POISONING
"All things are poison and nothing is without poison, only the dose permits something not to be poisonous.”
-Paracelsus
Overview
Children are curious and explore their world with all their senses, including taste. As a result, the home and its surroundings can be a dangerous place when poisonous substances are inadvertently ingested – every year millions of calls are made to poison control centres when this happens and thousands of children are admitted to emergency departments. Poisoning exposure typically causes minor symptoms in young children; death is a relatively rare occurrence. The rate of fatal poisoning is highest for children under one year, with another slight peak around 15 years. Common poisoning agents in high-income countries include pharmaceuticals, household products (e.g. bleach, cleaning agents), pesticides, poisonous plants and bites from insects and animals.
| Remember If a child has collapsed, stopped breathing, is fitting or is suffering an anaphylactic reaction, CALL an ambulance. Do not ring the Poisons Information Centre in an emergency. |
Risk Factors
- Young children are particularly susceptible to the ingestion of poisons, especially liquids, because they are very inquisitive, put most items in their mouths and are unaware of consequences.
- Adolescents, on the other hand, are more aware of the consequences of their actions but peer pressure and risktaking behaviour can lead them to misuse alcohol or illicit drugs, leading to a fatality rate higher than in younger children.
- Younger children are more susceptible to poisoning because of their smaller size and less well-developed physiology, particularly as the toxicity of most substances relates to dose per kilogram of bodyweight
- Lower sociceconomic status - severe poisoning
- Male
| Important Questions |
| What was indigested? |
| When was the substance indigested |
| How much was indigested? |
| What is the weight of the child? |
Management
- Call National Poison hotline for advice if needed
- Resuscitate
- Remove poison if indicated
- Activated charcoal - oral or nasogastric
- Gastric lavage
- Whole bowel irrigation
- Induced vomiting (not really used anymore)
- Administer antidote if one exists
| Poison | Antidote |
| Amphetamine | Esmolol, Labetalol |
| Benzodiazepine | Flumazenil |
| Beta-blocker | Glucagon, Isoprenaline, Adrenaline |
| Calcium Channel Blocker | Calcium chloride |
| Cyanide | Hydroxycobalamin with sodium thiosulfate |
| Digoxin | Digoxin Fab |
| Lead | If symptomatic Dimercaprol then calcium disodium edetate |
| Iron | Desferrioxamine |
| Opiates | Naloxone |
| Paracetamol | N-aceytlcysteine |
| Tetracycline Antidepressant | Sodium bicarbonate |
Ways to prevent poisoning:
- Store chemicals, medicines and cleaning products in a locked or child-resistant cupboard out of reach
- Store chemicals, medicines and cleaning products out of sight and reach of children
- Leave all chemicals, medicines and cleaning products in their original containers with clear labels.
- Medicines and other poisons should not be left unattended within children’s reach.
- Put all chemicals, medicines and cleaning products away immediately after buying or using them.
- Child-resistant lids or packaging.
- Store poisons away from food.
- Refer to medicines by their proper names. Do not confuse children by referring to medicines as lollies.
- Young children tend to imitate adults, so adults should avoid taking medicines with children present.
- Clean medicine cupboards out regularly. Take unwanted and out-of-date medicines to a pharmacy for disposal.
- Visitor’s bags may contain medicines. They should be kept well out of reach of children
ENVENOMATION
Overview
This section will mainly focus on snake bites. However, it is important to know that spider bites and jellyfish bites also exist. Venom from snakes may contain neurotoxins, procoagulants and rhadobmyolysins. Therefore, every snake bite should be regarded as potentially lethal.
