Overview
- Traumatic Brain Injury - classified as mild, moderate or severe based on GCS
- Concussion
- Cerebral contusion (intracerebral haemotoma)
- Subarachnoid Haemorrhage
- Subdural Haemorrhage
- Epidural Haemorrhage
- Diffuse axonal Injury
PAMD
- Preparation
- Assessment - Primary Survey
- Management
- Assessment - Secondary Survey
- Dislocation
Preparation

Assessment - Primary Survey - ABCDE
- Airway - Patent and Protected
- Foreign bodies
- Facial, mandibular, or tracheal/laryngeal fractures
| Remember If the patient is able to communicate verbally, the airway is usually patent |
- Breathing - Look, listen, feel
- Identify any life-threatening conditions affecting thorax
- Tension pneumothorax
- Flail Chest
| Side note Ventilation may be reduced for a number of reasons, (1) diaphragm fatigue, (2) Progressively ascending spinal cord damage from primary damage or secondary ascending spinal cord oedema encroaching on C3-C5, (3) These same segments may be involved from primary injury and diaphragm may be partially paralysed and (4) Consequence of co-existing chest trauma |
- Circulation
- HR, BP, Capillary refill, skin colour
- Look for signs of shock or unstable rhythm
- Hypotensive trauma victims should be considered as intravascularly volume depleted and bleeding until proven otherwise
- Disability
- GCS
- Pupils - equal and reactive
- Neurological examination - motor and sensory
- Suspect C-spine injury until ruled out
- Check for signs of ↑ICP - Cushing’s response (bradycardia, hypertension, irregular respirations)
| Remember A dilated pupil in an unconscious patient with head trauma is evidence of transtentorial herniation caused by downward pressure on the uncus and ipsilateral 3rd cranial nerve. |
- Exposure/Environment
- Increased risk of hyperthermia due to peripheral vasodilation
- Look for other injuries
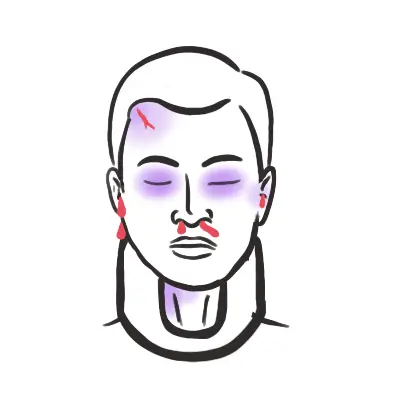
- Fractures - Basilar skull fracture?
- Scalp laceration
- Burns
| Warning Signs of Severe Head Injury |
| GCS <8 |
| Deteriorating GCS |
| Unequal pupils |
| Lateralizing signs |
| INVESTIGATIONS |
| Laboratory | Imaging |
| FBC | X-Ray - Neck, Thorax, Pelvis |
| EUC | Head CT scan (non-contrast) |
| Cross match | Ultrasound (FAST)? |
| Urinalysis | MRI - axonal injury is suspected |
| Pregnancy test | Angiogram? |
| Serum lactate | |
| Glucose | |
Management - The aim is to reduce secondary brain injury
- Airway - Patent and Protected
- Insertion of nasogastric tube important to minimise likelihood of aspiration
- Ensure oxygen delivery to brain through intubation and prevent hypercarbia
- Intubate if GCS < 9, patient is hypoxic, injury at or above C4'
- Oxygen!
| Remember Avoid secondary brain injury by preventing hypotension, hypoxia, fever, seizures and hyperglycaemia |
- Breathing - Look, listen, feel
- Consider diaphragm issues (injury at C3, C4, C5)
- Identify and treat life threatening chest injury
- In the absence of major airway obstruction and flail chest, the presence of paradoxical breathing is considered highly suggestive of cervical spine injury
- Circulation
- Look for signs of shock or unstable rhythm
- 2 large IV insertion
- If hypotensive - IV crystalloids, avoid albumin
- If seizure/risk - benzodiazepines, phenytoin, phenobarbital
- Disability
- GCS
- Pupils - equal and reactive
- Neurological examination - motor and sensory
- Spinal immobilisation until spinal cord or unstable vertebral injury has been excluded on physical examination and investigations (using nexus criteria as an example)
- If signs of increased intracranial pressure
- Calm (sedate) if risk for high airway pressures or agitation – paralyze if agitated
- Elevate head of bed
- Hyperventilate (100% O2) to a pCO2 of 30-35 mmHg
- Adequate BP to ensure good cerebral perfusion
- Mannitol 1g/kg infused rapidly (contraindicated in shock/renal failure
- Surgical - decompression, drainage
| Remember for raised ICP make sure to control perfusion, glucose, temperature and seizures |
- Exposure/Environment
- Increased risk of hyperthermia due to peripheral vasodilation
- Warm IV fluids
- Warm blankets
- Look for other injuries
| Remember Consult the neurosurgeon early and aggressively treat hypoxia, hypotension, herniation, and seizures to avoid secondary (preventable) injuries |
Early and Late signs of Head trauma
Assessment - Secondary Survey (Head to Toe) - Once patient is stabilised