions with a fibrous lining |
Well-marginated cystic lesions (radiolucent) i.e. “large bubble inside the bone”. No sclerosis Fallen leaf sign – where area of pathological fracture falls to the bottom of the cyst |
| Side note Giant cell tumours may metastasise to lungs but metastatic disease does not lead to patient death. |
Management
- NSAIDs
- Pathological fracture - treat
- Giant cell bone tumours and cystic bone tumours may need to be treated
- Excision, curettage +/- bone graft
- Radiotherapy
- Denosumab (RANKL Antibody)
| Malignant tumour | Clinical Features | Origin | Pathology | Radiology |
| Osteosarcoma |
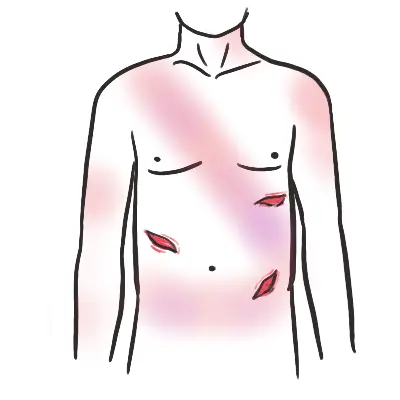
Localised pain – deep, dull, boring and relentless. Resistant to analgesia Progressively enlarging mass tender to palpation Inflamed overlying tissue Pathological fracture |
Metaphyseal region of long bones. 50% occur in knee (distal femur or proximal tibia). |
Highly malignant tumour which arises within the bone and spreads rapidly outwards to the periosteum and soft tissues. Osteosarcomas are bulky tumours which are gritty, grey-white and often contain areas of haemorrhage and cystic degeneration. |
Large destructive mixed lytic and blastic mass with infiltrative margins Codman triangle Sunburst appearance Poorly defined tumour margins |
| Chondrosarcoma |
Age: Adults >40yo Localised pain – deep, dull, boring and relentless. Resistant to analgesia Progressively enlarging mass tender to palpation Inflamed overlying tissue Pathological fracture |
Metaphysis of the proximal femur and humerus, pelvis, shoulder girdle and ribs. Can occur in any bone which develops in cartilage. |
Malignant tumour composed of hyaline or myxoid cartilage. Large bulky tumours with grey/white or translucent nodules of cartilage. Spotty calcification Cystic spaces Thickened cortex |
Mixed radiolucent and sclerotic appearance with mineralised chondroid matrix Thickened cortex No periosteal reaction |
| Ewing Sarcoma |
Painful enlarging masses Tender to palpation Localised swelling and erythema Systemic findings mimicking infection |
Diaphysis or metaphysis of bones of lower limb |
Arises in medullary cavity and invades the cortex, periosteum and soft tissue. Tumour is soft, tan-white and may contain areas of haemorrhage and necrosis. Characteristic periosteal reaction produces layers of reactive bone |
Destructive lytic tumour with permeative margins which extend into surrounding soft tissue. “Moth eaten” appearance “Onion peel” due to characteristic periosteal reaction |
| Remember Pain associated with malignant tumours: nocturnal pain, sudden severe pain – possible pathologic fracture, persistent pain, especially in children and pain which doesn’t respond to analgesia. |
| Side Note Codman triangle – triangular shadow between cortex and raised ends of periosteum due to tumour breaking through the cortex, lifting the periosteum and causing reactive periosteal bone formation. |
Treatment of Malignant Tumours - depending on severity and type on bone tumours
- Neoadjuvant chemotherapy
- Surgical resection
- Adjuvant chemotherapy
- Adjuvant radiotherapy