| Definition Venom a poisonous substance secreted by animals such as snakes, spiders, and scorpions and typically injected into prey or aggressors by biting or stinging. Neurotoxins: a poison which acts on the nervous system. Procoagulants: inactive coagulation protein that becomes activated during the coagulation process to form a serine protease or cofactor and produce a fibrin clot. Rhadobmyolysins: substances which cause delayed destruction of skeletal muscle fibers. |
Signs and symptoms
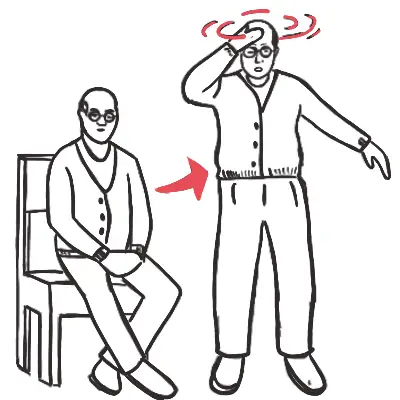
- Headache
- Nausea or vomiting
- Abdominal pain
- Blurred or double vision
- Slurring of speech
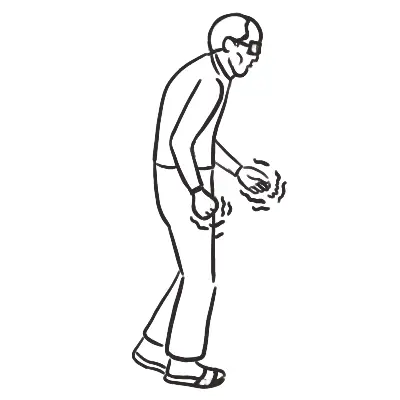
- Muscle weakness
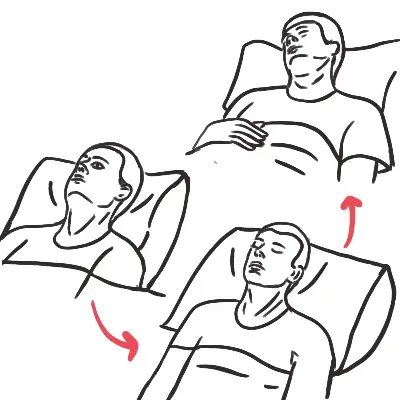
- Respiratory distress
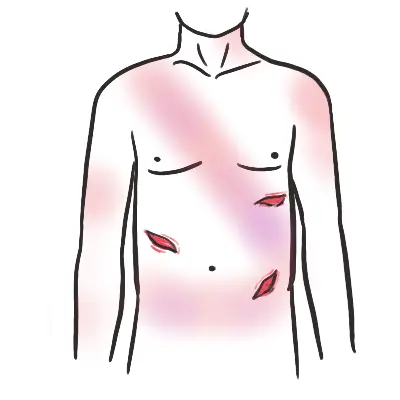
- Bleeding from the bite site or elsewhere
- Passing dark or red urine
- Local pain or swelling at bite
- Pain in lymph nodes draining the bite area
- Loss of consciousness and/or convulsions
Examination
- Evidence of a bite / multiple bites. Swab for venom but do not test.
- Evidence of venom movement (e.g. swollen or tender draining lymph nodes)
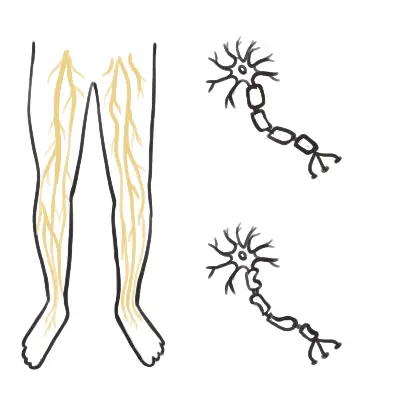
- Neurotoxic paralysis (ptosis, ophthalmoplegia, diplopia, dysarthria, limb weakness, respiratory distress)
Investigations
- Coagulation screen (INR, APTT, fibrinogen)
- Full Blood Count and blood film
- Creatinine Kinase
- EUC
- LDH
- LFT.
- Serial blood tests: INR, APTT, fibrinogen, CK, FBE, EUC
- hopefully clotting factors improve
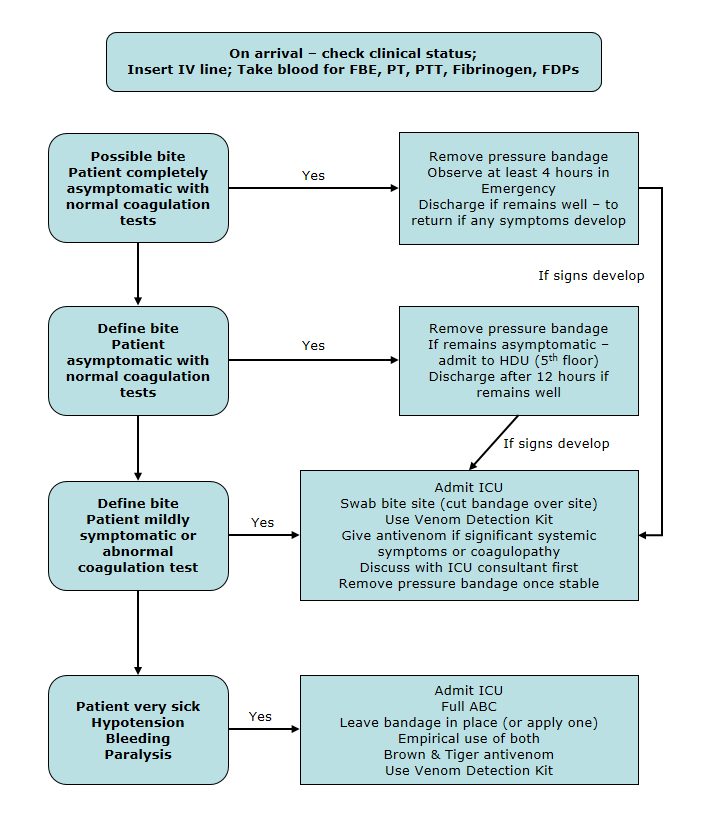
Management
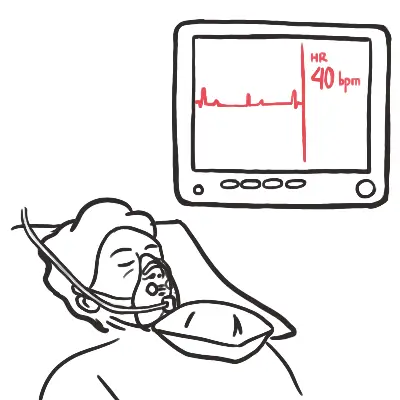
- Resuscitate and monitor closely
- First aid: Apply a pressure immobilisation bandage - immobilise joints either side of bite (use a splint), lay the patient down.
- The aim is to prevent lymphatic spread of venom, not to stop blood supply – make the bandage about as firm as you would use on a sprained ankle
- Antivenom if available and if indicated
- Giving antivenom should occur in consultation with a clinical toxicologist
- The choice of antivenom is based on the clinical syndrome and local geographical patterns of snake distribution
- There is a risk of anaphylaxis with antivenom administration – be prepared to treat
- Indication for antivenom
- Neurological signs and symptoms
- Significant coagulopathy
- History of unconsciousness, collapse, convulsions or cardiac arrest
| Remember DO NOT remove bandage until in a centre with full treatment facilities, including available anti-venom and access to laboratory testing. Do not wash or clean the bite site in any way. |
| Spider envenomation Spider bite is common, but most species cause minimal or no effects. Spider identification is problematic and the clinician is better off recognising the ‘toxindrome’ (ie. signs and symptoms associated with medically significant spider bite) than attempting to identify the spider responsible for the bite. The two main types of spider venom are: neurotoxic (affects the nervous system) and cytotoxic or necrotic (causing damage to tissue). Always consider spider bite in the differential diagnosis of unexplained autonomic and neurological dysfunction, particularly in children. In Australia, skin ulceration is more likely to be an infective, inflammatory or traumatic cause than a case of necrotising arachnidism. |